To the Editor,
Peritonitis continues to be one of the primary complications associated with peritoneal dialysis (PD), as well as being an important cause of morbidity, mortality, and technique failure.1
Cases of peritonitis produced by gram-negative bacteria are frequently more severe than others, implying a worse clinical prognosis and time on PD.2
This is fundamentally due to a number of intrinsic properties of gram-negative bacteria. Firstly, we should mention the high virulence inherent to gram-negative bacteria. Infections from Pseudomonas are the most common cause of severe cases of peritonitis, with high percentages of catheter loss and technique failure,3 and the same can be said for those caused by Escherichia coli and enterobacteria, with complete recovery of less than 60% of cases in some studies.4
A second important factor is the origin of the infection, since peritonitis caused by gram-negative bacteria is associated with contamination, infections of the outflow site, and intra-abdominal contamination. Finally, we should also point out the ability of gram-negative bacteria to protect themselves from antibiotic treatment thanks to a biofilm that forms in the catheter.1
In order to improve the results of treating these infections, a PD programme must have protocols for preventive care and the treatment of infectious complications, both peritonitis and infections related to the orifices and catheter. The patterns of infection at each centre should also be monitored (causative organisms and sensitivities); some guidelines recommend these reviews at least on an annual basis.5
At our institution, we performed a retrospective study in June 2008 of the cases of peritonitis that occurred between January 2006 and June 2008. In this period, it was observed that the resistance of gram-negative bacteria to ampicillin was increasing progressively, reaching 77% in 2008.6 Given these results, we decided to replace ampicillin and tobramycin with oral ciprofloxacin in our treatment protocol (ampicillin, tobramycin, vancomycin, and fluconazole), according to the recommendations of the Spanish Society of Nephrology [SEN, for its initials in Spanish] from 2004), since the sensitivity to this drug during the same time period was practically 100%.
Given the increase of cases of peritonitis from gram-negative bacteria, our institution also decided in February 2009 to change the protocol for treating the outflow orifices of peritoneal catheters to the application of topical gentamicin once per day. The primary objective of this modification was to prevent cases of peritonitis caused by gram-negative bacteria, avoiding the colonisation and infection by gram-negative bacteria of the peritoneal catheter outflow orifice.
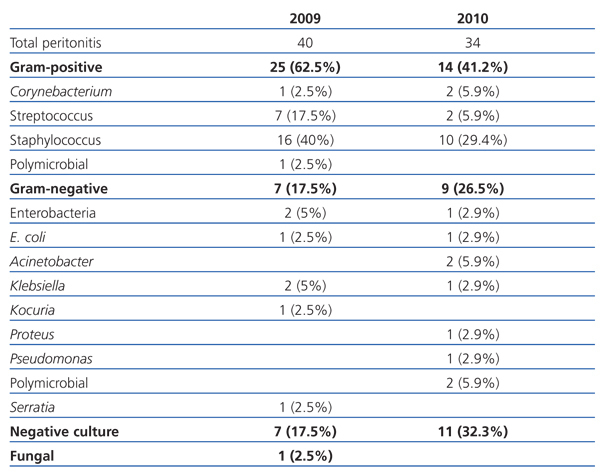
In this context, we carried out a retrospective analysis of all cases of peritonitis that occurred at our centre during 2009-2010 in order to evaluate the results of the changes mentioned to the treatment protocols. The micro-organisms responsible for the infections are compiled in Table 1.
In this study, we have focused on analysing the percentage of cases of peritonitis caused by gram-negative bacteria and the resistance these infections have to our empirical treatment protocol, comparing this data from the 2007-2008 study, which were from before the protocols were modified. We also calculated and compared ratios of peritonitis/patient and year.
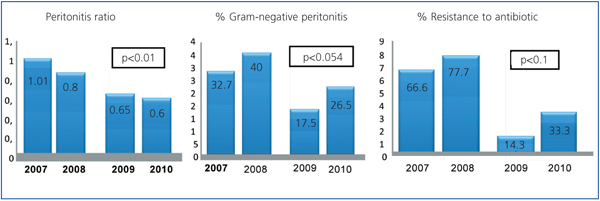
As shown in Figure 1, the results have been favourable since the changes in treatment protocols. Cases of peritonitis caused by gram-negative bacteria decreased by 17.5% in 2009 and 26.5% in 2010, and the resistance of these bacteria to ciprofloxacin decreased by 14.3% and 33.3%, respectively.
The ratio of cases of peritonitis/patient and year were 0.65 in 2009 and 0.6 in 2010, which is an improvement over the results from 2007 and 2008 (1.01 and 0.86, respectively).
Another result that highlights the new treatment in caring for the outflow orifice is that the same micro-organism was encountered both in the outflow orifice and from cultures of the peritoneal fluid in only 7 cases, and 100% of these were gram-positive bacteria.
In our opinion, these data support the idea that performing periodical reviews of treatment protocols and sensitivities to medication at each centre is a very important tool, both in the prevention and treatment of infectious complications of PD.
Conflicts of interest
The authors have no conflicts of interest to declare.
Table 1. Micro-organisms responsible for cases of peritonitis in 2009 and 2010
Figure 1. Description of the ratio of peritonitis/patients and year, percentage of peritonitis due to gram-negative bacteria, and resistance to antibiotic treatment. Comparison of the two-year period of 2007-2009 and 2009-2010