To the Editor,
Chronic kidney disease (CKD) is a common, treatable health issue that is well-known around the world. Although it is difficult to evaluate the repercussions that the various approximations to structuring the disease in recent years have had: a) classification of CKD according to the NKF-KDOQI 20021; b) consensus from the MDRD2 for estimating glomerular filtration rate (eGFR), and/or c) amplification of the use of albumin/creatinine ratios (ACR),3 their importance has been, without a doubt, very substantial, especially in non-nephrological fields.
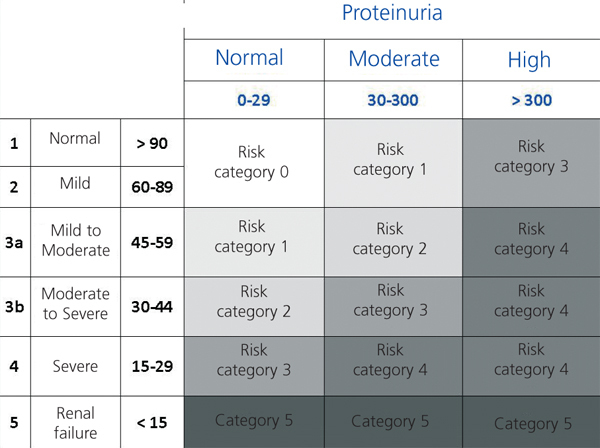
However, nothing is perfect, and several studies have demonstrated that proteinuria should be considered as an independent risk factor, both for the progression of CKD and mortality. As such, it would be logical to include this measure as a parameter used for stratifying patients with this disease. In this sense, the Kidney Disease: Improving Global Outcomes (KDIGO) has promoted several initiatives.4,5 Tonelli, et al6 presented their proposal for a new classification system based on risk categories, including proteinuria and eGFR, comparing it to the KDOQI-2002 in terms of referrals to nephrological consultations. In the accompanying editorial, Levey, et al5 refer to another similar classification, but one that adds more categories of proteinuria (KDIGO-2009 proposal) (Figure 1).
Recently, in the yearly meeting of the GRUPERVA in Granada, we presented the proposals of Levey5 and Tonelli6 as “the promising future in store for us,” primarily from a non-nephrological point of view, and we analysed their application in our field of medicine.
We used paired measurements (M) of glucohaemoglobin A1c (HbA1C) and fasting blood glucose levels (FBG) from our health area between September 2009 and February 2010 that were derived from primary care (PC) and hospital care (HC) settings. We assumed that the majority of measurements were taken from diabetic or pre-diabetic patients, which would give greater weight to the prognostic value of proteinuria.
First we sought to explore whether, as the guidelines indicate, these measurements were accompanied by a kidney profile (eGFR and ACR), and secondly, we evaluated the influence of classifying according to the KDOQI-20021 or Tonelli, 20116 systems (we opted for this method since it was more simple).
We accumulated a total of 3953 valid measurements, 3018 of which (76%) were from PC and 935 (24%) were from HC. In our sample, 2169 patients (55%) were women (M/W), and the rest, 1784, were men (M/M). The M of A1c/FGP were accompanied by requests for creatinine measurements in 98% of cases, eGFR in 72%, and ACR in 67%. If we compare by the origin of the patient (PC vs HC), creatinine levels were requested in 98% vs 98% (NS), eGFR was requested in 77% vs 54% (P<.01), and ACR was requested in 74% vs 46% of cases (P<.01).
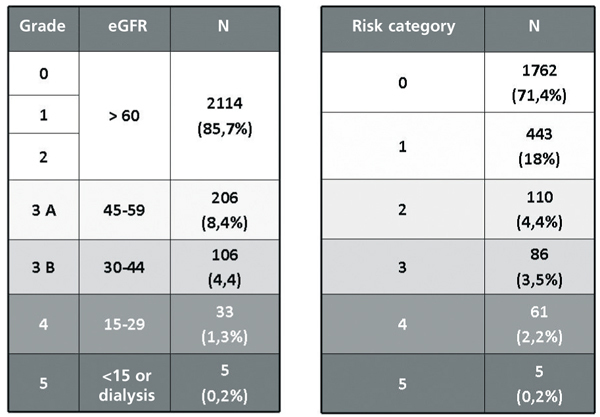
The results obtained from using the two classifications mentioned are summarised in Figure 2. In accordance with Tonelli, 2011, the low-risk situations (categories 0 and 1) increase, the moderate risk situations (2 and 3) decrease, and high-risk (category 4) also increase.
In spite of the usual biases inherent to observational retrospective studies that only examine measurements, we can state that: firstly, the normal evaluation of renal profiles is not correctly carried out, not all of the recommended parameters are requested; secondly, applying the new classifications, the highly debated level 3 of the KDOQI, 2002 decreases, due to the inclusion of proteinuria, provoking those patients that do not have this condition to descend to a lower category, whereas those that do are raised in category; and as such, lastly, the use of the new classifications can give greater reliability to the categorisation of patients at risk of CKD, and consequently improve the quality of referrals to nephrological consultations.
Figure 1. Proposal of a new classification system of chronic kidney disease by Tonelli, et al (ref. 6)
Figure 2. Comparative results of the application of the different chronic kidney disease classifications to measurements from our studies