The evidence of glomerular filtration rate (GFR) estimating with serum creatinine based formulae in the elderly population is scarce. The purpose of this study is to compare CKD-EPI, MRD4-IDMS and BIS1 equations to analyze correlation and concordance in a population older than 85 years old.
Patients and methodsWe designed a retrospective cross-sectional study, which included data from 600 patients older than 85 years. GFR was estimated by the following equations: CKD-EPI, MDR4-IDMS and BIS1, using as variables sex, age and serum creatinine concentration. Statistics analysis included Wilcoxon test, Bland–Altman plot, non-parametric Passing–Bablok method and kappa statistic (simple and weighted).
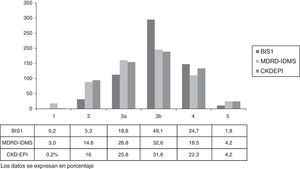
ResultsThe patients’ median (range) age was 87 (interval 85–98). The median GFR (range) was 42.4 (5.2–127.4)mL/min/1.73m2, when it was estimated with MDRD-IDMS, 40.0 (4.5–93.1) for CKD-EPI and 36.9 (7.6–83.7) for BIS1. The comparison of BIS1 and CKD-EPI and MDRD-IDMS using the Wilcoxon test was significant (p<0.001). The regression analysis yielded the following equations: MDRD-IDMS=1.025×CKD-EPI+1.360; BIS1=0.688×CKD-EPI+9.074 and BIS1=0.666×MDRD-IDMS+8.401. The weighted coefficient was 0.958 for the concordance between MDRD-IDMS and CKD-EPI, 0.812 for the concordance between MDRD-IDMS and BIS1 and 0.846 for CKD-EPI and BIS1.
ConclusionsThe GFR estimations obtained with BS1 equation are not interchangeable with MDRD-IDMS or CKD-EPI equations. BIS1 estimates lower GFR values than MDRD-IDMS and CKD-EPI and tends to classify the patients in a more advanced chronic kidney disease stage, especially for estimated GFR higher than 29mL/min/1.73m2.
La estimación del filtrado glomerular (FG) en el anciano con las fórmulas basadas en la creatinina es limitada. El objetivo del estudio es comparar las ecuaciones CKD-EPI, MDRD-IDMS y BIS1 y analizar la correlación y la concordancia en una población mayor de 85 años.
Pacientes y métodosRealizamos un estudio transversal retrospectivo y se recogieron datos de 600 pacientes mayores de 85 años. Se estimó el FG por las ecuaciones CKD-EPI, MDRD-IDMS y BIS1 a partir de datos de sexo, edad y creatinina. El estudio estadístico incluyó el test de Wilcoxon, análisis de Bland-Altman, rectas de regresión de Passing-Bablok, concordancia bruta e índice ponderado.
ResultadosLa mediana (intervalo) de edad de los pacientes fue 87 (85-98). Las medianas del filtrado glomerular estimado por MDRD-IDMS fueron 42,4 (5,2-127,4) mL/min/1,73m2, según CKD-EPI 40,0 (4,5-93,1) mL/min/1,73 m2 y por BIS1 36,9 (7,6-83,7) mL/min/1,73m2. La comparación mediante test de Wilcoxon de BIS1 con CKD-EPI y MDRD-IDMS fue significativa (p<0,001). El análisis de regresión dio lugar a las siguientes ecuaciones: MDRD-IDMS=1,025×CKD-EPI+1,36; BIS1=0,688×CKD-EPI+9,074 y BIS1=0,666×MDRD-IDMS+8,401. La concordancia ponderada entre MDRD-IDMS y CKD-EPI fue κ=0,598; entre MDRD-IDMS y BIS1: κ=0,812 y entre CKD-EPI y BIS1: κ=0,846.
ConclusionesLas estimaciones de FG obtenidas con la ecuación BIS1 no son intercambiables ni con MDRD-IDMS ni con CKD-EPI. La ecuación BIS1 presenta valores más bajos que MDRD-IDMS y CKD-EPI, y tiende a clasificar en un estadio mayor de ERC a los pacientes, sobre todo a partir de un FG estimado de 29mL/min/1,73 m2.
Chronic renal failure is health problem worldwide and the prevalence increases with the aging of the population. According to a epidemiological study in Spain “Epidemiology of chronic renal failure in Spain (EPIRCE)1 a 6.8% of the adult population has CKD with a GFR <60mL/min/1.73m2; if the population selected is >64 year the prevalence of CKD increases to 21.4%. The estimation of the GFR (eGFR) using formulas based on the values of serum creatinine concentration are the widely used to detect CKD in the entire population.
Screening for CKD is made by estimation of GFR, based in several equations that use values of serum creatinine (Cr) concentration,2 and the measurement the albumin/Cr ratio in urine. This method is being recommended by the Spanish Society of Clinical Chemistry and Molecular Pathology, the Spanish Society Of Nephrology and The Spanish Society of Primary Care Medicine. The most common equations utilized for estimation of GFR are: MDRD-IDMS (Modification of Diet in Renal Disease which includes 4 variables)3 and the CKD-EPI (Chronic Kidney Disease Epidemiology Collaboration which depends on the serum values of Cr)4 Also it is recommended to use the criteria of National Kidney Foundation Kidney Disease Outcomes Quality Initiative (NKF-KDOQI)5 to detect CKD in the entire population including young and aged individuals. Values of estimated GFR (eGFR) <60mL/min/1.73m2 are contemplated CKD but it should be contemplated that the GFR decreases with age in a physiological manner. From age 30 to 70 the GFR decreases 0.8mL/min/1.73m2/year and from age 70 the decline is 1.05mL/min/1.73m2/year.6 Thus it is important to take into consideration other parameters such as albuminuria, anemia, hyperphosphatemia, abnormalities of the urine sediment.
There reports on CKD screening in population of individuals 60–80 y.o.7–9 using equations to calculate eGFR based on serum Cr. Information about the use of these equations in individuals >85 years of age is limited; the diet, weight and body surface10 are different in elderly and younger people. The study by Gómez-Pavón et al.9 in 70 patents >75 y.o. concludes that the values of eGFR obtained by the MDRD-IDMS are not the same as eGFR corrected by body surface or the estimated by the Cockcroft–Gault equation.9 The MDRD-IDMS3 equation is not valid for people >72 y.o. and it was generated using only individuals with CKD. The formula CKD-EPI,4 developed in 2009, it is more precise and was generated based in a population with GFR >60mL/min/1.73m2, it is better than MDRD-IDMS to separate patients in the different stages of CKD. Furthermore, as compared with MDRD-IDMS, the CKD-EPI correlates better with direct measurements of GFR such as creatinine clearance and iothalamate clearance,4 and this is true also in elderly people11; a limitation of the CKD-EPI is that the evaluation was done only in 28 patients older that 80 in a total population of 5504 individuals. In the year 2012 the Berlin Initiative Study generated two new equations (BIS1 and BIS2) based in a sample of 570 patients >70 y.o. The BIS1 equation includes serum Cr, age and gender and the BIS2 includes also cystatin C. As compared with BIS1, BIS2 correlates with the measurement of GFR (plasma clearance of iohexol), but in people >70 y.o. it is recommended to use BIS1 if the measurement of cystatin C is not available, although results from external validation of this equation are not homogeneous.13,14 As far as the measurement of GFR by calculating the Cr clearance it should be pointed out that there is tubular secretion of Cr leading to overestimation of the GFR and this tubular secretion of Cr is increased as the GFR declines; furthermore and elderly individual had more difficulties to collect urine during 24h.
The aim of the present study is to compare the results obtained using the 3 different equations to estimate GFR: CKD-EPI, BIS1 and MDRD-IDMS, in patients >85 y.o. attending out patient primary care or specialized clinics. Will also analyze if the method to estimate GFR has an impact in the classification of patients in the different stages of CKD.
Patients and methodThis is a retrospective transversal study including patient's data from January 2009 to May 2015. There were 600 patients >80 y.o. with a determination of serum Cr that were seen in outpatient clinics of the Nuestra Señora del Prado de Talavera de la Reina Hospital or primary care centers of the area. Data was collected with the help of the information system Omega 3000 (Roche Diagnostic®). The following variables were collected: age, gender, serum Cr biochemistry was measured by autoanalyzer Cobas 711 (Roche Diagnostic®). The serum Cr was quantified by compensated kinetic Jaffé method which offers direct traceability and calibration against the reference method isotope dilution mass spectrometry (ID/MS). Reference values of serum Cr with this method are <0.9mg/dL for females and <1.1mg/dL for males.
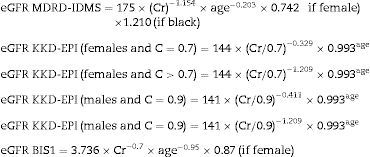
The eGFR was calculated using the equations MDRD-IDMS,3 CKD-EPI4 and BIS1.12
Equations used to calculate the eGFR (mL/min/1.73m2)eGFR units: mL/min/1.73m2; serum Cr units: mg/dL; and age in years.
The CKD stages were established according to the criteria of the Kidney Disease Improving Global Outcomes (KDIGO).5
The study was approved by the Ethics Committee of the Hospital “Nuestra Señora del Prado de Talavera de la Reina (Toledo)”.
Statistical analysisVariables were recorded in Excel 2007 to be subsequently analyzed with SPSS v15, Epidat 4.1 and Med-Calc v 11.3. Age, Cr and eGFR did not follow a normal distribution (p<0.05, test de Shapiro–Wilk), so means were compared by the non-parametric Wilcoxon test. Qualitative variables are expressed as frequency and percentage; quantitative variables are expressed as median, mean and interval. The degree agreement between equations was evaluated by non-parametric regression test of Passing and Bablok15 and the Pearson correlation. The prevalence of the different CKD stages for the 3 methods of eGFR was determined; and the agreement between the different methods was evaluated by the weighted “κ” index the gross agreement.
Bland–Altman16 graphs were obtained to estimate deviation among the 3 eGFRs. Significance was accepted if p<0.05.
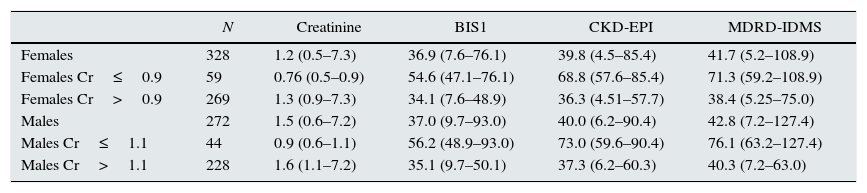
ResultsSample size is 600, 272 males (45.3%), median age 87 (interval: 85–98). Table 1 shows the medians of Cr and of the eGFR by the 3 equations separated by gender and serum Cr. Table 2 shows the medians of Cr and of the eGFR by CKD-EPI and MDRD-IDMS and the comparison with BIS1. The values obtained with BIS1 are significantly reduced as compared with MDRD-IDMS and CKD-EPI.
Characteristics of the population.
| N | Creatinine | BIS1 | CKD-EPI | MDRD-IDMS | |
|---|---|---|---|---|---|
| Females | 328 | 1.2 (0.5–7.3) | 36.9 (7.6–76.1) | 39.8 (4.5–85.4) | 41.7 (5.2–108.9) |
| Females Cr≤0.9 | 59 | 0.76 (0.5–0.9) | 54.6 (47.1–76.1) | 68.8 (57.6–85.4) | 71.3 (59.2–108.9) |
| Females Cr>0.9 | 269 | 1.3 (0.9–7.3) | 34.1 (7.6–48.9) | 36.3 (4.51–57.7) | 38.4 (5.25–75.0) |
| Males | 272 | 1.5 (0.6–7.2) | 37.0 (9.7–93.0) | 40.0 (6.2–90.4) | 42.8 (7.2–127.4) |
| Males Cr≤1.1 | 44 | 0.9 (0.6–1.1) | 56.2 (48.9–93.0) | 73.0 (59.6–90.4) | 76.1 (63.2–127.4) |
| Males Cr>1.1 | 228 | 1.6 (1.1–7.2) | 35.1 (9.7–50.1) | 37.3 (6.2–60.3) | 40.3 (7.2–63.0) |
Results are expressed as median and the interval (minimum and maximum).
Creatinine (Cr) units: mg/dL and eGFR units: mL/min/1.73m2.
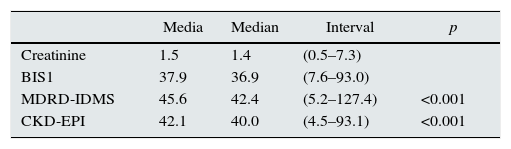
Comparison of GFR calculated with BIS1 and with MDRD-IDMS and CKD-EPI.
| Media | Median | Interval | p | |
|---|---|---|---|---|
| Creatinine | 1.5 | 1.4 | (0.5–7.3) | |
| BIS1 | 37.9 | 36.9 | (7.6–93.0) | |
| MDRD-IDMS | 45.6 | 42.4 | (5.2–127.4) | <0.001 |
| CKD-EPI | 42.1 | 40.0 | (4.5–93.1) | <0.001 |
Non-parametric comparison by Wilcoxon test of eGFR calculated with BIS1 and with MDRD-IDMS and CKD-EPI. Creatinine units: mg/dL; eGFR units: mL/min/1.73m2 and the interval (minimum and maximum).
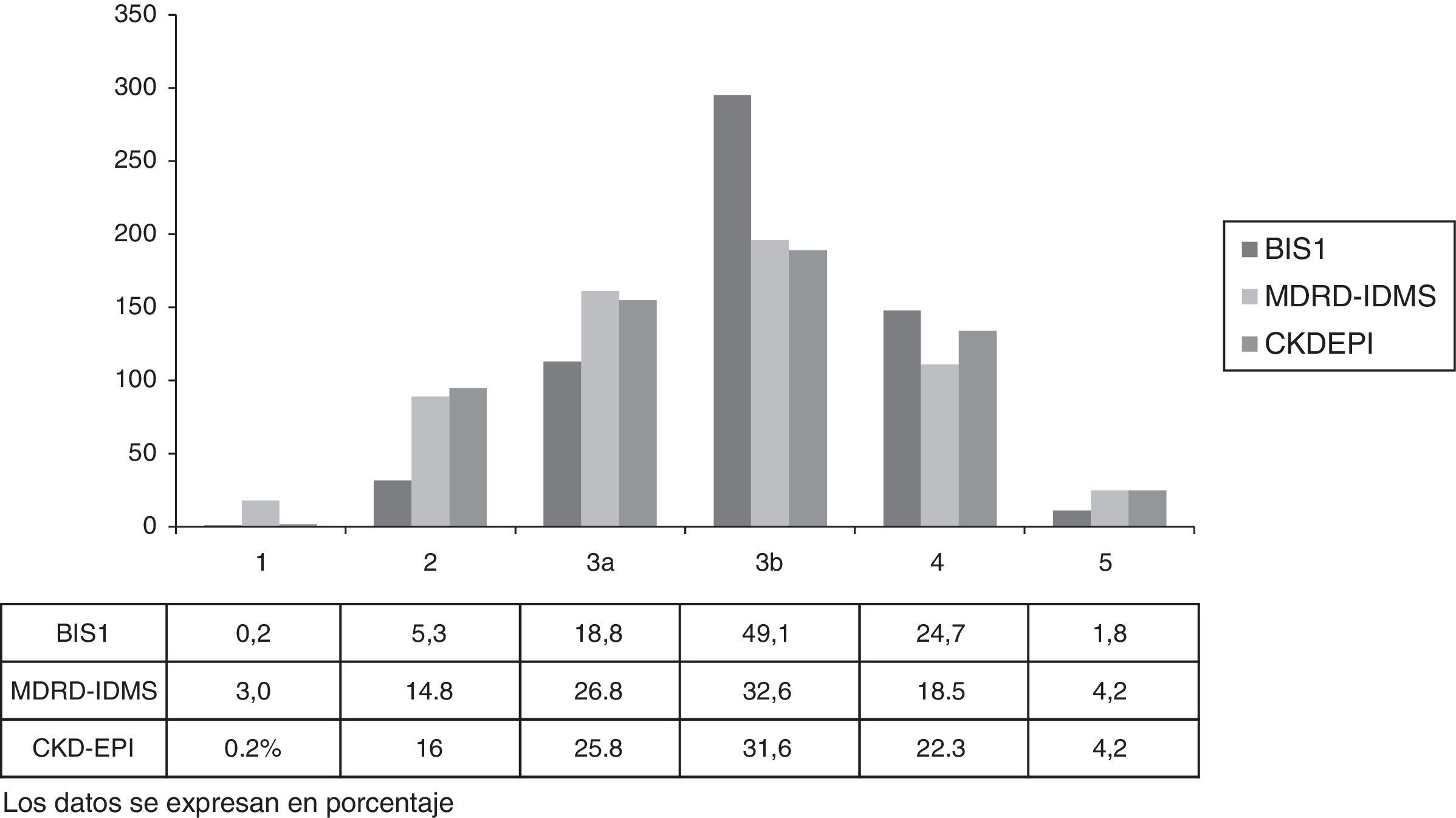
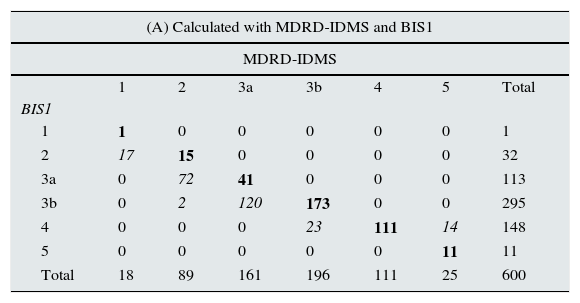
Classifications of CKD stages using BIS1 relative to MDRD-IDMS and CKD-EPI are shown in Table 3.
Number of subjects in CKD stages according to calculations with BIS1 vs MDRD-IDMS and CKD-EPI, and MDRD-IDMS vs CKD-EPI.
| (A) Calculated with MDRD-IDMS and BIS1 | |||||||
|---|---|---|---|---|---|---|---|
| MDRD-IDMS | |||||||
| 1 | 2 | 3a | 3b | 4 | 5 | Total | |
| BIS1 | |||||||
| 1 | 1 | 0 | 0 | 0 | 0 | 0 | 1 |
| 2 | 17 | 15 | 0 | 0 | 0 | 0 | 32 |
| 3a | 0 | 72 | 41 | 0 | 0 | 0 | 113 |
| 3b | 0 | 2 | 120 | 173 | 0 | 0 | 295 |
| 4 | 0 | 0 | 0 | 23 | 111 | 14 | 148 |
| 5 | 0 | 0 | 0 | 0 | 0 | 11 | 11 |
| Total | 18 | 89 | 161 | 196 | 111 | 25 | 600 |
| (B) Calculated with CKD-EPI and BIS1 | |||||||
|---|---|---|---|---|---|---|---|
| CKD-EPI | |||||||
| 1 | 2 | 3a | 3b | 4 | 5 | Total | |
| BIS1 | |||||||
| 1 | 1 | 0 | 0 | 0 | 0 | 0 | 1 |
| 2 | 0 | 32 | 0 | 0 | 0 | 0 | 32 |
| 3a | 0 | 64 | 49 | 0 | 0 | 0 | 113 |
| 3b | 0 | 0 | 106 | 187 | 2 | 0 | 295 |
| 4 | 0 | 0 | 0 | 2 | 132 | 14 | 148 |
| 5 | 0 | 0 | 0 | 0 | 0 | 11 | 11 |
| Total | 1 | 96 | 155 | 189 | 134 | 25 | 600 |
| (C) Calculated with CKD-EPI and MDRD-IDMS | |||||||
|---|---|---|---|---|---|---|---|
| CKD-EPI | |||||||
| 1 | 2 | 3a | 3b | 4 | 5 | Total | |
| MDRD-IDMS | |||||||
| 1 | 1 | 17 | 0 | 0 | 0 | 0 | 18 |
| 2 | 0 | 79 | 10 | 0 | 0 | 0 | 89 |
| 3a | 0 | 0 | 145 | 16 | 0 | 0 | 161 |
| 3b | 0 | 0 | 0 | 173 | 23 | 0 | 196 |
| 4 | 0 | 0 | 0 | 0 | 111 | 0 | 111 |
| 5 | 0 | 0 | 0 | 0 | 0 | 25 | 25 |
| Total | 1 | 96 | 155 | 189 | 134 | 25 | 600 |
Numbers in bold are those subjects that did not change the stage.
Numbers in italic are those subjects that changed the stage.
The estimation of GFR by BIS1 equation modifies the CKD classification in 248 (41.3%) and 188 (31.3%) with respect to the equations MDRD-IDMS and CKD-EPI respectively; this difference mainly concerns to stage 3b as shown in Fig. 1. Using the equation BIS1, 568/600 (94.6%) of the individuals present a eGFR <60mL/min/1.73m2; this number changes to 494/600 (82.3%) if GFR is calculated using the formula MDRD-IDMS and it changes to 505/600 (84.2%) if calculation is made with the CKD-EPI equation. If, as other author suggest,17 the cutting value for CKD is set at eGFR 38mL/min/1.73m2 the prevalence of CKD is 44.4% according to CKD-EPI, 54.3 using BIS1 and 38.3% if the calculation are made using MDRD-IDMS formula.
The analysis of agreement between MDRD-IDMS and CKD-EPI reveals a value of weighted kappa of 0.958 (95% CI: 0.948–0.968), while with the BIS1 equation the value of weighted kappa is 0.812 (95% CI: 0.789–0.936) and 0.846 (95% CI: 0.824–0.866), as compared with MDRD-IDMS and CKD-EPI, respectively. The degree of agreement between MDRD-IDMS and CKD-EPI was 89.2%, between BIS1 and MDRD-IDMS 59.1% and between BIS1 and CKD-EPI 68.5%.
Among the subjects that were changed of CKD stage after estimation by BIS1 with respect to MDRD-IDMS, 232 (38.6%) were change to one stage superior and 2 (03%) were changed to 2 stages above the initial; 14 individuals (2.3%) were reclassified to a lower stage of CKD. The most numerous changes were observed in stage 3a with 120 individuals (74.5%) being changed to stage 3b after application of the BIS1. With the use of CKD-EPI equation, 172 (28.6%) subjects were changed to a superior stage and 16 (2.6%) to a inferior stage. Most changes concerned to stage 3a, in which 106 (68.3%) were changed to stage 3b. In relation to MDRD-IDMS, the equation CKD-EPI change 66 (11%) subjects to a superior stage and none to an inferior stage.
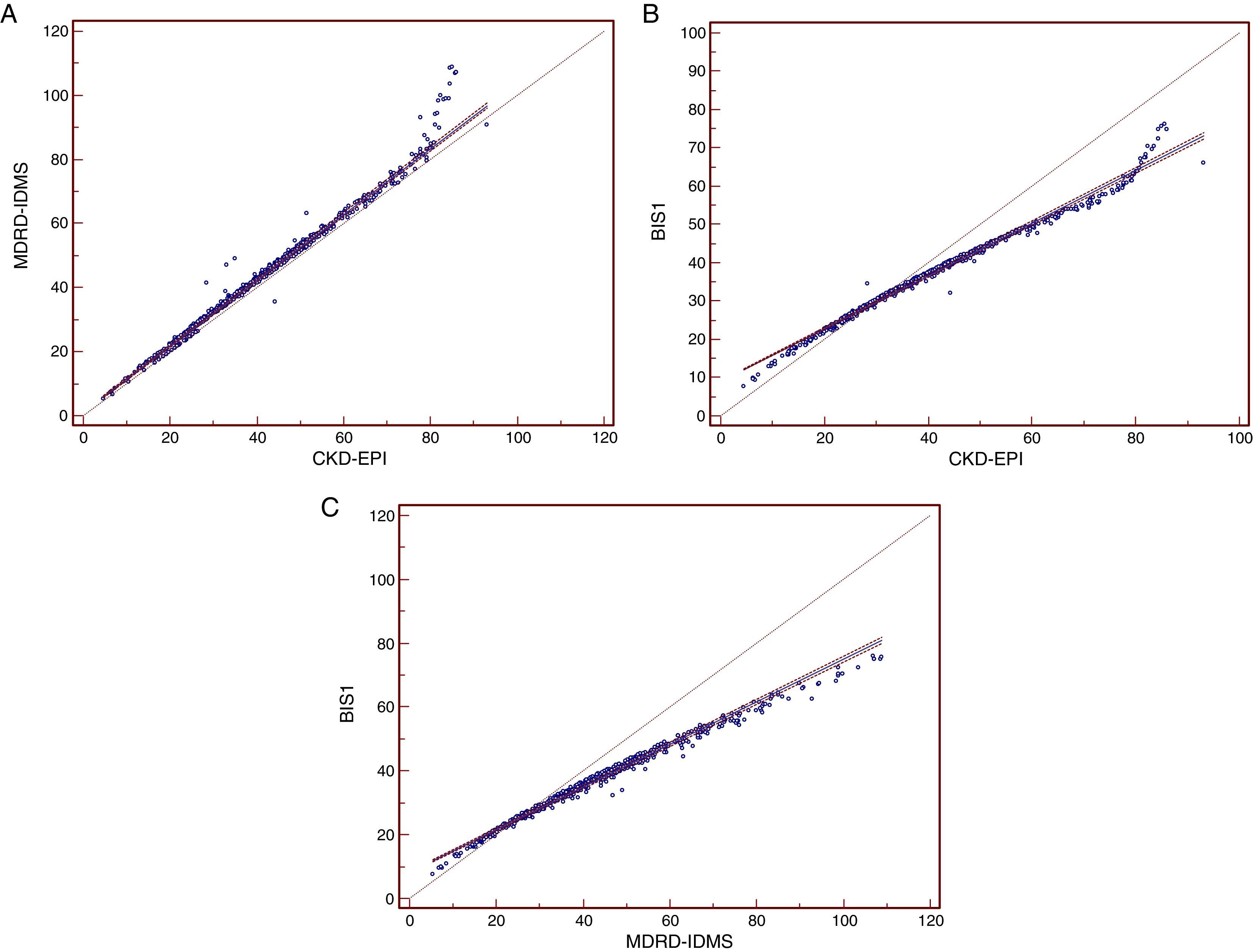
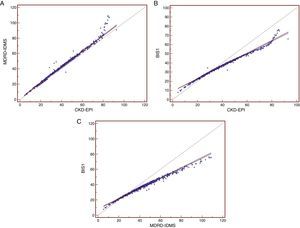
The Passing–Bablok regression (Fig. 2) including the different GFR equations produced the following results: MDRD-IDMS=1.025×CKD-EPI (95% CI: 1.019–1.030)+1.36 (95% CI: 1.152–1.568) with a correlation coefficient r=0.990 (95% CI: 0.989–0.992); BIS1=0.688×CKD-EPI (95% CI: 0.682–0.694)+9.074 (95% CI: 8.843–9.318) with r=0.993 (95% CI: 0.992–0.994) and BIS1=0.666×MDRD-IDMS (95% CI: 0.659–0.673)+8.401 (95% CI: 8.100–8.659) with r=0.992 (95% CI: 0.991–0.994).
Rectas de regresión de Passing-Bablock de las ecuaciones de filtrado glomerular. Rectas de regresión de Passing-Bablok entre las distintas ecuaciones para la estimación del filtrado glomerular. (A) Recta de regresión MDRD4-IDMS-CKDEPI. (B) Recta de regresión BIS1-CKDEPI. (C) Recta de regresión.
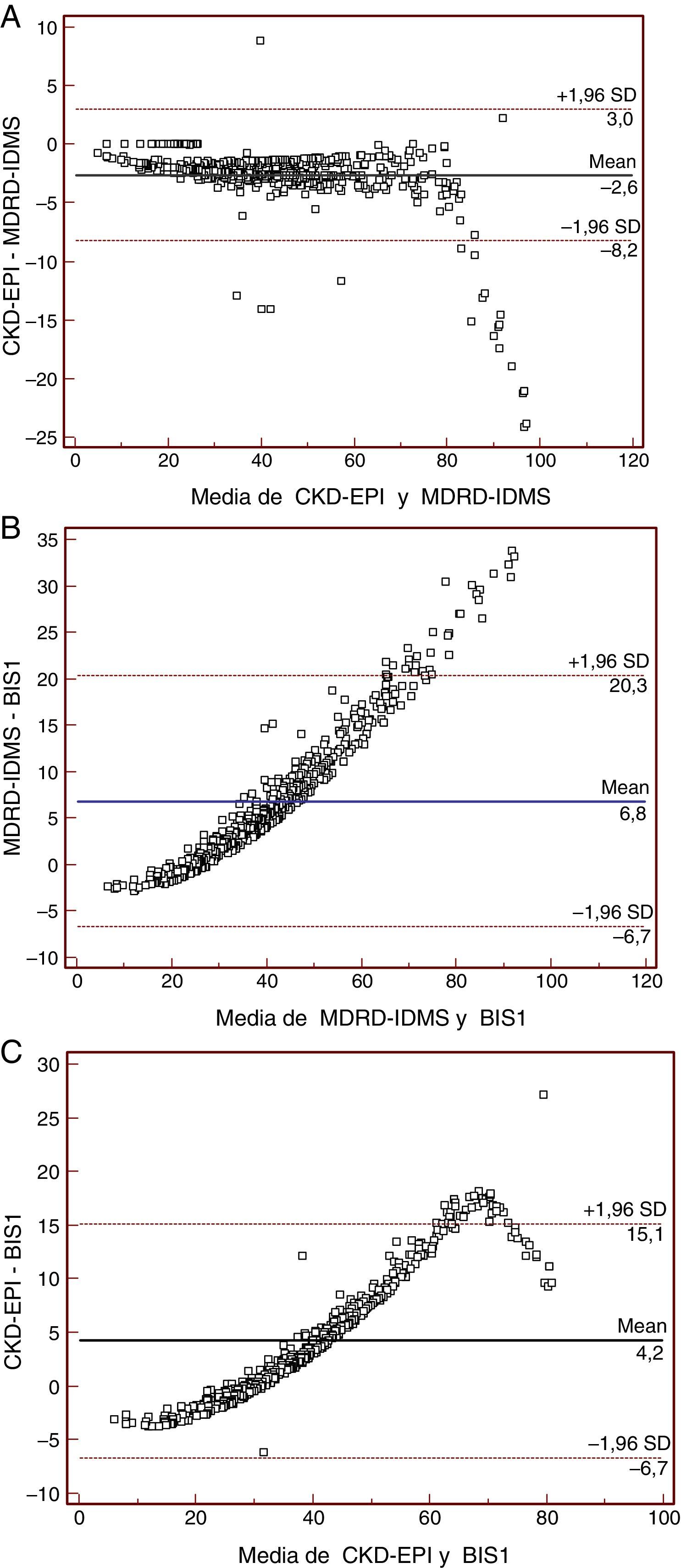
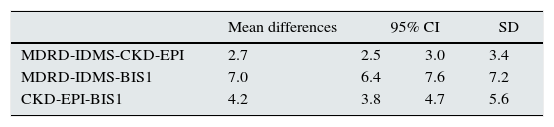
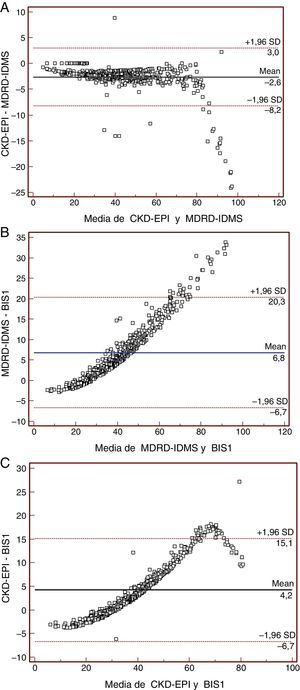
The results of Bland–Altman test are shown in Table 4 and Fig. 3. Comparison of MDRD-IDMS and CKD-EPI is shown in Fig. 3a; from values above eGFR of 75–80mL/min/1.73m2 there an increased dispersion but there differences were homogenous up to that value. Fig. 3b shows that a difference between the two estimations of GFR increases with the value of GFR throughout the entire range of values, while in Fig. 3c this increase is observed until eGFR values of 75–80mL/min/1.73m2.
The GFR is the best method to assess renal function and it is necessary for a correct use of the dose of medication. In clinical practice there are several formulas available for the calculation of GFR18 so the 24h urine collection is avoided, such a procedure is not easy in this population. Recently, Schaeffner et al.12 had developed 2 new equations, BIS1 and BIS2, to obtain better estimation of GFR in people older that 70 years.
Lopes et al.19 shows that the equation BIS1 is more exact than the MDRD-IDMS and CKD-EPI in patients older that 80 years with a GFR <60mL/min/1.73m2. In our study we have compared BIS with MDRD-IDMS and CKD-EPI in patients older than 85 years. The equation BIS1 and the BIS2 were obtained from a population >70 years with a mean of 78.5 years of age.
In our study we have found that GFR calculated by BIS1 is lower than with MDRD-IDMS and CKD-EPI. Table 1 shows that the values of eGFR obtained using the BIS1 equation in people with serum Cr below the reference values are similar independent of gender and the values are lower than those obtained with the equations MDRD-IDMS and CKD-EPI. Besides, there is less dispersion of eGFR calculated with BIS1 since the sample used to develop BIS1 is similar to that presented in this study.
As compared with MDRD-IDMS, la difference of the means is 7.7mL/min/1.73m2 (18%) and with CKD-EPI the difference is 4.23mL/min/1.73m2 (10%). As compared with the results reported by Schaeffner et al.,12 the differences are similar for MDRD-IDMS (19.6%) but are less for CKD-EPI (19.6%). In the study by Koppe et al.,20 with 224 patients and a mean age of 75.3 years the difference between values obtained with BIS1 and both MDRD-IDMS and CKD-EPI were similar (7 and 5%, respectively). These results are not the same as ours, and the explanation could be that the sample is size different and our population is older. Considering these differences, estimations with BIS1 results in a greater proportion of patients with severe CKD since there will be more patients allocated to stages 3b and 4. This change in the classification of the CKD stage is supported by the fact that in people with eGFR <30mL/min/1.73m2 there is a better correlation between BIS1equation and the gold standard GFR20 measurement than between the CKD-EPI and MDRD-IDMS and the gold standard GFR.
Our study shows that the use of BIS1 produces some differences in the population older than 85 years. With this age, the values of eGFR using BIS1 are reduced as compared with CKD-EPI if the GFR is less than 29mL/min/1.73m2. Therefore using BIS1 the prevalence of CKD in this population increases independently of whether the limit for CKD is set at 60 or 38mL/min/1.73m2.17,21 With the use of the formula BIS1the prevalence of CKD (GFR <60mL/min/1.73m2) would be increased a 11 and a 12.6% as compared with the CKD-EPI and MDRD-IDMS methods respectively. If CKD is considered with a GFR <38mL/min/1.73m2 the respective increase in prevalence would be 8.5% and 15.4%. Using the formula BIS1 the percent of patients with eGFR less than 30mL/min/1.73m2 being sent to nephrologists from primary health care doctors will be 26.5% which is not different with respect to CKD-EPI but it is greater than MDRD-IDMS (22.8%); this difference of 4% is less than the values obtained (12%) in another study performed in Spain22 although the patients in this study were >70 years.
There is an acceptable agreement between values obtained with CKD-EPI and MDRD-IDMS and patients are classified within the same CKD stage which confirms previous results.23,24 In general the values obtained with CKD-EPI are lower than with MDRD-IDMS so patients are reclassified to a superior stage of CKD, this is similar to other reports.25,26 Although the percent of patients reclassified is only 11% it is greater than the 2.6% obtained in another study6 that included 20.000 subjects with a mean age of 73.5. The values of weighted κ index from BIS1 equation vs MDRD-IDMS and CKD-EPI are not very low (κ>0.8), but the values obtained after analysis of gross agreement are clinically unacceptable since a large number of patients are reclassified.
The Passing–Bablok linear correlation analysis shows a constant and proportional with respect to MDRD-IDMS and CKD-EPI; thus, the results obtained with these two equation is not exchangeable results obtained BIS1. The BIS1 derived values are inferior to the obtained with CKD-EPI and MDRD-IDMS in patients with a GFR lower than 25mL/min/1.73m2. This is also illustrated in the Bland–Altman graphs which reveal that the greater the GFR, the larger the difference between values of BIS1 vs CKD-EPI and MDRD-IDMS. These results are in agreement with other reports showing that MDRD-IDMS and CKD-EPI overestimate the GFR with respect to as direct gold standard GFR measurements mainly if GFR is above 60mL/min/1.73m2 and patients are >70 y.o.12,13,20 In addition dispersion of values analyzed by Bland–Altman test are, in both cases, too large from a clinical point of view. The observed differences in the regression lines and in the Bland–Altman graph indicate that it is necessary to modify the reference values if calculation of GFR are made with BIS1 in a elderly population without a renal disease. In this group of patients there is also a moderate overestimation of GFR by MDRD-IDMS as compared with CKD-EPI. This slight difference seen in people >85 y.o. is in contrast with other reports in younger patients in which the difference is greater27 and it is not no longer evident in people older that 70 years. We believe that similarities between our values and MDRD-IDM are due to the fact that the MDRD-IDMS equation was developed in a population with reduced GFR: mean 40mL/min/1.73m2 which is similar to the population evaluated in he present study. The CKD-EPI equation was developed from a population with higher GFR and even with normal GFR. In fact the Bland–Altman graph shows greater dispersion if GFR is greater than 80mL/min/1.73m2.
Limitations of this study include the fact that it does not represent the general population because the subjects included in the study came from primary care and specialized out patients clinics from a single health care area. In some patients, established renal disease was suspected. Estimation of the number of consultations to nephrologists was based on eGFR; albuminuria, anemia, hematuria, abnormal sediment or changes in parameters of mineral metabolism were not taken into consideration for this calculation. The equation developed in the work of Schaeffner et al. was based in a population with a high percentage of hypertension (76.1%) and diabetes mellitus (24%); we do not have information on the prevalence of diabetes mellitus and hypertension or the treatment received which is important in elderly people. The serum level of cystatin was not available therefore it was not possible to estimate GFR by the BIS2 formula.
As a conclusion, in people older than 85 years the calculation of GFR using different equations are not interchangeable from one method to another. The regular use of the BIS1 formula in people more that 85 y.o. result in values of eGFR lower that those obtained with MDRD-IDMS or CKD-EPI, consequently the prevalence of CKD will appear to be increased. The MDRD-IDMS or CKD-EPI methods overestimate the eGFR with respect to BIS1 due to the reduction of lean body mass that occurs in senescence. These values of eGFR may cause changes in the dose adjustment in some medication to avoid overdose that could occur if the other two equations are applied. It is observed that with the use of BIS1 patients are classified with more severe CKD stage, particularly from patients stage 2 are changed to 3a and from 3a to 3b. Since results from BIS1, MDRD-IDMS and CKD-EPI are not interchangeable it is necessary to establish new reference values of GFR for elderly people more than 70 years old if eGFR is calculated with the BIS1 equation; it is also needed to establish limits of GFR to define CKD in the elderly.
Conflict of interestThe authors declare not to have any potential conflict of interest in relation to the content of the present article.
Please cite this article as: Bustos-Guadaño F, Martín-Calderón JL, Criado-Álvarez JJ, Muñoz-Jara R, Cantalejo-Gutiérrez A, Mena-Moreno MC. Estimación del filtrado glomerular en personas mayores de 85 años: comparación de las ecuaciones CKD-EPI, MDRD-IDMS y BIS1. Nefrologia. 2017;37:172–180.