Variations in the use of healthcare services can be defined as systematic variations of adjusted rates for certain aggregation levels of the population. The study analyses how renal replacement therapy (RRT) is used, identifying RRT variability in Catalonia from 2002 to 2012.
Material and methodsEcological study by health area using data from the Catalan renal registry. We present incident rates, standardised incidence ratios and prevalence, while variability was calculated through direct and indirect standardisation methods.
ResultsFrom 2002 until 31/12/2012, 10,784 patients initiated RRT in Catalonia: 9238 on haemodialysis (HD) (50 treatments per 100,000 people 2010/2012), 1076 on peritoneal dialysis (PD) (8.2 treatments per 100,000 people 2010/2012) and 470 received an early kidney transplant (KT) (4.4 treatments per 100,000 people 2010/2012). Over the 10 years, the HD cumulative incidence rate fell (7%), while the PD and KT incidence rates increased (63% and 177%, respectively); both are higher in young patients (<45 years). 4750 patients received a kidney transplant in this period, 49% of which were aged between 45 and 65 years. There were no significant differences in variability in HD (RV5–95=1.3; Empirical Bayes [EB]∼0), or in the prevalence of KT (RV5–95=1.4; EB∼0). Nevertheless, we found significant geographical variability in PD; notably in the districts of the province of Lérida, where the number of cases observed was greater than expected (RV5–95=4.01; EB=0.08).
ConclusionAlthough there was a notable rise in PD and early KT incidence rates, PD is still underused when compared to international recommendations. No territorial variability was found for HD or KT, but the use of PD was found to be higher in Lérida than in other areas. To reduce PD territorial variability and increase the uptake of this technique in the other regions, we propose 3 initiatives: the development of RRT support tools for shared decision-making, the encouragement of specific PD professional training and the promotion of PD through complementary reimbursement systems.
Las variaciones en la utilización de servicios de salud pueden definirse como variaciones sistemáticas de las tasas ajustadas para ciertos niveles de agregación de la población. Analizamos el tratamiento sustitutivo renal (TSR) e identificamos la posible variabilidad en Cataluña entre 2002 y 2012.
Material y métodosEstudio ecológico por áreas de salud con datos del registro de enfermos renales de Cataluña. Presentamos tasas de incidencia, incidencia estandarizada y prevalencia. Variabilidad calculada mediante estadarización directa e indirecta.
ResultadosDesde 2002 hasta el 31/12/2012, 10.784 pacientes iniciaron TSR en Cataluña: 9.238 mediante hemodiálisis (HD) (50 tratamientos/100.000 habitantes 2010/2012), 1.076 diálisis peritoneal (DP) (8,2 tratamientos/100.000 hab. 2010/2012) y 470 recibieron un trasplante renal (TR) anticipado (4,4 tratamientos/100.000 hab. 2010/2012). Durante 10 años, la tasa de incidencia acumulada de HD ha descendido (7%) y las tasas de incidencia de DP y TR han aumentado (63 y 177%); ambas son más elevadas en pacientes jóvenes (<45 años). Un total de 4.750 pacientes recibieron en ese periodo un TR; el 49% con edad de 45 a 65 años. No detectamos variabilidad entre áreas en HD (RV5-95=1,3; empírico de Bayes [EB] ∼ 0), ni tampoco en la tasa de prevalencia en TR (RV5-95=1,4; EB ∼ 0). Detectamos variabilidad significativa entre áreas geográficas en la indicación de DP, en las comarcas de la provincia de Lérida, donde el número de casos observados era superior a los esperados (RV5-95=4,01; EB=0,08).
ConclusiónHay un notable incremento en la indicación de DP y TR anticipado, aunque la DP sigue infrautilizada considerando las recomendaciones internacionales. No hemos encontrado variación territorial en la indicación de HD y los casos con TR, pero sí en la indicación de DP: el área de Lérida es la que presenta unas tasas por encima del resto de las áreas. Para reducir la variabilidad territorial en DP incrementando la indicación de esta técnica en el resto de las comarcas, proponemos 3 actuaciones: desarrollo de herramientas de decisión en TSR compartidas, potenciación de formación específica en DP de los profesionales y promoción de la DP a través de sistemas de reembolso suplementarios.
From 2002 to 2012, the prevalence of stage 5 chronic kidney failure (CKD-5) has been persistently increasing, both in Catalonia and in Spain. In 2002, data from the Spanish Registry of Renal Patients (SRRP – Registro Español de Enfermos Renales), the Spanish Society of Nephrology (SSN – Sociedad Española de Nefrología) and the Spanish National Transplant Organisation (NTO – Organización Nacional de Trasplantes) showed an incidence of CKD stage 5 of 132 patients per million population (PMP), 94.4% of whom started renal replacement therapy (RRT), with haemodialysis (HD) as the first RRT; 4.6% started RRT with peritoneal dialysis (PD); and only 1% received an early renal transplantation (RT). The prevalence of CKD stage 5 in that year was 895 patients PMP.1 Incidence decreased to 120.4 patients PMP in 2012, but prevalence increased steadily, mainly due to the accumulation of patients who maintained a functioning RT.2 Data of year 2014 from the same registry, presented at the 45th SSN Conference in Valencia in October 2015, which included for the first time 100% of the population, showed that incidence was 133.6 patients PMP and the prevalence was 1179.3 patients PMP,3 for a Spanish population that at that time was 46,771,341 inhabitants.
In Catalonia the incidence of stage 5 CKD in 2002 was 146.8 PMP and the prevalence, 1017.8.4 Data from the Catalan Registry of Renal Patients (CRRP – Registre de Malalts Renals de Catalunya) for 2013 showed an incidence of 145.0 PMP and a prevalence of 1262.2.5
In Spain the annual cost of RRT for CKD stage 5 is more than 800 million euros. Although there are several estimates, this cost may represent up to 2.5% of the government's total annual health budget.6–9
Health care providers dealing with this disease, as well as patients themselves, face complex decisions such as, in most cases, making a decision of how the level of functional autonomy conditions the election the modality of RRT. Regarding RT, a risk–benefit analysis for patients has to be evaluated. And, of course, they must help to decide whether a patient should elect a conservative therapy.
All these decisions should be made by the patients themselves, with the help of health professionals, based on the best available evidence, and obviously, with the relevant family support, so that CKD patients are made aware of the risks and benefits of the different options used to treat their disease.
In the 1970s, Wennberg et al.10 studied the variations in health care service delivery. Since then, numerous studies have shown that place of residence may condition the number of hospitalisations, diagnostic tests or treatments, regardless of age, sex and the usual adjustment factors. Variations in health care delivery are matter of concern, because they indicate that some citizens receive less attention than they need, while others receive more and others receive care that they do not need,11 with a subsequent impact on both outcome indicators and health budgets that are limited. In Spain, as part of the “Atlas of Variations in Health Care Delivery in the National Health Service” project,12 and the one recently launched in Catalonia as part of this work,13 numerous studies have been conducted to analyse these variations for different diseases and procedures, although none have been dedicated to RRT. The study of RRT variations is of significant interest for patients and health care providers in terms of assessing whether the indications regarding the different RRT options—HD, PD or RT—are different according to geographic variability.
In a study of 31,778 patients at 56 sites in 13 regions of Canada, Sood et al.,14 adjusting the model by patient, site and region, it was found a variability in PD indication as the first RRT, with substantial differences in low indication (odds ratio 1.51; CI 95%: 1.33–1.73) versus high indication rates (odds ratio 0.69; CI 95%: 0.60–0.79), that were attributable to geographic region.
A few months later, these authors15 reported the findings on the study, extended to 33,263 patients and carried out between January 2001 and December 2010 at 63 sites in 14 different regions, also in Canada. Adjusting the model to type of patient and the dialysis centre, they found a variability in the indication of PD for RRT that was attributable in 96.9% of cases to the patient—case mix index—and in 3.1% of cases to the dialysis centre, with no variability in this study in relation to the region where the patients were included.
Couchaud et al.16 published data from the REIN registry. It was analysed the variability in PD indication in 10,815 incident cases from 59 districts in France and they compare, by using logistic regression models, factors such as age, gender, presence of diabetes, congestive heart failure, behavioural disorders, mobility and employment. PD was indicated in 14% of the incident cases, but with a large variability, from 0% to 45%, depending on the districts. The authors concluded that PD may be indicated in a wide array of different clinical conditions and that patients’ preferences play an important role in the choice of RRT method and therefore in this variability.
The aim of our study was to assess whether any variability in RRT indication might be due to inequity to the access or to other factors in different areas of health care in Catalonia.
Material and methodsEcological study of variability in RRT by areas of health care. An ecological study is a type of epidemiological study, in which the unit of analysis is a set of individuals from a community that is well-defined geographically. Ecological studies allows to analyse the frequency of a disease.
The study's main source of data was the Catalan Transplant Organisation's (CTO) CRRP. From January 1, 2002 to December 31, 2012, incident cases on HD and PD per year were selected according to age (<45, 45–64 and ≥65 years) and gender. Given the low incidence of RT as the first RRT it was more appropriate to work with prevalent cases in the years 2005, 2009 and 2012. The denominator to calculate activity rate (the number of inhabitants of each area) was obtained from the Central Registry of Insured Persons of the Catalan Health Service (CatSalut), the public insurance.17 We also obtained from this source the structure by age group and gender group to calculate indirect standardisation.
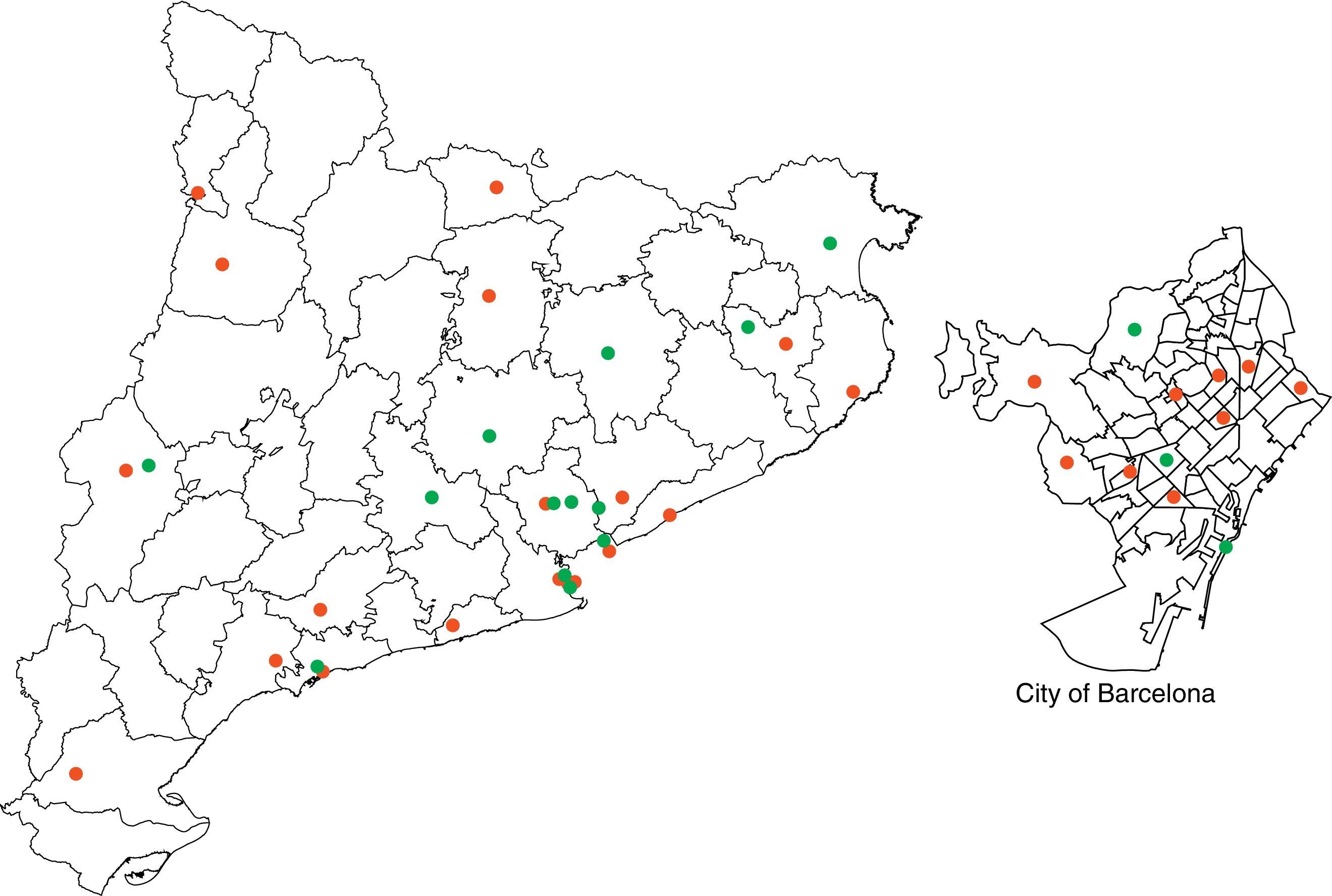
The unit of analysis—i.e. the geographic areas—are the 45 areas of Heath Care Management from the 7 Health Care Regions of Catalonia. The areas of health care management are clusters of basic health care areas, which define regions formed by one or more hospitals and closely related basic health care areas. It is an intermediate level of organisation where primary and specialised care activities are coordinated.18
The outcome measures used in this study were the crude incidence rates of HD and PD by area (per 100,000 inhabitants). The standardised ratio of HD and PD incidence compare the interventions performed by the residents in an (observed) area with those that would have been performed (expected) if each of their age/gender groups had an utilisation to equal the whole set. Last, we analysed the prevalence of RT in 2005, 2009 and 2012 by area and by group of age and gender.
First the crude and standardised HD and PD rates were calculated by area and by groups of age and gender. Next, the usual statistics parameters of variability were estimated in an analysis of small areas19: the rate of variation between the 75th and 25th percentiles (RV 25–75), the systematic coefficient of variation (SCV) and the empirical Bayes (EB) approach. The SCV and EB are statistics parameters of variation that take into account the part of the variation that is expected for the type of phenomenon and population analysed. Both identify a source of variation between areas (which is expected to be systematic) and another source of variation within the area (which is expected to be at random). Although they usually use similar values, the EB is a better estimator than the SCV when the events in the areas are uncommon, as the EB corrects the effect of over-dispersion or extra-variation that tends to produce estimates of extreme systematic variation. For both statistics, the higher the value, the greater the systematic variation. By using a procedure with no systematic variation as a reference, such as a hip fracture, it has traditionally been agreed that values up to 0.05 involve no systematic variation; up to 0.10–20, moderate variation; and from 0.20, high variation. However, it is essential to put the value in a given context for each study.
Then, the standardised HD and PD ratios were constructed, which were described by using dot charts—in which each area is represented by a dot—and one map for each health area. All the analyses were performed using STATA, v13.
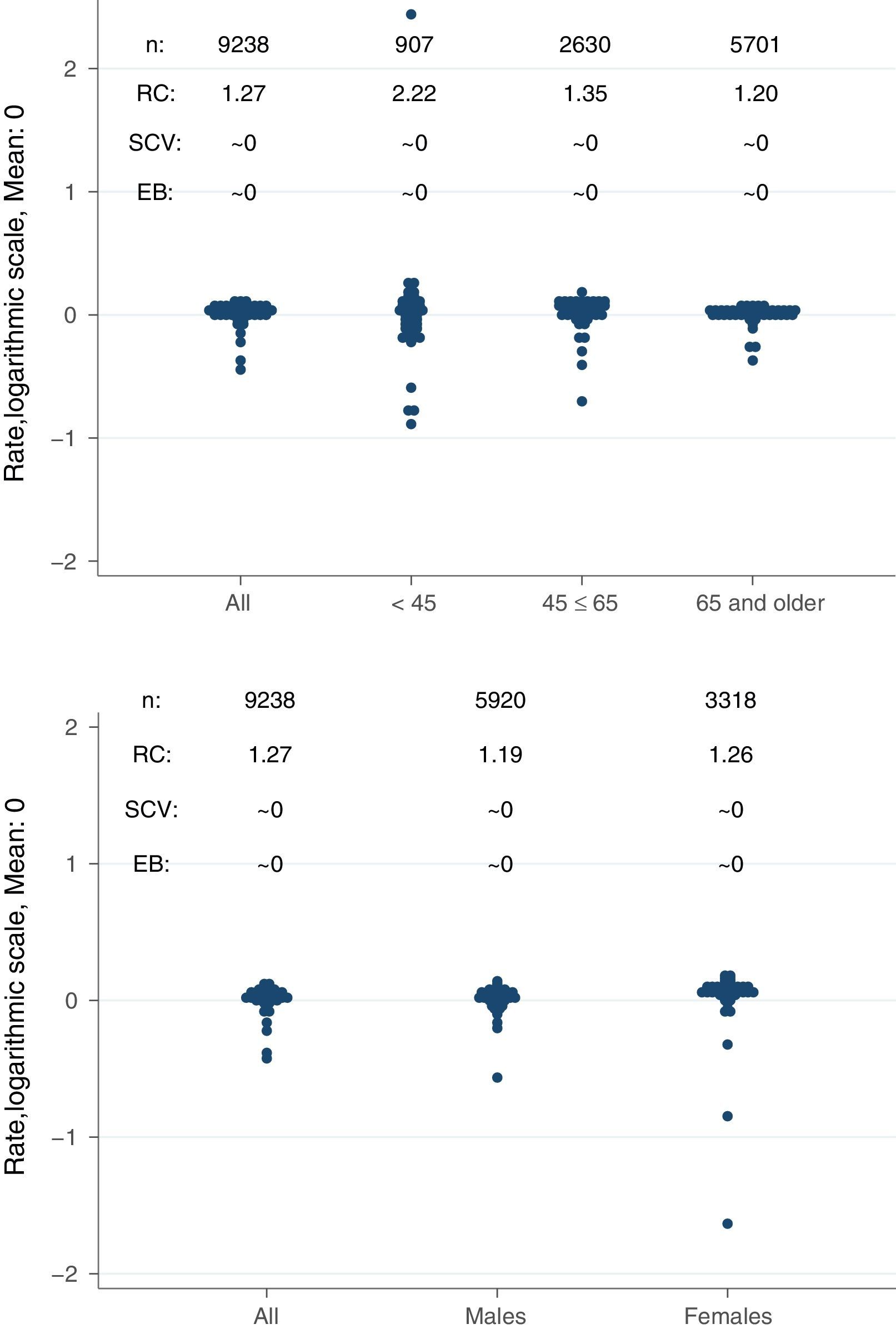
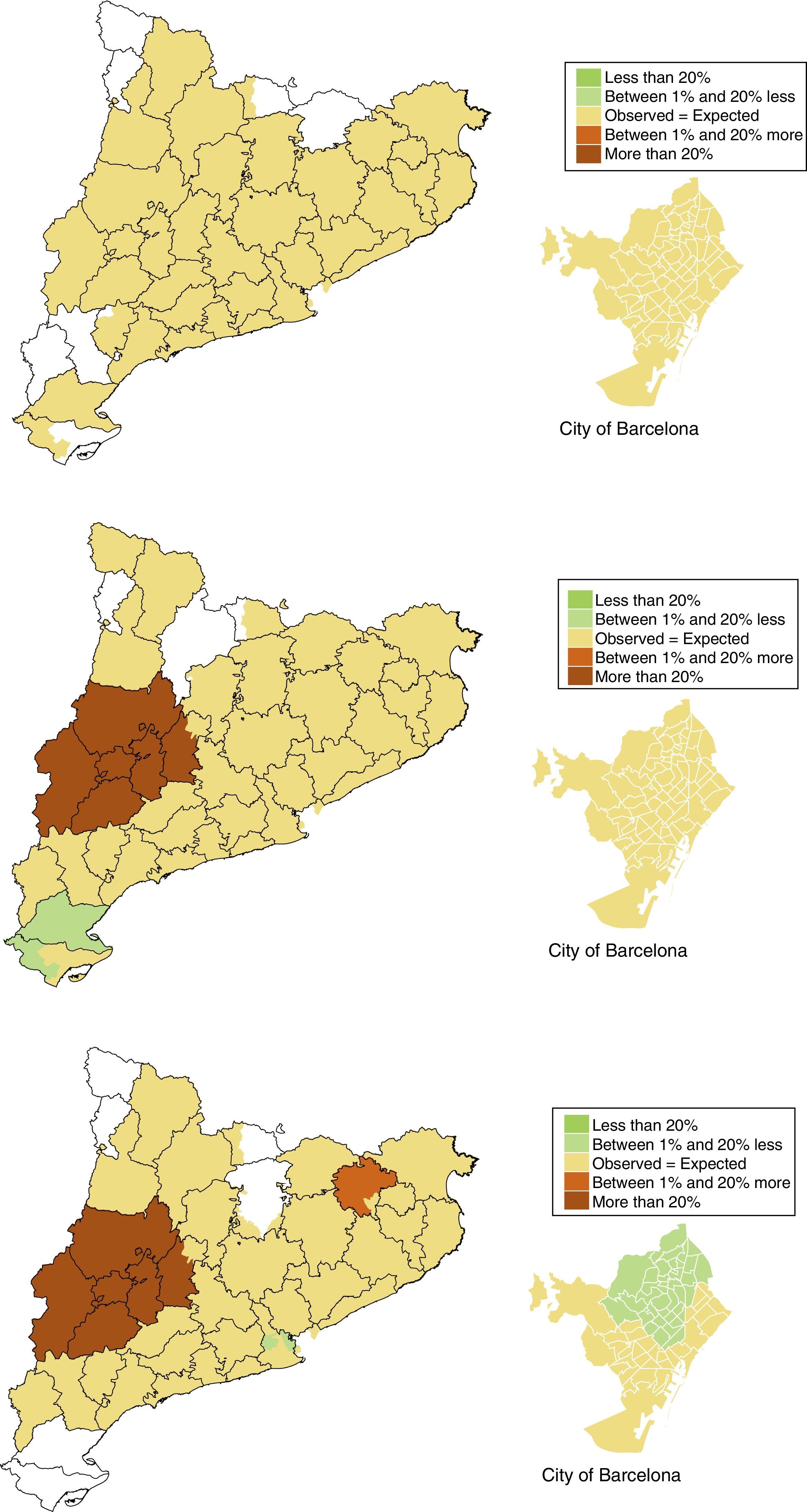
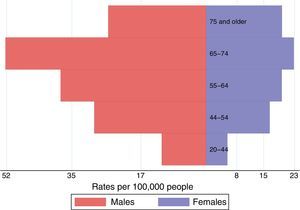
ResultsMaps of RRT variations: haemodialysisActivityBetween January 1, 2002 and December 31, 2012, 9238 patients started RRT using HD. Of these, 64% were men and 62% were >65 years. During this period, the cumulative incidence rates of HD decreased from 61 treatments per 100,000 inhabitants in the period 2002–2005 to 50 treatments per 100,000 inhabitants in the period 2010–2012 (Fig. 1).
The decrease in HD indication as the first RRT is related to the increase of PD and to the early RT. From 2010 to 2012, HD represented 80% of the indication in incident cases, while from 2002 to 2005, it was 90%.
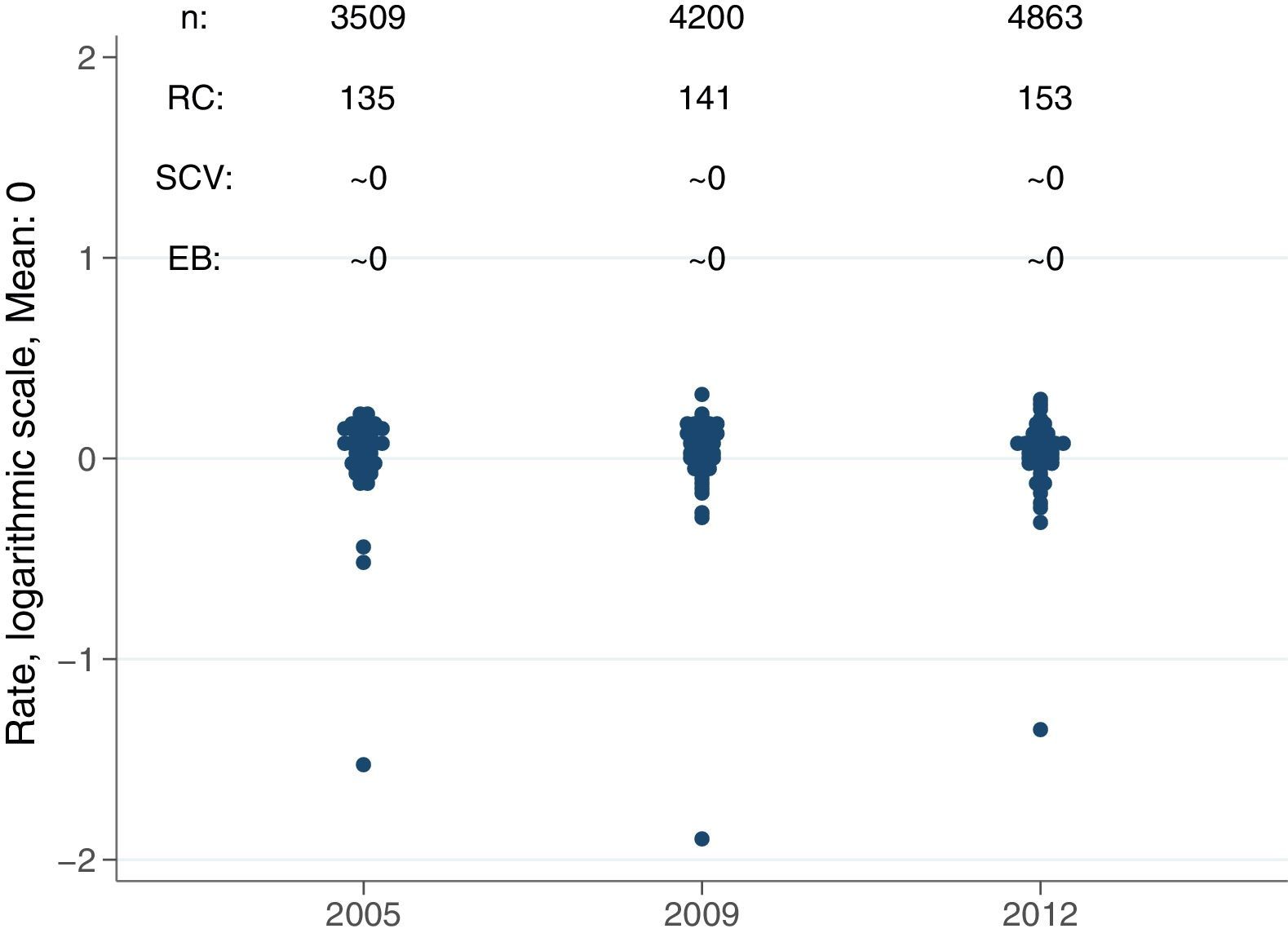
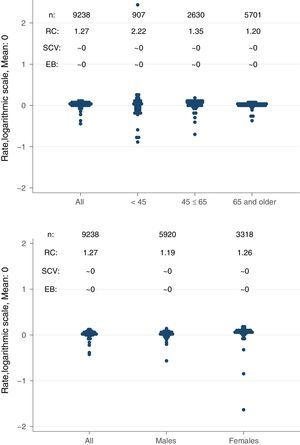
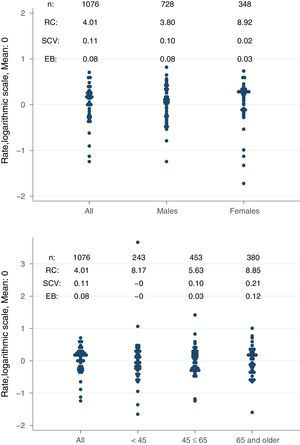
Magnitude of variationThe ratio of variation (RV25–75) of the rate of HD relative to that of PD and RT was 1.3 times higher in women and 1.2 times higher in men respectively. By age group, the RC25–75 was similar among those >45 and higher in <45. The statistic value that quantifies the non-random variation by area showed, as a whole and over time, a value associated with virtually no variation (EB≈0) Fig. 2). When studying the standardised ratio by age group, there was a pattern of zero variation, in which no area was significantly different from the mean in Catalonia.
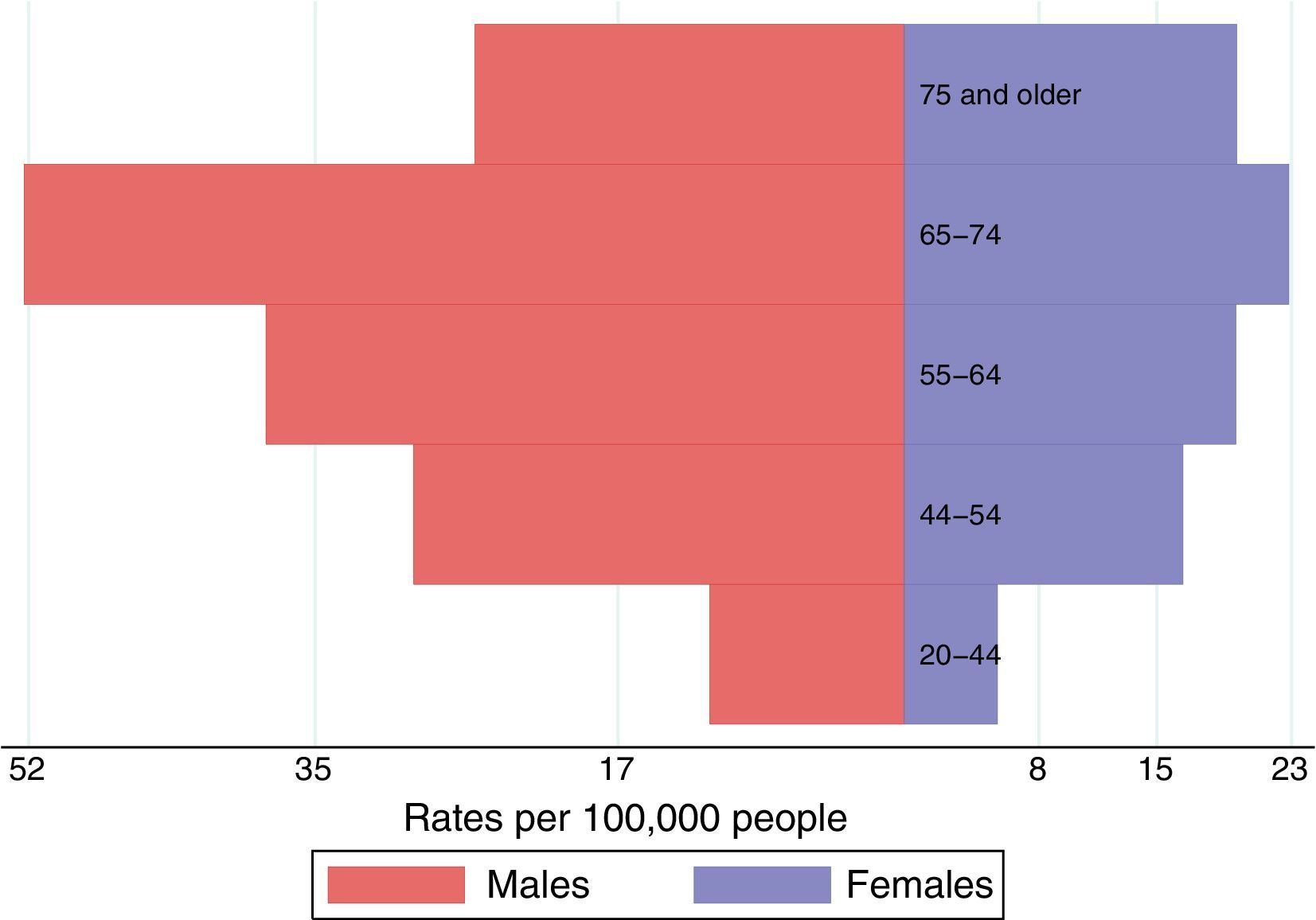
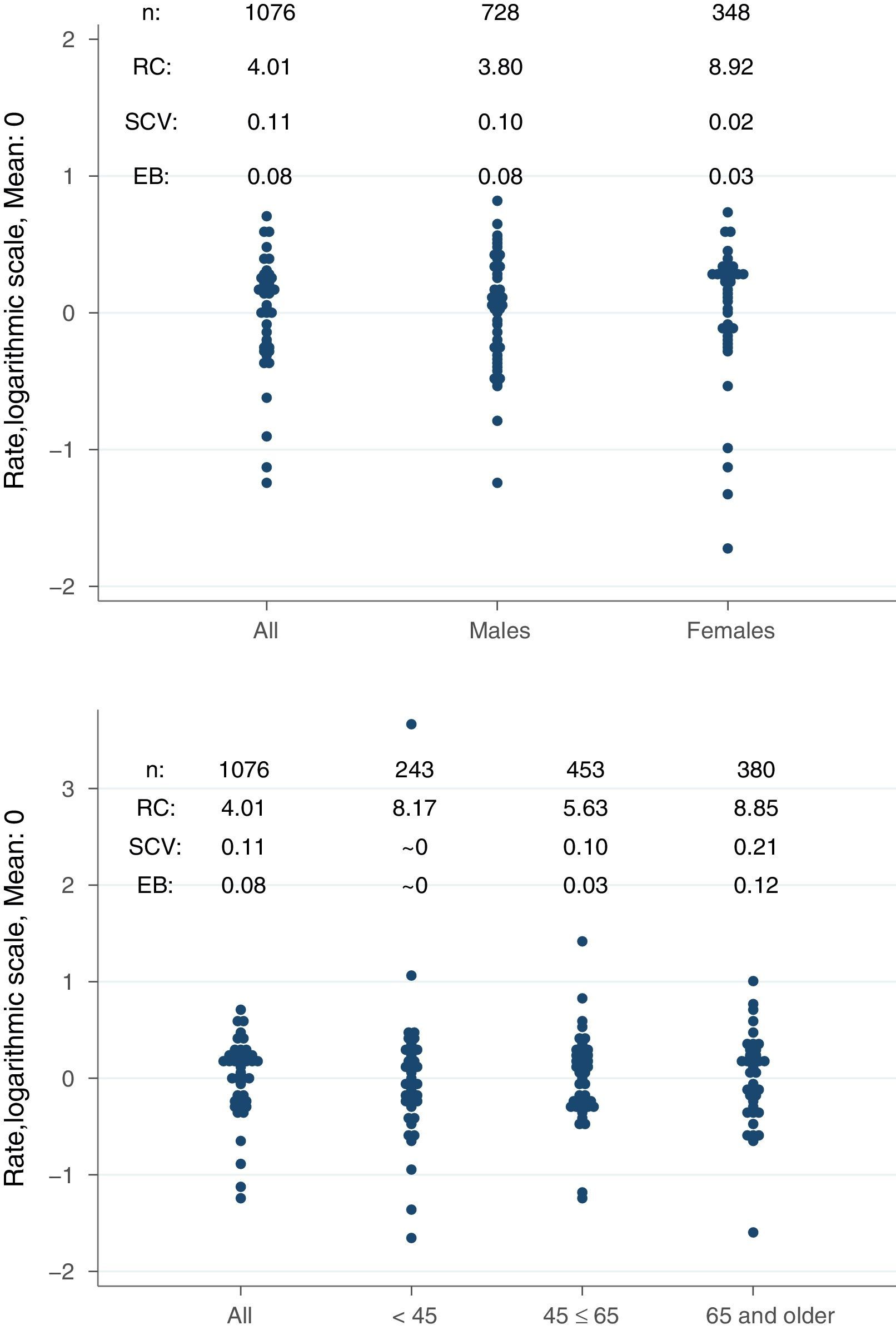
Map of RRT variations: peritoneal dialysisActivityBetween January 1, 2002 and December 31, 2012, 1076 patients started RRT using PD. 68% were men and 42% were between the ages of 45 and 65. In the period studied, the cumulative incidence rates of PD increased from 5.1 new patients per 100,000 inhabitants in the period 2002–2005 to 8.2 per 100,000 inhabitants in the period 2010–2012. In this period, PD represented 13% of incident cases of RRTs, whereas in the period 2002–2005, it was 8% of incident cases of RRTs. Fig. 3 shows the cumulative incidence rates by age and gender g.
Magnitude of variationThe difference between the areas with a highest and lowest standardised incidence rate of PD was 8 times in women and 3 times in men. By age group, the ratio was 8 times between those <45 and those >65. The statistic that quantifies the non-random variation by area showed, as a whole and over time, a value associated with a moderate variation (EB=0.08) (Fig. 4).
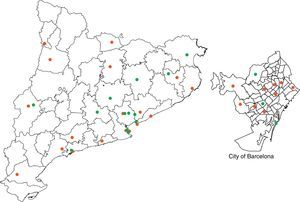
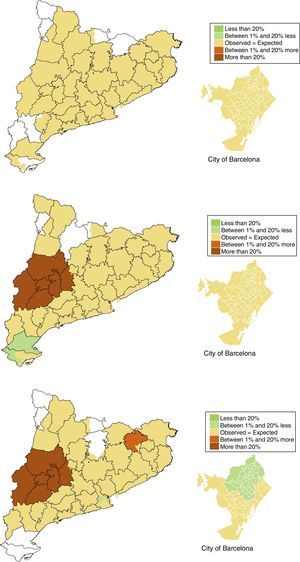
Fig. 5 shows the geographic distribution of the ratios of standardised incidence of PD by age group. The maps show a pattern of zero variation among patients <45 years, none of the areas was significantly different from the expected values in relation to the standardised rate in Catalonia. However for patients >45 years, the areas of Segrià, Garrigues, Pla d’Urgell, Segarra, Noguera and Garrotxa, in the province of Girona, have a number of observed cases 20% greater than the expected values calculated from the standardised average rate in Catalonia.
The effect of existence of a dialysis centre or nephrology care unit in the area was also analysed. The results showed that there was no significant association with the number of PD cases in these areas.
Atlas of RRT variations: kidney transplantActivityBetween January 1, 2002 and December 31, 2012, 4750 patients received RT; a 76% had been treated with HD previously; 62% were men and 49% were 45–65 years old. The percent of patients that were on PD as prior to RT doubled, from 6.2% in 2002 to 14.4% in 2012. Likewise, the percentage of patients who received an early RT rose from 6% in 2002 to 13.8% in 2012. The percentage of living donors RT also increased from 2.1% in 2002 to 16.7% in 2012.
The percentage of patients receiving a RT compared with the total number of patients on RRT increased from 43% in 2005 to 54% in 2012.
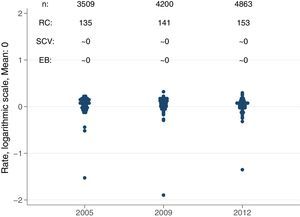
Magnitude of variationThe difference between the areas with a highest and lowest standardised prevalence rate of RT was 40% (RC25–75=1.4). The statistic parameter that quantifies the non-random variation by area showed, over time, a null value associated with a significant variation (EB≈0).
Given the low incidence of RT as the first RRT, it was considered more appropriate to work with the prevalent cases in 3 years. Therefore, 3 cut-offs were used in the study to explain the percentage of RT in relation to the total RRT prevalent in 2005, 2009 and 2012. In the maps the pattern was homogeneous, with minimal differences between regions (Fig. 6).
DiscussionDespite the increase in the incidence of PD as the first choice for RRT, there is an relatively low use of PD as compared with the most recent data from the Spanish registry3 and from the European Renal Association-European Dialysis & Transplant Association (ERA-EDTA).19
The indication of PD and early RT as the first RRT is more frequent in patients <45 years of age. In this age group, the incidence of PD is three times greater than in >65 years and it is 50% higher than in patients 45–65 years of age.
No significant region-related variability was observed in incident cases receiving HD as the first RRT option; the same can be said about RT. All this leads us to believe that in our entire community there is a balanced equity to access RRT.
However, it was observed region-related variability in the indication of PD. The areas of Lérida and Garrotxa (in Girona) show a higher incidence of PD as compared with the median incidence in Catalonia.
Similar results have been observed in other countries where the use of HD and PD may show region-related variations, which seem to be related to the development of specific programmes by Nephrology Services.11 We believe that similarly to what has been observed in other countries the variability in the use of the different modalities of RRT, specific programmes generated by the nephrologist are making a difference. Other factors such as associated comorbidities or patients’ age, or even the organisational model of care or the ownership of the centres do not explain the region-related variations. All centres that offer HD are either publicly or private. The centres that perform RT are public. The centres that offer PD are public, but agreements are made with suppliers that provide the materials needed to perform PD, either continuous ambulatory peritoneal dialysis (CAPD) or automated peritoneal dialysis (APD).
To reduce the region-related variability in PD, it would be advisable to increase its indication in the rest of the areas so the PD reach levels similar to Lérida and Garrotxa in Girona.
To reach such objective, several aspects should be improved. First, it is necessary to develop or refine existing support tools that help to make shared decision about the most suitable choice of RRT. This decision has to be shared by the various actors—doctors, nurses, health officials—and the patients themselves and their families. It is important to consider the patients’ preferences, and to maintain and improve their quality of life as much as possible. The patients must have access to objective, regulated, understandable and detailed information on the different methods of RRT; this is essential when deciding on the RRT method. An informed and reasoned choice made by patients must be a fundamental element in the decision.
Second, further training of resident and fellows doctors should be enhanced, as well as maintaining and improving the ongoing training of health professionals working with CKD and PD, either in a centre itself or at centres with a PD programme. Third, the adoption of PD as the first RRT method should be promoted, with incentive-based reimbursement in contracts with different suppliers.
Finally, it would be desirable to analyse other potential types of region-related variability, such as the time needed to access the RT waiting list, or to analyse whether there are differences in access to RT depending on areas of residence. In Catalonia, the CTO is working in a comprehensive way to organise the proper management, uniformity and dissemination of all sources of information. This task will help to obtain data to evaluate and propose different actions and road maps.
In addition, the rates of patients >80 years in RRT have increased significantly in recent years.2,3,19 The current volume of cases is still insufficient to conduct a variability study in this population which will undoubtedly be of interest in future studies due to the fragility and complexity of this subgroup of patients.
Lastly, the results of this study may be affected by some limitations related to the quality of the data sources and by the usual limitations of the ecological design, limitations which affect the causality of the relationships observed and their transference to the individual level.20
In conclusion, there has been a notable increase in PD and early RT indications, but the rates for PD are still below the average for Spain and Europe. The variability is similar to that observed in other countries; it is worth to mention the regional variations in PD in Catalonia.
Conflicts of interestThe authors declare that there are no conflicts of interest.
We would like to thank all the members of CRRP's Advisory Committee: Higini Cao (Hospital del Mar), Joan Manuel Díaz (Fundació Puigvert), Alberto Martínez Castelao (Hospital Universitario de Bellvitge), Albert Martínez Vea (Hospital Joan XXIII de Tarragona), Francesc Xavier Moreso (Hospital General Vall d’Hebrón), Joan Fort (Hospital General Vall d’Hebron), Aleix Cases (Hospital Clínic), Enrique Lara (Hospital Materno-Infantil Vall d’Hebron), Maribel Troya (Hospital Germans Trias i Pujol), Martí Vallès (Hospital de Gerona Josep Trueta), Elvira Fernández (Hospital Arnau de Vilanova de Lérida).
Please cite this article as: Tebé Condomí C, Arcos E, Comas J, Espallargues M, Pons JMV, Díaz JM, et al. Atlas de variaciones sistemáticas en el tratamiento sustitutivo renal en Cataluña (2002–2012). Nefrologia. 2017;37:164–171.