To the Editor,
Post-infectious acute glomerulonephritis can be manifested as a nephritic syndrome. Macroscopic haematuria (MH) is self-limited and appears in more than half of cases. Kidney failure is due to inflammatory glomerular lesions. On the other hand, some patients with MH as a symptom of IgA nephropathy can undergo certain worsening of renal function due to tubular mechanisms.1 Recently, nephropathies other than IgA have been reported (vasculitis, Goodpasture syndrome and others) in which kidney failure is not only due to glomerular damage but also tubular lesions caused by intraluminal haematic casts.2
We describe the case of endocapillary proliferative glomerulonephritis with haematuria and renal failure and glomerular lesions and intratubular haematic casts.
A 38-year-old female, subjected to laryngeal polypectomy 20 days before, with odynophagia and fever. Three days before being admitted, she felt general discomfort, an itchy rash, haematuria, followed by anuria. Physical examination: blood pressure 98/51mm Hg; pointed exanthema was resolved; other aspects were normal. Biochemical tests showed: hypochromic anaemia, with no haemolysis data. Creatinine: 8.1mg/dl; urea: 166mg/dl; protein/creatinine ratio: 1.3g/g and sediment with uncountable red blood cells. Normal immunoglobulins. Negative antinuclear antibodies (ANA), anti-DNA, C3, C3, C4 and antistreptolysin O (ALSO) antibodies. Normal chest ultrasound.
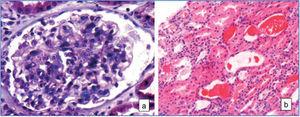
Given that renal function rapidly deteriorated, he received steroid treatment (in bolus and orally [p.o.] and haemodialysis). The renal biopsy found: 17 glomeruli, diffuse endocapillary hypercellularity and neutrophils in capillary lumens, epithelial crescents in two glomeruli. Interstitial space with frequent haematic casts and epithelial space with denudate haematic casts (Figure 1). Immunofluorescence, mesangial deposits and in capillary walls of C3 and IgM (endocapillary proliferative glomerulonephritis).
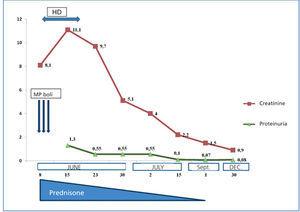
The patient progressed favourably, as shown in Figure 2, and renal function fully recovered.
Our patient therefore had an acute endocapillary glomerulonephritis, possibly post-infectious, discovered with macroscopic haematuria and acute kidney failure. For most renal biopsies, the key areas of study are the interstitial and tubular spaces, and they are analysed in detail. However, it is necessary to seek the presence of intratubular haematic casts as the cause of tubular necrosis, which can add to massive extracapillary proliferation or vasculitis. In our case, glomerular lesions justify acute renal failure, but tubular necrosis, given the advanced stage, has possibly played a more important role.
The physiopathology of the renal function disorder in MH patients is not fully understood, especially if we take into account the fact that not all haematuria episodes are associated with acute renal failure. Iron and haemoglobin poisoning, together with tubular obstruction are the main mechanisms,3,4 favoured by protein expression induced by intratubular-free haemoglobin, by tubular lesions,5 and sometimes by association with interstitial nephritis.6 Praga, at al1 described the relationship between acute tubular changes and the percentage of haematic casts and MH duration, although other mechanisms may exist, such as the presence of necrotising glomerular or extracapillary proliferative lesions2,7 as possible triggers of AKF in the MH episode.
Progress is favourable by stopping macroscopic haematuria3,6; however, some patients benefit from steroids if they have prolonged haematuria, are over 50 years of age, or have had previous kidney damage.8 Immunosuppressive drugs are not recommended, unless a massive extracapillary proliferation or signs of acute vasculitis coexist.
In summary, MH in cases of glomerulonephritis different to IgA can become complicated with acute failure due to tubular necrosis and intratubular haematic casts. Its pathogenesis is not fully known and it seems that steroids may be effective in the most serious cases.
Figure 1.
Figure 2.