To the Editor,
Libman-Sacks endocarditis is the most classic heart disorder associated with systemic lupus erythematosus (SLE) and is a serious cause of morbidity and mortality. For some patients undergoing peritoneal dialysis (PD) lupic activity markers remain positive after having started treatment, with accompanying clinical symptoms, especially serositis or vasculitis.
We present the case of a 46-year-old female, affected by advanced type IV lupus nephropathy, undergoing a PD programme since February 2009. Since then, she has presented with positive markers. She was suffering flare on her skin and joints, and received sodium mycophenolate at a dosage of 180mg and prednisone at 5mg daily. She is on the waiting list for a kidney transplant. The only PD complication that she experienced was an episode of peritonitis, in June of the same year.
She was admitted because of dyspnoea and general progressive discomfort, which had lasted for 15 days. During the last days she had chest pain in the left hemithorax, which increased when she breathed deeply and improved relatively in anteversion. She did not have a fever or any other clinical symptoms.
In the physical examination, a diastolic murmur was found in the aortic area, which extended to the carotids, with a significant pericardial friction, but there were no signs of heart failure. The rest of physical examination was normal.
The biochemical tests found: leukocytes: *21.3K/µl (4.4-11.3), band cells: 3%, neutrophils: * 92.0% (50-70), lymphocytes: * 3.0% (25-40), C-reactive protein (CRP): * 17.73mg/dl (0.1-0.5), procalcitonin: * 4.84ng/ml (<0.5). Antinuclear antibodies (indirect immunofluorescence [IIF]): 320-640 u arb (0-80), anti-DNA antibodies (enzyme immuno-assay): 1.3ml (<10IU/ml), anti-DNA antibodies (IIF): 80-640 u arb (0-80), cardiolipin antibodies (IgG): 3.5IU GPL/ml, IgM: 2.5IU GPL/ml (negatives), C3: 118mg/dl (79-152), C4: 24.4mg/dl (16-38), urea 127, creatinine: 8.46mg/dl; haemoglobin (Hb): 9.6g/dl, haemocrit: 29%. Cephalin time test: 27.9/30 seconds (29-31s), positive lupus anticoagulant.
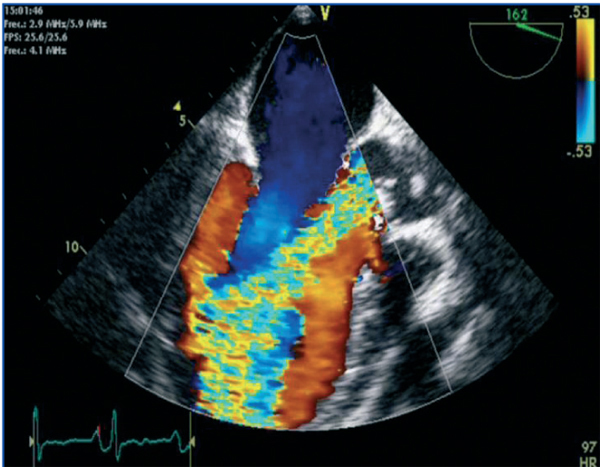
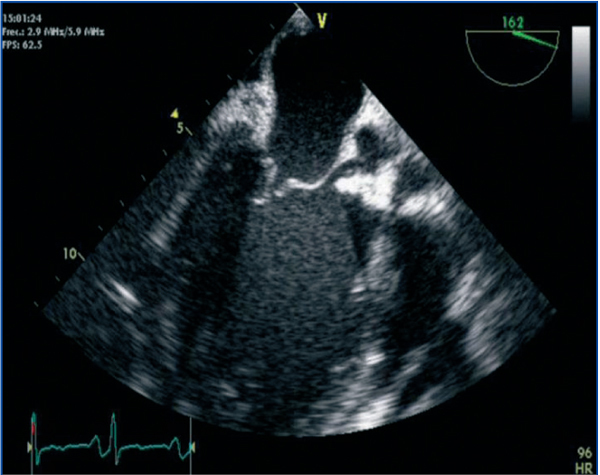
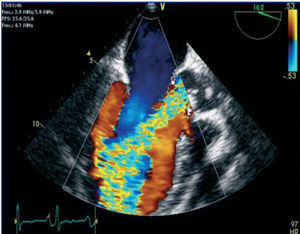
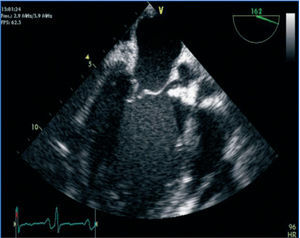
A cardiac ultrasound was performed, showing massive aortic regurgitation (AR) with a preserved left ventricular ejection fraction (LVEF) (69%). Three vegetations were found in the aortic valve, and the largest one measured 20mm. A pericardial haemorrhage was also observed without signs of heart block or thrombi (Figures 1 and 2).
All of the blood and serum cultures were negative. Chest, abdominal and cranial computed tomography (CT) did not show any significant changes.
Daily dialysis was indicated given the evidence of pericarditis and the uraemic evidence. With the diagnosis of endocarditis and awaiting the haemocultures, treatment with empirical antibiotics was started with vancomycin + ceftazidime + gentamicin. Given the suspicion of lupus activity, the prednisone dose was increased to 60mg/24 hours and the sodium mycophenolate dose to 180mg/12 hours.
After eight days of treatment, a control echocardiogram was performed which showed that the pericardial leakage had reduced and that the severe AR was persistent, with an image of swaying vegetation. Lastly, blood cultures were negative.
Given the severity of AI, it was decided that the valve should be repaired surgically, and a mechanical prosthesis placed. The anatomopathological diagnosis of the valvular piece informed of an aortic endocarditis with no evidence of microorganisms (Libman-Sacks endocarditis). On the pericardium a fibrinous chronic pericarditis was observed.
At present, two months after heart surgery, the patient has returned to the PD programme, with no clinical signs of lupus activity, maintaining positive immunological markers and undergoing treatment with sodium mycophenolate at a dose of 180mg/12 hours and prednisone at a dose of 50mg/24 hours.
Figure 1. Massive aortic regurgitation.
Figure 2. Large vegetation adhered to the right coronary sigmoid