To the Editor,
Varicella zoster virus (VZV) infection may present with two types of symptoms: the primary infection, known as varicella, with different stages of vesicular lesions mainly on the chest, head and limbs, and subsequent reactivation that causes herpes zoster (HZ). HZ complications are most common in immunocompromised patients with a high incidence in bone marrow transplantation. It may coexist with a visceral dissemination, which is difficult to diagnose if it is not associated with usual skin lesions. Therefore, delayed treatment is associated with high morbidity and mortality, mainly caused by respiratory distress syndrome, fulminant liver failure, pancreatitis or meningoencephalitis.4,5
We present the case of a 79-year-old male with antineutrophil cytoplasmic antibodies (p-ANCA). He was diagnosed in 2004 with alveolar haemorrhage and nephritic syndrome treated with corticoids and cyclophosphamide; chronic kidney failure (started haemodialysis in 2006); pulmonary bleeding secondary to a disease flare that was treated with corticoids and cyclophosphamide in 2008; and subsequent maintenance treatment with prednisone at 5mg/day combined with sodium mycophenolate mofetil (MMF) at a dosage of 180mg/12 hours. This treatment is maintained to date. Vesical transurethral resection in 2009 due to vesical neoplasm and atrial fibrillation. His usual treatment was: acetylsalicylic acid 100mg, bisoprolol 2.5mg/24 hours, omeprazole 20mg/24 hours, calcium carbonate 2.5g/24 hours, dacortin 5mg/24 hours and MMF 180mg/24 hours. He was administered Eprex 2000 and weekly Venofer during haemodialysis.
He went to the emergency department with dyspnoea of several days of evolution, coughing and slight expectoration, together with abdominal pain that was variable in intensity. He had nervous fever, but no other symptoms of interest and was sent home. He came to the emergency department again four days later, being referred to our hospital. He had the same clinical symptoms and in the physical examination presented with vesicular lesions limited to the abdomen on dermatomes D9, D10 and D11, which appeared two days later. He had blood pressure of 80/40mm Hg, basal oxygen saturation of 84%, tachypnoea, pain upon deep palpation in the right hypochondrium and intercostal muscle strain. Wheezing could be noted on both sides until the middle fields during auscultation. When he was admitted, the biochemical and radiological data were:
1. Haemoglobin (Hb): 11.7g/dl; leukocytes: 4200 (N: 91.4%, L: 5.3%); platelets: 77 000.
2. Aspartate transaminase (GOT): 6926IIU/l; alanine transaminase (GPT): 3587IIU/l; amylase: 100IIU/l; lactate dehydrogenase (LDH): 1995IIU/l; creatine kinase (CK): 152IIU/l; myoglobin: 708IIU/l; creatinine (Cr): 6.3mg/dl; urea: 88mg/dl; K: 6nmol/l; Na: 144mmol/l; total bilirubin: 2.17mg/dl.
3. pH: 7.21; CHO3: 12mEq/l; pCO2 : 32mm Hg; pO2 : 59mm Hg.
4. International normalised ratio (INR): 1.7; prothrombin activity: 37%; fibrinogen: 663mg.
5. Chest X-ray: Bilateral interstitial and alveolar pattern with peripheral disposition and cotton-wool like distribution that does not improve following ultrafiltration (Figure 1).
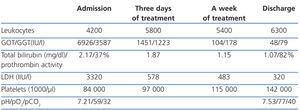
Given that the patient was immunocompromised, and data supported liver failure and acute respiratory failure with skin conditions, VZV was highly probable. We decided to request a serology test for atypical cells; it was VZV-positive, so empirical treatment with acyclovir was started at a dosage of 250mg/12 hours was started, combined with antibiotic treatment (levofloxacin 250mg/48 hours plus cefotaxime 1g/24 hours). HZ diagnosis complicated with visceral dissemination was confirmed by polymerase chain reaction (PCR) for associated viral DNA, and the remaining study was negative. The patient progressed satisfactorily with acyclovir, including clinical symptoms –recovery from respiratory failure and skin lesions–, radiological symptoms, –the interstitial and alveolar infiltration disappeared– and biochemical parameters (Table 1).
Complications secondary to VZV reactivation are common in immunocompromised patients. Data collected from bone marrow transplant patients show that incidence varies from 17% to 52%, according to different studies.5,9 For solid organ transplantation there is one retrospective study with a total of 869 patients worth mentioning, which reports an incidence of 8.6%, particularly in lung (15.1%) and kidney transplantation.3
Its clinical forms vary: local zoster with or without visceral dissemination, visceral involvement without skin lesion or generalised zoster with no visceral involvement.1,2 Reactivation takes place from the spinal ganglia; its mechanism is still fairly unknown and presents as the main cause of all forms of HZV. However, there are contradictory data regarding cases secondary to reinfection in the literature.1
As in our case, it can coexist with visceral dissemination. Between 3% and 15% of HZ reoccur.1,3 It presents a high mortality rate, with studies that show up to 55%3 in cases secondary to complications such as meningoencephalitis, pancreatitis or fulminant liver failure.5 After skin, the lung is the most affected organ, followed by the liver.1,3 Diagnosis is hindered if the skin involvement does not presents before visceral dissemination, as has been shown in a series of negative laparotomies in patients with significant abdominal pain. Three of the 123 cases presented with symptoms of HZV.7 Therefore, it can present as variable clinical symptoms with a constitutional syndrome associated with symptoms of visceral involvement, abdominal pain due to stretching of the Glisson capsule or pancreatitis, respiratory failure, etc., which is often subsequently clearer, once neuritis and vesicular exanthema –common HZ symptoms– develop.
Diagnosis requires a high clinical suspicion in those patients with previous history of non-disseminated zoster and powerful immunosuppression. Previous clinical background factors that must be highlighted are: immunosuppression, treatment with steroids and/or MMF, and previously positive serology.3 We did not know the previous serology results for our patient, but among his medical history we found significant immunosuppression due to the underlying condition, in the last stage of MMF and steroid treatment, which immunitary dysfunction caused by the very uraemic state added to.
Diagnosis in immunocompromised patients or atypical symptoms can be confirmed by different laboratory techniques, given that suspected clinical symptoms with positive serology may not be enough to confirm it. Amplification of viral DNA in the blood or vesicular fluid in cases of visceral dissemination is quick, has low contamination risk and is more sensitive than the conventional culture or direct immunofluorescence.1,6
In summary, treatment should prevent complications. Given the highly suspected clinical symptoms, specific and early treatment is recommended. Full dose acyclovir seems to be the most effective agent. Treatment duration is still not defined in the literature and it should be combined with wide-spectrum antibiotic treatment to avoid complications due to over infection.8
To conclude, visceral dissemination of HZ is a complication of a variable frequency, which has a high morbidity and mortality and requires rapid treatment management based on highly suspected clinical symptoms.
Figure 1. Chest x-ray upon admission
Table 1. Biochemical evolution