Q fever caused by Coxiella burnetti may produce acute or chronic clinical manifestation, although most cases are asymptomatic or mild.1 Acute presentation of Q fever is characterised by a sudden flu-like syndrome and high-grade fever. Nearly 1–5% of infected patients develop a chronic form, which can take place months or years after an acute infection. The most common manifestation is endocarditis, especially in immunocompromised patients or in patients with valvular heart disease. Mixed cryoglobulinaemia is rare2,3 and can be diagnosed using an immunoassay. Seroconversion is usually detected 7–15 days after the onset of symptoms. Titres of anti-phase II antigens IgG greater than 200 or Titres of anti-phase II antigens IgM greater than 50 are indicative of a recent infection, whereas titres of anti-phase I antigens IgG greater than 800 are suggestive of chronic infection. Mild forms are commonly self-limiting. Doxycycline is the drug of choice if treatment is needed. Hydroxychloroquine and doxycycline are recommended for at least 18 months for the treatment of chronic forms of endocarditis.
Our patient is a 64-year-old man from Germany who has been living in Mallorca since 2011.
History: HTN, ischaemic cardiomyopathy that underwent revascularisation (3 stents). Atrial fibrillation treated with anticoagulation. Moderate alcoholism. End-stage chronic renal disease (ESCRD) receiving haemodialysis with vascular graft access.
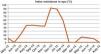
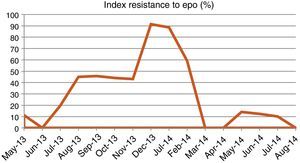
In April 2013, the patient started with fever, elevated transaminases (GPT 124, GOT 114, and GGT 100), and positive CMV IgM. Following 2 weeks of treatment with ganciclovir, the fever abated but the inflammatory parameters remained high (CRP 9.24 and PCT 12.48). Fever recurred subsequently and neutropenia (up to 1150mcl), anaemia refractory to erythropoiesis-stimulating agents (ESA) (Fig. 1), and thrombocytopenia were associated. Ganciclovir was administered for 3 weeks with Rickettsia- and Coxiella-positive serologies (IgG using IIF).
Although the patient denied any animal or tick bites, treatment with doxycycline (100mg/12h) was initiated due to a suspected Coxiella/Rickettsia infection and after ruling out endocarditis using a transthoracic echocardiogram.
The patient still had fever and neutropenia seven days after treatment began. A CT scan of the abdomen and chest revealed liver cirrhosis and splenomegaly. HCV and HBV serologies were negative. Finally, Serratia marcescens was isolated in a sputum culture, and fever subsided following 5 days of treatment with ceftazidime. The patient remained without fever after 2 weeks of treatment with ceftazidime and doxycycline.
Fever recurred one month later (June 2013). The sputum culture and haemocultures were negative, while Rickettsia and Coxiella serologies remained positive (phase 1 IgM and IgG and phase 2 IgM and IgG [1/512; 1/2056, respectively]). Hypergammaglobulinaemia was observed with an IgG kappa monoclonal component, and serologies were read as false positives in the context of hypergammaglobulinaemia, which is why patient was not treated. The patient developed apparent purpura in the lower limbs soon after and cryoglobulins containing polyclonal Ig and monoclonal IgG kappa (essential mixed cryoglobulinaemia) were positive. After ruling out haematological neoplasia (a bone marrow biopsy revealed no signs of multiple myeloma) and HBV/HCV as potential causes, serology tests for Coxiella were requested, and the results – IgG (phase 2)>1/4092, IgM (phase 1)>1/64, IgG (phase 1)>1/4092 – were consistent with chronic Q fever. Endocarditis was ruled out and treatment with doxycycline 100mg/day and hydroxychloroquine 200mg/day was initiated. The fever abated and the patient had a favourable outcome.
Symptomatic Q fever is common among adult male patients such as ours. Despite the sudden onset of fever without a focus, which is typical of acute forms, recurrence of symptoms following withdrawal of doxycycline was rather suggestive of chronic Q fever.
Endocarditis is the most common presentation, particularly among immunocompromised patients or patients with valvular heart disease. And yet, surprisingly, endocarditis was ruled out in our patient, who was immunocompromised as a result of his baseline comorbidity (ESCRD undergoing haemodialysis) and neutropenia.
Hepatitis and cirrhosis are also common. In our patient, who had a history of moderate alcoholism, transaminasaemia had remained normal before he developed his condition. Liver cirrhosis and splenomegaly were observed in the CT scan, and Q fever may have been a contributing factor.
Anaemia and thrombocytopenia may also occur. Our patient already had nephropathy-related anaemia which was initially refractory to EEAs, probably as a result of Q fever.
Finally, the diagnosis of Q fever was reinforced by the finding of type II cryoglobulinaemia (mono-polyclonal) in the absence of the hepatitis C virus or haematologic neoplasia, as it is one of its potential manifestations.4,5
Our patient started treatment with doxycycline and hydroxychloroquine and so far, after 18 months of treatment, the fever has not recurred and the anaemia has resolved, even without EEAs.
In conclusion, the patient described here is a case of chronic Q fever with blood, liver, and skin involvement, together with secondary cryoglobulinaemia.
Please cite this article as: Allende Burgos N, Calls Ginesta J. Anemia resistente y crioglobulinemia mixta en paciente en hemodiálisis en contexto de fiebre Q. Nefrología. 2015;35:586–587.