Catheter-related infections are a common and clinically relevant in peritoneal dialysis patients. Exit-site infections are characterized by the presence of purulent discharge, with or without local. The most common pathogens are Staphylococcus and Gram-negative bacteria; however, rapidly growing atypical mycobacteria (RGAM) are rare.
Here we describe a paediatric patient with a Mycobacterium fortuitum peritoneal catheter exit-site infection together with literature review.
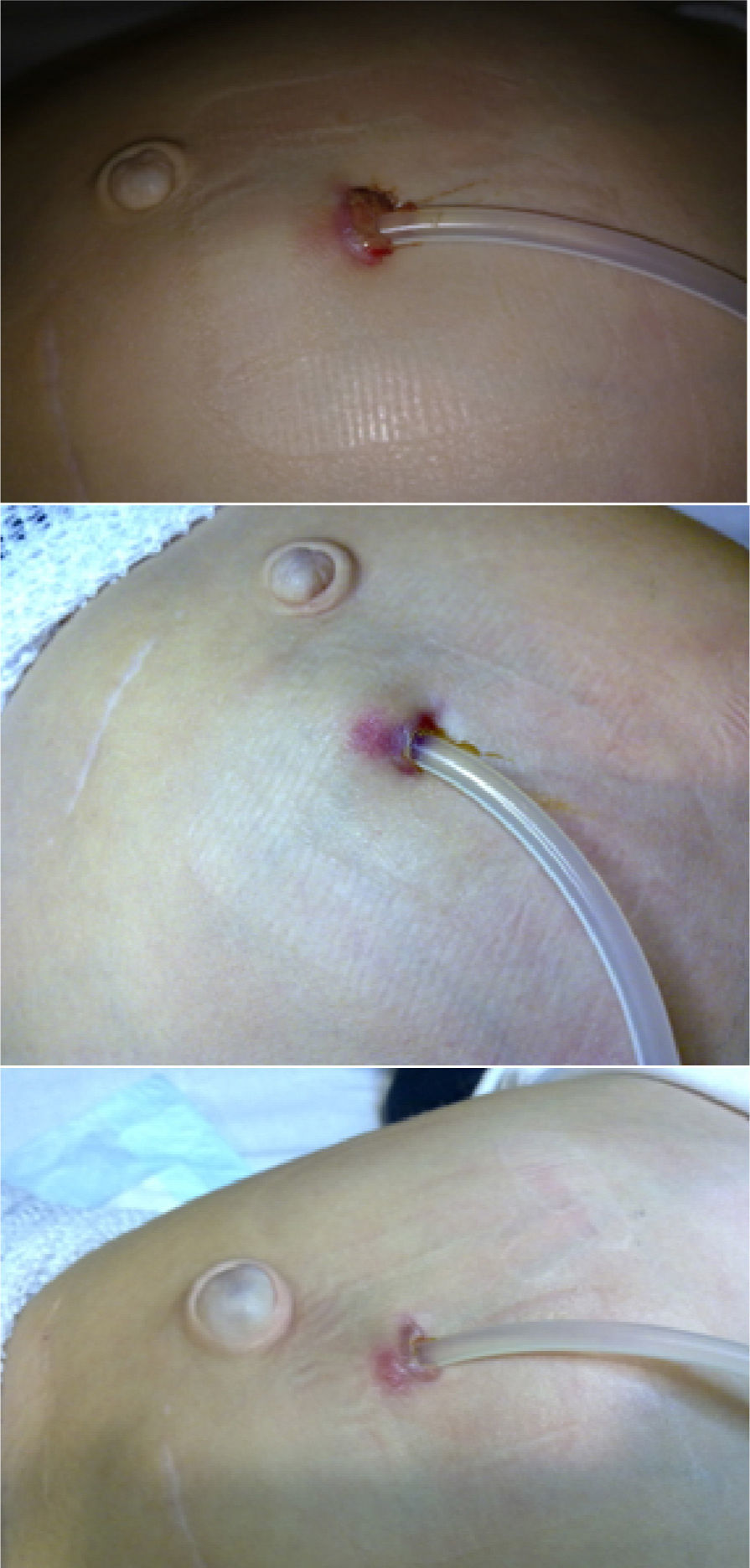
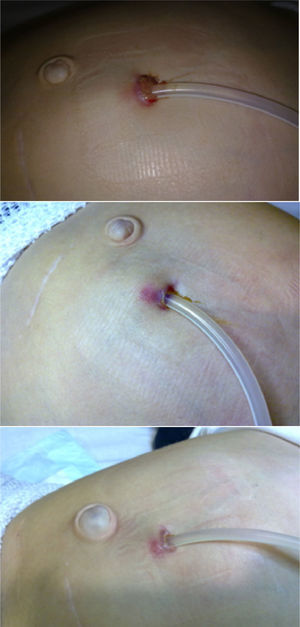
He is a 4-year-old boy with a 4-month history of continuous ambulatory peritoneal dialysis (CAPD). He complained of erythema in the peritoneal catheter exit site, with mild discharge and no improvement following 7 days of treatment with topical mupirocin. After sampling for exudate culture, topical therapy with ciprofloxacin was initiated. Six days later the erythema was still present and the patient developed a chocolate-coloured discharge and a granuloma was observed (Fig. 1). The patient was asympyomatic with no fever. Blood chemistry did not show an increase in acute-phase reactants, and cytochemistry of peritoneal fluid was normal. Previous culture was positive for RGAM. Intraperitoneal ciprofloxacin and amikacin were initiated, together local care of the exist site with Betadine®. The Mycobacteria was subsequently classified as Mycobacterium fortuitum sensitive to both antibotics, ciprofloxacin and amikacin. Treatment was continued for 8 weeks and culture became negative, with low improvement of the exit site appearance (Fig. 1). Thus, it was decided to replace the Tenckhoff catheter, despite no evidence of peritonitis. The patient continued under CAPD with no acceptable ultrafiltration. The patient was naïve to systemic antibiotics and had no history of previous infections before this episode.
The incidence of RGAM infections has increased during the last years, this group of Mycobacteria is widespread, and without nutrients and over wide-ranging temperatures. The most prevalent RGAMs involved in human infections include: M. fortuitum, Mycobacterium chelonae, Mycobacterium mucogenicum, Mycobacterium abscessus, and Mycobacterium marinum,1 with the first two most commonly resulting in peritoneal dialysis catheter infections.
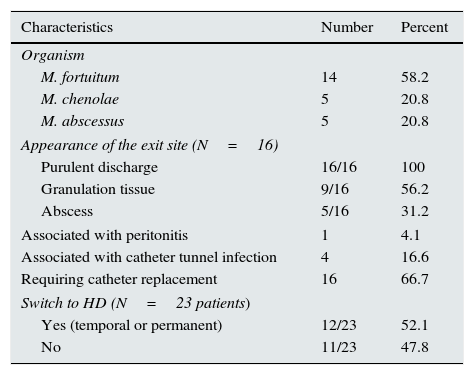
We have found twenty-three cases reported of RGAM infections of the peritoneal catheter exit site were identified in 10 English and Spanish articles published between 1990 and 2011,2–11 including a paediatric patient.2 The most common microorganism, as in our patient was M. fortuitum, followed by M. chenolae, and M. abscessus. Infection was associated with peritonitis in one patient and with the infection of subcutaneous tract in 4 patients (Table 1).
Characteristics of patients on peritoneal dialysis with exit-site infection by rapidly growing non-tuberculous mycobacteria (N=24).
| Characteristics | Number | Percent |
|---|---|---|
| Organism | ||
| M. fortuitum | 14 | 58.2 |
| M. chenolae | 5 | 20.8 |
| M. abscessus | 5 | 20.8 |
| Appearance of the exit site (N=16) | ||
| Purulent discharge | 16/16 | 100 |
| Granulation tissue | 9/16 | 56.2 |
| Abscess | 5/16 | 31.2 |
| Associated with peritonitis | 1 | 4.1 |
| Associated with catheter tunnel infection | 4 | 16.6 |
| Requiring catheter replacement | 16 | 66.7 |
| Switch to HD (N=23 patients) | ||
| Yes (temporal or permanent) | 12/23 | 52.1 |
| No | 11/23 | 47.8 |
Predisposing factors described are: immunesupression, peritonitis resistant to several cycles of antibiotic, surgery, accidental trauma, or injections.
Auramin or Ziehl-Neelsen staining techniques reveal the acid-alcohol resistance of mycobacteria. A culture should be made in 2 specific media: a solid egg-based medium (Lowenstein-Jensen) and a liquid medium allowing for automated reading (MGIT, MB/BacT, ESP). Colony growth usually occurs within 7 days and is identified by means of faster and more accurate phenotyping (biochemical tests) and genotyping systems, based on the detection of species-specific DNA sequences.
RGAMs are relatively resistant to standard disinfectants and are able to generate biofilms to survive. Consequently in many cases, peritoneal catheters must often be removed or replaced. In our literature review the dialysis catheter was replaced in 65.2% of patients. The catheter was also removed in all cases showing peritonitis or tunnel infection, patients with M. abcessus infection, and 80% of M. chenolae infections. More than 50% of patients had to be on haemodialysis.
In light of the extensive variability reported in terms of antibiotic resistance, species should be accurately screened in vitro for sensitivity to certain antibiotics so a right therapy can be established. Medium microdilution is recommended for determining sensitivity; a faster commercial technique, E-test, has been introduced in recent years, with an outstanding correlation with the reference method. An empirical therapy may include a combined therapy with aminoglycosides (amikacin), macrolides (clarithromycin and azithromycin), and fluoroquinolones (although M. chenolae and M. abscessus may be resistant to the latter). Optimal treatment duration has not been established yet, but ranged from one to six months in our literature review. One case was cured after withdrawal of topical gentamicin, which had been administered for 7 weeks, and required no further antibiotic treatment.10
In conclusion RGAMs should be suspected in catheter infections or peritonitis with negative cultures so as to prevent a delay in diagnosis and decrease associated morbidity. A large number of patients require replacement or removal of the Tenckhoff catheter and should be switched to haemodialysis.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Martínez López ÁB, Álvarez Blanco O, Ruíz Serrano MJ, Morales San-José MD, Luque de Pablos A. Mycobacterium fortuitum como causa de infección del orificio del catéter de diálisis peritoneal. Caso clínico y revisión de la literatura. Nefrologia. 2015;35:584–586.