IgA nephropathy (IgAN) is known to be the most common cause of glomerular disease and the clinical course is variable ranging from microhematuria and isolated proteinuria to acute renal failure (ARF) or rapidly progressive GN. IgAN often presents with ARF due to tubular necrosis (ATN)1; however, biopsy findings of eosinophilia, tubulitis, and interstitial eosinophils, which are typical of acute interstitial nephropathies (AIN), and its association with the use of iodinated (IC) contrast media, are exceptional.
Therefore, we believe that renal biopsies (RB) should be performed in ARF, even when its cause appear to be clear, as with the use of IC. In our case of ARF, the starting point was a case with typical presentation of ATN resulting from IC; yet, the RB showed overlap with a severe form of IgAN and severe tubulointerstitial damage.
A 73-year-old male patient, with a history of high blood pressure, diabetes mellitus (DM), normal renal function (RF), serum creatinine (SC): 1.0mg/dl, and urine without abnormalities.
A month before consultation he had undergone embolization of a giant bi-lobulated aneurysm of the anterior cerebral artery, requiring intravenous IC. Five days later, he developed progressive impairment of RF with SC: 1.6mg/dl, eosinophilia: 7.90cells/mm3, and persistent microhematuria. The ultrasound revealed normal kidneys, and autoimmunity tests were negative. RB was not considered because of fever of unknown origin and negative blood and urine cultures. Empirical treatment with steroids 1mg/kg was started, resulting in a rapid decrease of SC levels.
RF was progressively impaired in subsequent controls, resulting in SC: 2.3mg/dl, microhematuria: 50–60 red blood cells/field, proteinuria: 0.8g/24h, without eosinophilia at 15 days; and so readmission for RB was decided.
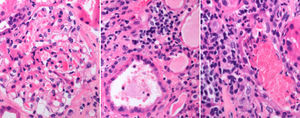
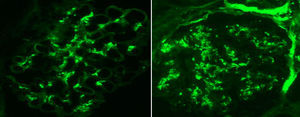
Renal biopsy showed glomeruli with an increased mesangial matrix and cell proliferation. Tubules had severe tubulitis, signs of ATN with epithelial flattening and loss of brush border, and extensive interstitial inflammatory infiltration with the presence of eosinophils (Fig. 1). Immunofluorescence revealed granular deposits of IgA and C3 within the mesangium (Fig. 2).
The patient was diagnosed of IgAN with severe acute tubulointerstitial involvement suggestive of AIN. Treatment with prednisone 1mg/kg/day was initiated, and renal function stabilized although SC levels did not return to baseline after 2 months of follow-up (SC: 2.2mg/dl).
From nephrologist's perspective, RB is an essential procedure with well-established indications for the study of variety of renal diseases. It confirm the diagnoses, determine prognosis, and helps to stabilize the right treatment. It is most commonly used in cases of nephrotic syndrome, abnormal urine tests, and unclear ARF. Our patient is a real example of the importance of confirming clinical suspicions with histological findings of RB. IgAN is the most common primary renal disease, but it can also progress to some form of “superimposed” glomerulonephritis (GM) in patients with diabetic nephropathy who develop ARF of any cause. In the series of Castellano et al., IgAN, together with membranous GM and vasculitis, were the most common non-diabetic conditions found in RBs among these patients.2 This has led to a discussion over the role of abnormal synthesis and the degradation of glomerular basement membrane and mesangial matrix which is characteristic of these cases, with haemodynamic factors and nonenzymatic glycosylation being typical of DM.3
The association of IgAN with ARF and IC media is also common since hypersensitivity reactions result in changes in T cell receptors and cytokine release, thereby activating cell and humoral immunity. These findings would account for the link between AIN and the use of IC. Nonetheless, their actual prevalence is underestimated by their confirmatory diagnosis, because of the bias against performance of RBs in most patients with ARF.4 AIN is well-known to benefit from early treatment with steroids. González et al. studied the outcome of 61 patients diagnosed with drug-induced AIN by RB5: 85% received steroids and achieved final improvement of RF and decreased need of dialysis.
Presentation and outcome in this patient with AIN and IgAN illustrates the importance of RB among patients with ARF of uncertain etiology. This leads to early initiation of the appropriate treatment to improve prognosis for our patients and it also provides important clinical information in patients with poor outcomes (Figs. 1 and 2).
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Valdenebro M, Marques M, Rubio E, Palomino E, García E, Fernández J, et al. Nefropatía IgA asociada a nefritis intersticial aguda tras administración de contraste yodado. Nefrologia. 2015;35:582–584.