To the Editor,
Chronic kidney disease (CKD) is an important issue for public health, given its high incidence, prevalence, morbidity and mortality, and socio-economic cost.1
In Spain,2 the prevalence of replacement renal therapy is 986 patients per million population (pmp), which means that approximately 45 000 people need extrarenal clearance or have received a kidney transplant. CKD is much more prevalent in earlier stages, and is associated with a poor prognosis, given the increased risk of premature death caused by cardiovascular disorders and the risk of kidney disease progressing. If this were to occur, replacement renal treatment is needed.
The prevalence of CKD at stages 3b and 4 is 1.38%,3 presenting a greater risk of death, cardiovascular disease (CV), CV morbidity and mortality, greater cognitive deterioration and worse quality of life.4
CKD treated at early stages progresses to a lesser extent and presents with less CV complications. Therefore, the public health system should advocate for an early CKD detection and treatment.
We saw World Kidney Day (WKD) as the perfect opportunity to assess CKD prevalence and its associated vascular risk in a non-selected population in the Galician city, Ourense.
We spontaneously studied a non-selected population that attended the WKD marquee in the city centre. The following measurements were taken: anthropometrics, blood pressure (Omron®), glucose (Reflotron®) and creatinine (Reflotron®) rates, intima-media thickness (IMT) measured by ultrasound of the supra-aortic trunks (LOGIQ, 12MHz probe), taken from the posterior wall and from an area free from atheromatous plaques. An arteriosclerosis score was used (AS): AS 1: ITM<0.8; AS 2: ITM>0.8; AS 3: ITM><0.8 with plaques.
Statistical calculations included mean, standard deviation and the Pearson’s regression.
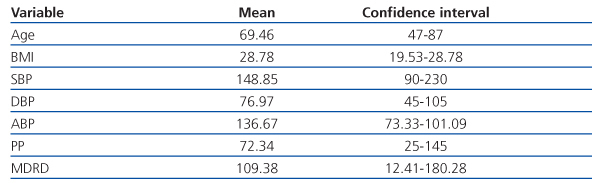
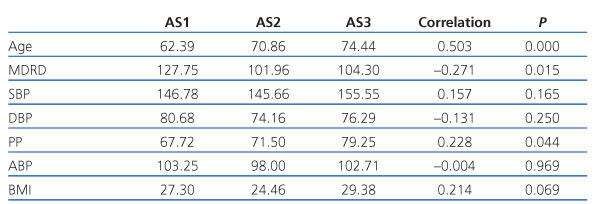
We obtained the following results: 82 people came to the marquee, 75 men (69.66 years) and 7 women (67.28 years), see Table 1. Average MDRD was 109.38 (12.4-180), the percentage of MDRD<60ml/min was 11.9%, and the different degrees of arteriosclerosis are shown in Table 2. AS correlated with age (0.000), kidney function (0.015), pulse pressure (0.044) and BMI (0.069).
When the glomerular filtration rate (GFR) is lower than 50ml/min, inflammatory response to endothelial dysfunction (ED) is initiated, the latter being a precursor of the atherothrombotic/arteriosclerotic process. It is initiated by an increase in adhesion molecule expression, monocyte infiltration, and their activation and transformation into macrophages. When the eGFR is lower than 30ml/min, phosphorus (P) ‘retention’ is produced and fibroblast growth factor (FGF 23) activated. Through its specific binding with a receptor and Klotho, it does not only reduce the kidney’s P absorption, it also inhibits 1-alpha-hydroxylase and results in lower calcitriol synthesis.
CKD progression, the decrease in FGF 23’s phosphaturic action and lower vitamin D rate produce a situation of resistance to FGF 23’s phosphaturic action. As a result, the P’s plasmatic rate increases, which upregulates the gene that codes for PTH through a “P sensor” in the parathyroid glands. Furthermore, in this hyperphosphataemia situation, extracellular P is transported by the cotransporter Pit-1 to the intracellular compartments, and once there, it acts as an indicator of an increase in mineral nucleation expression agents.5
Deficiency in vitamin D contributes to this process, given that Th1 lymphocyte action cannot be inhibited, which continue activating and perpetuating the ED process.
To conclude, there is a high prevalence of CKD in a non-selected and spontaneous population. Arteriosclerotic disease is not only related to kidney function, but also to age and pulse pressure. Pathogenic mechanisms are well known, meaning that a change is needed. Nephrology departments, in collaboration with primary care centres should create programmes for detecting CKD and incipient vascular lesions early, so as to reduce CKD progression and cardiovascular morbidity and mortality.
Table 1. Descriptive
Table 2.