La frecuencia de embarazos en mujeres en diálisis es extremadamente baja, aunque el porcentaje de gestaciones con éxito ha aumentado a lo largo de los años, siendo, según distintas series, superior al 70%. Estos embarazos no están exentos de complicaciones tanto para la madre como para el feto, el manejo de las cuales requiere el trabajo conjunto del nefrólogo, el ginecólogo, el enfermero y el nutricionista. A día de hoy no es posible encontrar un tratamiento sistemático nefrológico y ginecológico en este tipo de pacientes. Las principales medidas que se deberían adoptar incluirían: aumento del tiempo de diálisis, mantener bajos niveles de urea prediálisis, evitar hipotensiones e hipertensión materna, así como infecciones urinarias y fluctuaciones electrolíticas. Se requiere, además, una adecuada monitorización fetal.
The frequency of pregnancy in women on dialysis is extremely low, but the percentage of successful pregnancies in this context has increased over the years, with some studies placing the survival rate above 70%. These pregnancies are not exempt from both maternal and foetal complications, and so their management requires the joint efforts of nephrologists, gynaecologists, nurses, and nutritionists. Currently, we have been unable to establish consistent systematic treatment from both nephrological and gynaecological specialists in these patients. The main changes that need to be made are: increased time on dialysis, maintaining low levels of pre-dialysis urea, avoiding: maternal hypertension and hypotension, anaemia, urinary tract infections, and fluctuations in electrolytes. Adequate foetal monitoring is also necessary.
INTRODUCTION
Pregnancies in dialysis patients are uncommon and difficult to study. These pregnancies occur in widely separated dialysis units, and so the majority of nephrologists encounter one or two pregnant patients during their time in practice.1 Fortunately, the percentage of successful pregnancies has increased consistently, but there is still a very high maternal/foetal mortality and morbidity rate as compared to the normal population.2,3 In order to achieve a successful birth, this situation requires the joint efforts of nephrologists, gynaecologists, nephrological nurses, and nutritionists.2
This article is a review of the existing medical literature regarding the management of this type of patient, the incidence of successful pregnancies, and the maternal and foetal complications involved.
FREQUENCY AND DIAGNOSIS OF PREGNANCY IN WOMEN ON DIALYSIS
Although not well documented, it is believed that the frequency of pregnancies in women on haemodialysis is on the rise, from 1% to 7%, according to the most recent publications, with different rates in different countries.2,4-7 Pregnancies are more common in women with preserved residual diuresis.8,9
The majority of patients on haemodialysis have sexual dysfunction as a result of physical and/or emotional problems.2
Fertility drops due mainly to anaemia and hyperprolactinaemia; this decrease in fertility is also associated with hypothalamic/pituitary dysfunction, which results in ovarian dysfunction and anovulatory cycles, multiple drug treatments, depression, and loss of sex drive.10,11
However, the improved efficacy of dialysis, along with corrections to anaemia due to the standardised application of erythropoietin, has improved general health in these patients, as well as their sexual function, which involves increased fertility and normal menstrual cycles.11,12
Pregnancy in these patients tends to be diagnosed late, since irregular cycles and abdominal pain are already common, and many doctors do not think immediately of pregnancy as a possible cause of the symptoms.13
Further deterioration of anaemia or apparent resistance to erythropoietin as well as hypotension episodes of unknown cause in premenopausal women should arouse suspicion of a possible pregnancy.14
Urine pregnancy tests are not very useful in these situations, even if the patient has residual diuresis. The measurement of human chorionic gonadotrophin is inexact, since this molecule is produced by somatic cells and excreted by the kidney, and so ultrasound is the only reliable method to calculate gestational age.15
RESULTS OF PREGNANCIES IN WOMEN ON HAEMODIALYSIS
The first pregnancy with a successful result in a patient on haemodialysis was described in 1971 by Confortini et al16; the patient was 35 years old.
In 1980, a case series was published in the European Dialysis and Transplant Association (EDTA) register involving 1300 women of child-bearing age, reporting a 0.9% incidence rate of pregnancies in patients on chronic haemodialysis.17
In 1994, Hou published another case series from 206 North American dialysis units. The percentage of miscarriage was 70% before 1990 and under 40% in the following years.17
The majority of case series described since 2000 reported success rates for these pregnancies over 70%.5,18-24
As regards maternal mortality, few such cases have been registered in the literature. The prognosis for the mother is good; especially in patients that start dialysis after conception.2-7
MATERNAL AND FOETAL COMPLICATIONS
Maternal complications include: miscarriage, placental detachment, anaemia, infection, premature rupture of membranes, polyhydramnios, pre-term birth, uncontrolled arterial hypertension, preeclampsia/eclampsia, haemorrhage, need for a caesarean, and maternal death.25,26
The incidence of polyhydramnios has been estimated at 30%-70%. The increased production in foetal urine secondary to urea-induced osmotic diuresis is probably the cause of excess amniotic fluid.23,24 Several studies have suggested that treatment for this complication consists of increasing dialysis doses.24
As regards preeclampsia/eclampsia, approximately 80% of women on haemodialysis that become pregnant have arterial hypertension or require anti-hypertensive medications at some point during pregnancy.3
Uncontrolled hypertension poses a serious risk to the mother, and must be quickly and adequately controlled, maintaining diastolic blood pressure below 80-90mm Hg.2,13,27 As in any other dialysis patient, the initial treatment consists of adjusting volume using ultrafiltration, but if the cause of hypertension is preeclampsia, fluid extraction could exacerbate hypoperfusion to the various organs.15
Several different types of medications are used to treat hypertension in pregnant women:
- Alpha-methyldopa is commonly used; no adverse side effects have been observed in babies, and they are relatively few in the mother: fatigue, depression, and in a small percentage of patients, hepatitis.2
- Hydralazine has been used both orally and intravenously with no problems. It is not effective as a monotherapy under oral administration, but can also be associated with first-line drugs if results are not sufficiently effective.3-28
- Beta-blockers are not used due to their adverse effects on new-borns; labetalol does not produce these effects, so it is widely used.3-29
- The experience with clonidine and prazosin is limited, and these drugs do not appear to provide any serious benefit.3-30
- Calcium channel blockers that can be used include: nifedipine, nicardipine, and verapamil. These have been used in cases of severe hypertension, and do not appear to be associated with congenital defects when used during the first trimester. Only limited experience has been gained using diltiazem. We must remember that combined therapy with magnesium can lead to severe episodes of hypotension.15,28,31
- Diuretics can be used when no other alternative exists, but must be suspended in the event of suspected preeclampsia.3 Some publications have described neonatal thrombocytopenia, haemolytic anaemia, electrolyte imbalances, and jaundice with the use of thiazides.32
- Angiotensin-converting enzyme (ACE) inhibitors, angiotensin receptor blockers (ARB) and minoxidil are contraindicated due to their adverse effects on the new born.2,33-35
As regards drugs used in hypertensive emergencies, labetalol and hydralazine are prescribed intravenously.3,36
The most common foetal complications are: restricted intra-uterine growth, acute and chronic foetal suffering, pre-term birth, respiratory difficulty in the new-born, growth in neonatal intensive care units, and uterine or neonatal death.25
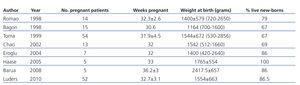
Pre-term births occur in 83% of live births; the new-borns have a low weight and the gestational age is approximately 32 weeks or even less (Table 1).5,19-24,37
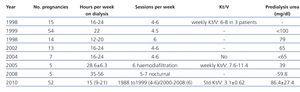
Table 2 describes the primary recommendations for managing these patients.
INTENSIVE DIALYSIS
It is well established that a longer duration of dialysis treatment prolongs the gestation period, resulting in babies with a higher weight at birth, improved life expectancy, and reduced long-term complications.3
The weekly time that patients should be on dialysis varies according to study (Table 3), but regardless of the criteria followed, the prescription of haemodialysis must be sufficient to maintain stable conditions in the mother in terms of volaemia, blood pressure, and weight gain between sessions.10
The results from the study by Hou showed that pregnant women that receive over 20 hours of dialysis per week gave birth to babies with higher weight and gestational age.3 Two studies have also shown that pregnant patients should receive the maximum possible amount of time on dialysis, at least 24 hours per week.23,38
Nocturnal haemodialysis provides greater clearance of small and medium molecular weight molecules and improves the control of metabolic, electrolyte, phosphorous, volaemia, and blood pressure profiles.21,39-42
MATERNAL UREA NITROGEN
Several retrospective studies and isolated clinical cases have reported increased new-born survival in women with blood urea nitrogen (BUN) levels <50mg/100ml, but Asayima et al, in a retrospective study involving 28 pregnant patients on haemodialysis, demonstrated for the first time that lower maternal BUN levels are associated with higher weight and gestational age at birth.37,39,43,44
Predialysis BUN levels are recommended to be kept below 50mg/100ml.2,11
TECHNIQUE
The experience with peritoneal dialysis has been limited to a very few number of patients; in fact, the incidence of pregnancies in these patients is even lower than the rates for haemodialysis patients. This could be due to the presence of hypertonic solutions in the peritoneum, previous episodes of peritonitis, or physical factors that could interfere with foetal implantation. Most of the authors do not recommend changing the dialysis technique after conception.45,46
More data are needed on the results of pregnant patients on peritoneal dialysis and the possible associated complications.46
Data from the register of pregnant patients on dialysis and several reports showed no differences in the maternal and foetal results between haemodialysis and peritoneal dialysis.27,43,47
Peritoneal dialysis has the advantage of not inducing sudden metabolic changes, and allows for a gradual control of volaemia, thus avoiding episodes of hypotension. The main disadvantage would be difficulty in maintaining proper nutrition.3
MEMBRANE TYPE AND FLOW
New dialysers, not recycled ones, with high biocompatibility and functionality are recommended in these patients.25,48
It is best to use membranes with a lower surface area combined with increased time on dialysis so as to minimise excessive fluid losses and avoid episodes of hypotension and sudden changes in osmolarity.2
Five different studies used dialysis fluid flow rates between 500ml/min and 700ml/min, and only one used low flow rates.21-23,40,49
WEIGHT GAIN
Maternal dry weight and weight gain should be regularly evaluated and adjusted according to the estimated weight of the foetus. In the first trimester, the mother should gain a minimum of 1kg -1.5kg. After this, weight should increase by 0.45kg to 1kg per week. In the third trimester, foetal weight and growth can also be directly evaluated using ultrasound.44
Maternal blood pressure and heart rate must be closely monitored before, during, and after each dialysis session.44
Ultrafiltration doses should be administered on an individual basis so as to avoid episodes of arterial hypotension, hypovolaemia, and arrhythmia; and maternal blood volume expansion and weight gain should be proportional to the gestation stage. Severe maternal weight loss due to rapid and excessive ultrafiltration can reduce the foetal-placental blood flow, which could be very harmful for the foetus. As such, these factors must be considered in ultrafiltration prescription.25
DIALYSATE
Potassium levels in the dialysate must be increased to 3-3.5mmol/l in order to avoid hypokalemia.2,3 Electrolyte levels must be checked weekly.2,3
For bicarbonate levels, Hou recommends low concentrations (25mEq/l). Based on collective experience, frequent haemodialysis can result in excessive alkali transfer to the mother, producing alkalemia.3,27,42
Frequent haemodialysis can also lead to hypophosphataemia. Given that added phosphorous in the dialysate can be a complicated issue, oral supplements are recommended, or increased dietary intake.50
With daily haemodialysis and a 3.5mEq/l dialysate calcium concentration, hypercalcaemia can develop, and so a 2.5mEq/l dialysate calcium concentration is preferred.3
ANAEMIA
In order to achieve the desired haemoglobin levels of 10-11g/100ml in these women (haematocrit: 30%-35%), erythropoietin doses must be increased by 50%-100%.25-27
In addition, anaemia during pregnancy is associated with increased incidence of pre-term births, which results in greater infant mortality rates.51
Asamiya et al analysed 24 pregnant patients on haemodialysis and demonstrated a positive correlation between maternal haemoglobin and a successful pregnancy.43
The use of erythropoietin during pregnancy has proven safe, with no documented increases in blood pressure or teratogenicity.25,52
During pregnancy, the mother and foetus need 800-1000mg of iron. Oral supplements would be insufficient, so it can be administered intravenously, without adverse effects. Frequent checks of haemoglobin and ferritin values should be performed.2
ANTICOAGULATION
Heparin does not cross the placenta and is not teratogenic. It must be used in order to avoid coagulation of the vascular accesses.3,53 This treatment should be administered to all patients, except for those with active bleeding.25
Coumarin is contraindicated in these patients.25
CALCIUM AND VITAMIN D
Physicians must take into account both the calcium provided by the dialysate and calcium intake in the form of calcium chelating agents. Daily haemodialysis with a 3.5mEq/l dialysate calcium concentration could induce hypercalcaemia, and so 2.5mEq/l concentrations are preferred, along with oral supplements of 1g-2g calcium carbonate.2
Since maternal hypercalcaemia can cause hypocalcaemia and hyperphosphataemia in the newborn and affect its skeletal development, both calcium and phosphorous levels must be monitored weekly.2,44
The placenta converts 25-OH D3 (calcidiol) into 1,25-OH2 D3 (calcitriol), and so 25-OH vitamin D must be measured every trimester, administering supplements if levels are low.3
Although primary hyperparathyroidism is known to increase the frequency of pre-term births by 10%-20%, the effects of hyperparathyroidism on the foetus are unknown. The use of 1,25-dihydroxy-vitamin D is indicated in these cases: this molecule can be used to control both hyperparathyroidism and 1,25-hydroxy-vitamin D deficiency. Calciferol does not appear to be toxic at reasonable doses. Dosage adjustments must be based on weekly calcium and phosphorous measurements.2
Sevelamer, lanthanum carbonate, aluminium hydroxide, cinacalcet, and paricalcitol have not been tested or established for use during pregnancy/lactation.54,55
NUTRITION
We recommend to:
- Increase calorie intake by 30-35kcal/day.3
- Consume 1-1.5g/kg of weight (haemodialysis) or 1.8g/kg of weight (peritoneal dialysis) of additional protein daily in order to ensure foetal development.3,8
- Take 1mg/day of folic acid starting from the first trimester.3
- Consume 1500mg/day of calcium.2
- Take water-soluble vitamins throughout the pregnancy, since the requirements for these molecules increase and intensive dialysis promotes their elimination.44
- Supplements for vitamins that can be dialysed (vitamin C, thiamine, riboflavin, niacin, vitamin B6).45
- Many patients also need increased potassium and phosphorous uptake in order to maintain adequate levels.3
OBSTETRIC MANAGEMENT
As regards tocolytic agents, intravenous magnesium must be administered with caution in these patients in order to avoid toxicity, keeping levels below 5-7mg/dl. Calcium channel blockers are also administered for this purpose.2,3,56
Indomethacin has been used successfully, especially in women with polyhydramnios. However, in women with residual renal function, this effect can be lost. Additionally, prolonged use for more than 72 hours has been correlated with severe side effects on the newborn, so it should only be used for short periods.3,57
Progesterone supplements in their various presentations have not been evaluated in haemodialysis patients or women with chronic kidney disease.58
As regards the length of the gestation period, some authors recommend inducing labour after 34-36 weeks if the baby’s lungs have developed sufficiently, but the majority prefers to prolong the gestation period to 38 weeks.3
Caesarean sections should only be undertaken under the same indications as for women not being treated with haemodialysis.3
Newborns should be monitored in high-risk units, since they are usually born with similar urea and creatinine levels to their mothers, and may suffer osmotic diuresis.2,3
Conflicts of Interest
The authors affirm that they have no conflicts of interest related to the content of this article.
KEY CONCEPTS
1. Gestation in patients on renal replacement therapy involves a risk both to the mother and the foetus, even though new-born survival has improved in recent decades; various studies and registries report survival rates of 40%-85%.59
2. We currently have no literature reference for systematic nephrological/gynaecological treatment of these patients.30,59
3. According to the available literature on the subject, the measures to be taken in order to achieve successful pregnancies in these patients include: multidisciplinary approach, increased time on dialysis, maintain low levels of predialysis urea, prevention of pre-term birth, strict control of blood pressure and electrolyte levels, prevention of urinary infections, and adequate foetal monitoring.2,3,23,24
Table 1. Parameters for pregnancy and new-borns in women on chronic haemodialysis
Table 3. Parameters for dialysis and foetal survival
11319_19157_28450_en_ref.1131912388_11319_19115_25239_es_11319_tabla_2_en.doc
Table 2. Recommendations for optimising the treatment of pregnant women on haemodialysis