Introducción: La nefropatía membranosa (NM) es la causa más frecuente de síndrome nefrótico en adultos. El diagnóstico se basa en los hallazgos típicos observados con el microscopio electrónico (ME) y el estudio de inmunofluorescencia (IF). En algunas ocasiones, sólo se dispone de tejido para estudio de microscopio óptico (MO); en estos casos puede ser complicado diferenciar entre una NM y una enfermedad por cambios mínimos (ECM). Recientemente se está extendiendo el estudio con C4d por inmunohistoquímica. Existe muy poca información sobre el depósito de C4d en la NM. Nuestro estudio consistió en analizar si el depósito de C4d realizado en la muestra en parafina podría ser útil en el diagnóstico de NM. Material y métodos: Estudio retrospectivo que incluyó a todos los pacientes diagnosticados de NM mediante biopsia renal en nuestra unidad entre enero de 2001 y octubre de 2008. Se incluyeron sólo adultos con un diagnóstico certero de NM y ECM idiopática que dispusieran de estudios con MO, IF y ME. En octubre de 2008, secciones de 3 µm de tejido renal fijado en formaldehído fueron deparafinadas y rehidratadas. Después se tiñeron mediante inmunohistoquímica con C4d usando un anticuerpo policlonal antihumano obtenido de conejo. Resultados: Se incluyeron finalmente 19 pacientes con ECM y 21 con NM. Ningún depósito de C4d fue observado en ninguno de los glomérulos de los pacientes con ECM y el 100% de estos pacientes fueron clasificados como negativos. Sin embargo, el depósito de C4d se detectó en el 100% de los pacientes con NM y en todos los glomérulos con una distribución uniforme y granular dibujando todas las asas capilares. Conclusiones: El depósito de C4d mediante inmunohistoquímica es una herramienta muy útil en el diagnóstico de NM.
Introduction: membranous nephropathy (MN) is the most common cause of nephrotic syndrome in adults. The diagnosis is based on typical findings observed using electron microscope (EM) and immunofluorescence (IF) studies. On some occasions, tissues are only available for analysis using an optical microscope (OM); in these cases, it can be difficult to differentiate between MN and minimal change disease (MCD). Recently, the use of C4d immunohistochemical staining has spread. Very little information is available regarding C4d deposits in MN. Our study consisted of analysing whether C4d staining of samples embedded in paraffin could be useful for diagnosing MN. Material and Method: Ours was a retrospective study including all patients diagnosed with MN by renal biopsy in our unit between January 2001 and October 2008. We only included adult patients with a definitive diagnosis of MN or idiopathic MCD by OM, IF, and ME studies. In October 2008, 3µm sections of renal tissue fixed in formaldehyde were removed from paraffin and rehydrated. The samples were then stained for C4d immunohistochemical analysis using anti-human polyclonal antibodies obtained from rabbits. Results: Our study included a final sample of 19 patients with MCD and 21 with MN. No C4d deposits were observed in any of the glomeruli in patients with MCD, and 100% of these patients were classified as negative. However, C4d deposits were detected in 100% of patients with MN, and were observable in all glomeruli with a uniform granular distribution, demarcating all capillary loops. Conclusions: C4d immunohistochemical staining is a very useful tool for diagnosing MN.
INTRODUCTION
Membranous nephropathy (MN) is the most common cause of nephrotic syndrome in adults.1 The diagnosis is based on typical findings observed using electron microscope (EM) and immunofluorescence (IF) studies. On some occasions, tissues are only available for analysis using an optical microscope (OM); in these cases, it can be difficult and at times impossible to differentiate between MN and minimal change disease (MCD). In these cases, it would be highly useful to have a diagnostic technique that could be performed on paraffin-fixed renal tissue.
The use of immunohistochemistry to detect the C4d complement degradation product in kidney disease has sparked considerable clinical interest recently. Studies have focused on transplant biopsies as an indicator of acute humoral rejection.2 Very little information is available on glomerular nephropathy. We have recently demonstrated that mesangial C4d deposition can be used as a bad prognostic factor in IgA nephropathy.3
C4d is a fragment of C4 generated during activation of the classical complement or lectin pathways. This fragment is highly stable, binds covalently to cell surfaces, and can be detected using reagents that are currently available.
MN pathogenesis is mediated by the in situ formation of immune deposits, with the resulting activation of the complement. Therefore, we can expect to find C4d deposits as a marker of complement activation in MN but not in MCD.
The aim of our study was to determine if C4d detection by immunohistochemical staining in MN patients could be a useful diagnostic tool.
MATERIAL AND METHOD
The study included all consecutive patients who underwent renal biopsies in our hospital between January 2001 and October 2008. The study was approved by the hospital’s Ethics and Research Committee. Patient information was processed in accordance with personal data protection regulations. Only adult patients with a diagnosis of MCN and idiopathic MN based on the histological analysis of the renal biopsy with OM, IF and EM studies were considered for inclusion in the study. For OM assessment, 2µm histological slices prepared from formaldehyde-fixed paraffin-embedded tissue were stained with hematoxylin and eosin, Schiff's periodic acid and methenamine silver. The IF study was performed with anti-IgG, IgM, IgA, C3, C1q, κ light chain, λ light chain antibodies, fibrinogen and albumin. The EM study was performed on glutaraldehyde-fixed renal tissue which was processed for ultrastructural analysis in line with standard laboratory protocols. The histological classification system proposed by Ehrenreich et al4 was used in MN. Five patients were in stage I, 15 in stage II and 1 patient in stage III.
Thirteen patients were excluded as glomeruli were not obtained for the C4d study. In the end, 19 patients with MCD and 21 patients with MN who met the criteria for inclusion were included in the study.
C4D IMMUNOHISTOCHEMICAL STAINING IN PARAFFIN-FIXED TISSUE
All renal biopsies were routinely processed for OM, IF and EM when they were taken, between January 2001 and October 2008. In October 2008, 3µm formaldehyde-fixed sections underwent immunohistochemical staining using anti-human C4d polyclonal antibodies from rabbits (Biomedica, Vienna, Austria).
All the patients’ histological sections were reviewed without clinical or pathology information. The details of these procedures were published previously.3 Patients were classified as positive when more than 75% of the glomeruli were C4d-positive and as negative when less than 25% of the glomeruli were C4d-positive.
C4d was also analysed by IF with monoclonal antibodies (Biogenesis, Vitro SA, Seville, Spain) in 2 MCD patients and 5 MN patients diagnosed after October 2008.
RESULTS
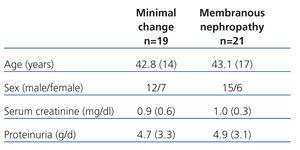
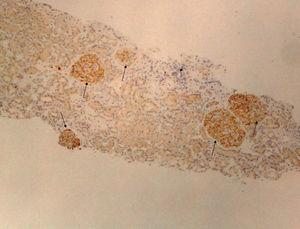
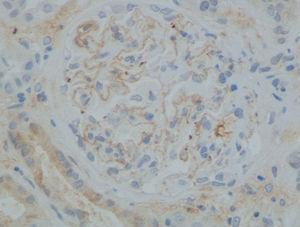
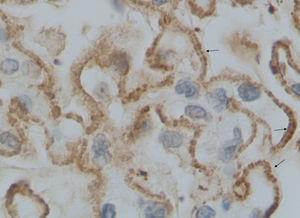
The Table shows the age, sex, serum creatinine and proteinuria of patients diagnosed with MCD and MN before October 2008 at the time of the biopsy. No C4d deposits were observed in any of the glomeruli in patients with MCD and 100% of these patients (n=19) were classified as negative. However, C4d was detected in 100% of patients (n=21) with MN (and in 100% of the glomeruli) (Figure 1) in the form of deposits with uniform granular distribution outlining all the capillary loops (Figure 2 and Figure 3). No mesangial deposits were found.
The C4d study by IF with monoclonal antibodies was conducted on another 5 patients diagnosed with MN after October 2008. All patients tested positive for C4d (Figure 4) in both the IF study and the immunohistochemical staining.
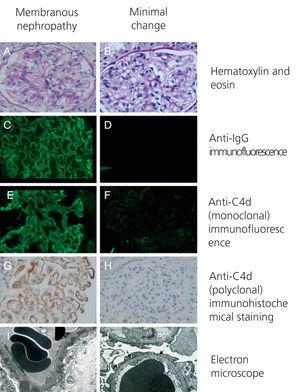
Figure 4 shows the hematoxylin and eosin staining study (A and B), the IF studies with anti-IgG (C and D), the IF study with anti-C4d (monoclonal) (E and F), the immunohistochemical staining with anti-C4d antibodies (polyclonal) (G and H) and the EM studies in two representative patients with MCD (B, D, F, H and J) and MN (A, C, E, G and I).
DISCUSSION
Complement deposition (detected by IF, immunohistochemical staining, or EM) is a common characteristic of certain forms of glomerulonephritis (membranoproliferative, post-streptococcal, IgA nephropathy, MN, lupus nephritis and some forms of rapidly progressive glomerulonephritis), and it is generally associated with antibody deposition.5-7 These complement deposits often contain both C4 and C3 and are characteristics of the classical pathway of complement activation. Sometimes, they only contain C3 or lack the first components, indicative of complement activation through the alternative pathway.
C4d is the breakdown product of C4, which is activated and degrades as part of the classical pathway of component activation, which is usually mediated by antibodies. This is more useful and applicable to this disease now as the antibody responsible for more than 50%-70% of these cases has been recently identified, an antibody targeted at M-type phospholipase A2 receptor.8 C4d can also be generated when the complement system is activated through the lectin pathway. Once generated, C4d binds covalently to tissue components at the activation site and is, therefore, a biomarker of classical or lectin pathway activation. C4d deposition in the capillaries of the renal graft was first described in 1993 by Feucht et al.2 More recently, the detection of C4d in the peritubular capillaries by immunohistochemical staining has been recognised as a sensitive index of antibody-mediated rejection.9,10
Very few studies have analysed C4d deposition in glomerular diseases. Glomerular C4d deposition is expected to be found in lupus nephritis and it is believed to be the result of the immune complex mediated activation of the classical complement pathway.11,12 In IgA nephropathy, Roos et al13 showed that renal histology is more severe when the lectin pathway is activated (and there are C4d deposits in the mesangium). Subsequently, our group demonstrated that mesangial deposition of C4d can be used as a prognostic factor in patients with IgA nephropathy.3 Renal survival after 10 years stood 43.9% in C4d-positive patients compared with 90.9% in C4d-negative patients (P=.005), which suggests that a different type of complement activation (classical pathway or lectin pathway) plays and important pathogenic role. In idiopathic MN, unlike MN secondary to lupus, there is no C1q deposition. In these cases, the presence of C4d is probably an indicator that the complement is being activated through the lectin pathway.
Information on the role played by C4d in MN is limited to one study published in 1989. In this study,14 IF was used to test for C4d in 12 patients with idiopathic MN and was detected in 11 of these patients.
C4d immunohistochemical staining using the immunoperoxidase technique described in our study has the major advantage of being performed on paraffin-embedded tissue so those cases in which there is no tissue available for IF or EM study can be diagnosed. Suzuki et al15 showed that C4d immunohistochemical staining was comparable to IF detection. Our data obtained from 5 patients coincides with this idea.
The site where the C4d is deposited is also worth mentioning. In IgA nephropathy, C4d staining was mainly observed in the mesangium, indicating the probable site where the local complement was activated.3,13 In this study on MN patients, C4d deposits were located in the capillary loops of the mesangium and with a granular distribution. MN is characterised by an accumulation of immune deposits on the outer surface of the glomerular basement membrane, which causes the membrane to thicken. These immune deposits have been identified as IgG, often IgG4,16,17 and the membrane attack complex of complement C5b-9.18 We believe that C4d forms part of these immune deposits. Furthermore, it has been suggested that complement activation plays no role in MCD pathogenesis. Our study provides support for both of these theories. C4d deposition was observed in the glomerular basement membrane of 100% of MN patients while the results were negative in 100% of the cases with MCD.
In summary, our data suggest that C4d immunohistochemical staining is a highly useful tool for the differential diagnosis of MN and MCD in adults. This finding is particularly significant as the diagnosis can be performed even if we only have tissue for OM available.
Conflicts of interest
The authors affirm that they have no conflicts of interest related to the content of this article.
Table 1. Clinical and analytical data at the time of renal biopsy
Figure 1. Immunohistochemical study with anti-C4d antibodies of a patient with membranous nephropathy (x10)
Figure 2. Immunohistochemical study with anti-C4d antibodies of a patient with membranous nephropathy (x40)
Figure 3. Immunohistochemical study with anti-C4d antibodies of a patient with membranous nephropathy (x100)
Figure 4. Hematoxylin and eosin studies, immunofluorescence with anti-IgG and anti-C4d antibodies (monoclonal), immunohistochemistry with anti-C4d (polyclonal) and electron microscope studies in two patients with minimum change disease and nephropathy