A 70-year-old woman with a prior history of primary biliary cirrhosis diagnosed 18 months earlier, being treated with ursodeoxycholic acid 600mg/day. No prior history of hypertension or diabetes mellitus. No known kidney diseases. Admitted to the nephrology department owing to acute renal function deterioration (creatinine: 4.12mg/dl; urea: 122mg/dl). Reported wasting syndrome, over a period of several months. Diuresis was maintained, and vital signs (blood pressure [BP]: 125/75mmHg) and physical examination were normal.
Findings included normocytic normochromic anaemia (Hb 10.3g/dl), which required initiation of erythropoietin treatment. Proteinuria of 0.840g/day with granular casts in the sediment, and ++++ microhaematuria. She tested positive for p-ANCAs at a titre of 29.1IU/ml. She also tested positive for anti-mitochondrial antibodies that were, at stable levels, given her already known biliary cirrhosis. Considering her acute kidney failure with positive autoimmunity for p-ANCAs, she underwent a kidney biopsy, which was consistent with diffuse extracapillary proliferative glomerulonephritis with cellular crescents in 75% of her glomeruli. She was diagnosed with rapidly progressive kidney failure secondary to type III or pauci-immune extracapillary proliferative glomerulonephritis, consistent with microscopic polyangiitis (MPA). Treatment with corticosteroids and oral cyclophosphamide (1.5mg/kg/day) was indicated. Good response to treatment with modest kidney improvement up to a creatinine level of 3.63mg/dl at discharge from the hospital.
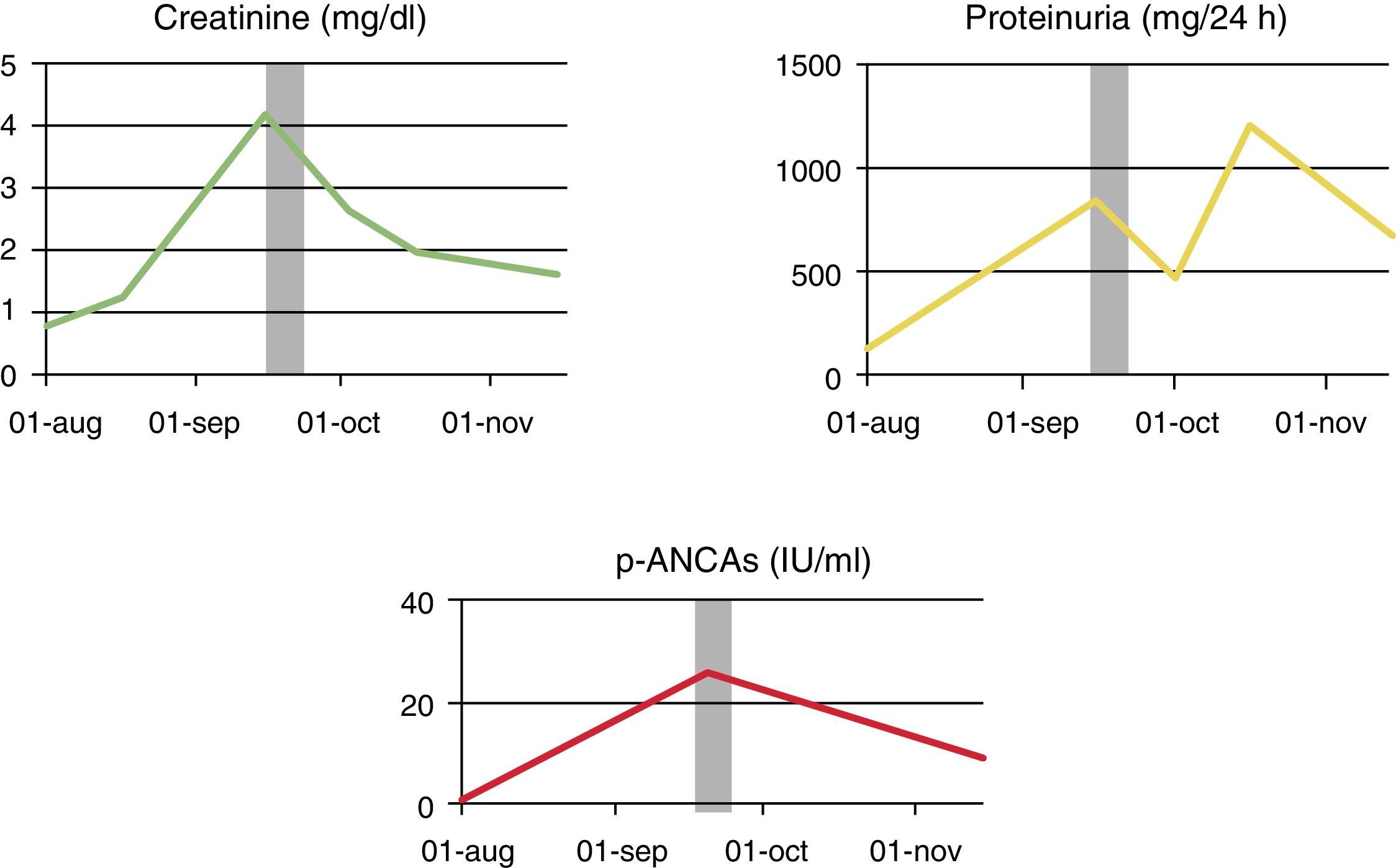
During subsequent follow-up in a nephrology visit, the patient was found to be asymptomatic and with a good control of BP. Her serum creatinine values decreased (1.56mg/dl), her p-ANCA titre were also reduced (8.5IU/ml), her proteinuria decreased (0.639g/day) and her microhaematuria disappeared (Fig. 1). In addition, her haemoglobin levels improved so erythropoietin treatment was discontinued.
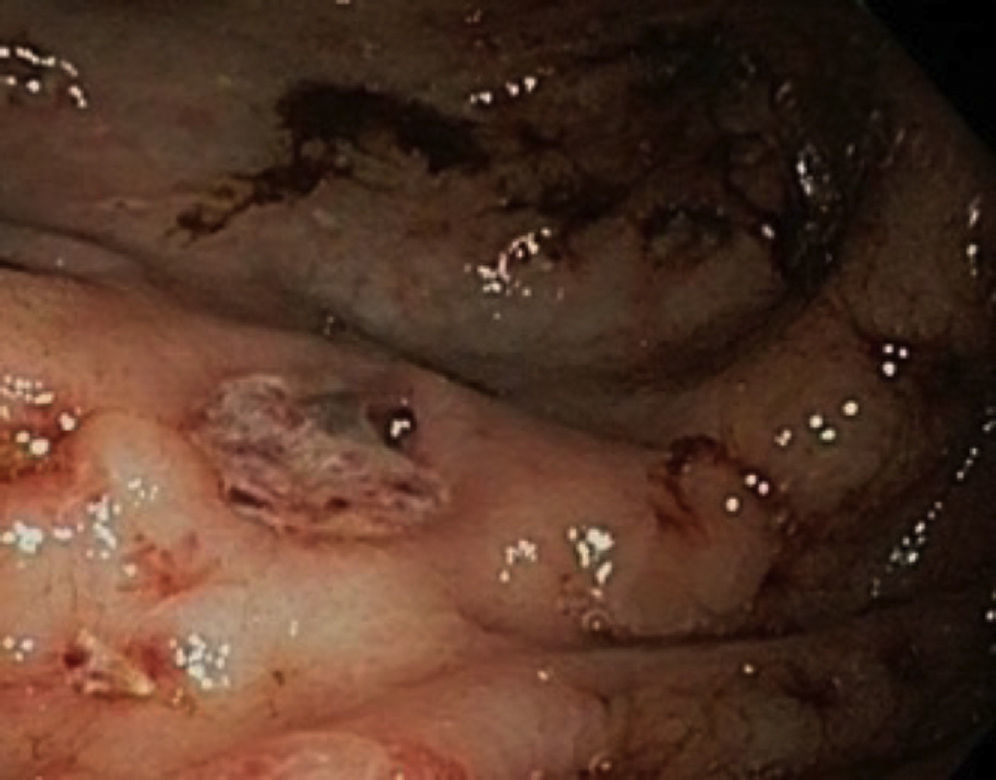
Two months after hospital discharge, she was admitted to the GI department due to gastrointestinal bleeding that affected her laboratory results with an acute exacerbation of renal failure due to hypotension and volume depletion. Gastroscopy and a colonoscopy were performed; denudation with capillary bleeding upon contact plus superficial and deep ulcers were observed, thus signs of vasculitis and inflammatory bowel disease were ruled out. As for infection, she tested positive for IgMs for cytomegalovirus, and herpes virus was isolated in oropharyngeal lesions. Despite the improvement in renal function up to baseline levels, the patient had a poor clinical course, as frequent fresh bloody stools persisted and she required transfusions every 24–48h that required admission to ICU. A repeat colonoscopy was performed, which showed multiple deep ulcers on punch biopsy with abundant bleeding (Fig. 2), and CMV of 27,784cop/ml was confirmed with PCR. Anti-viral treatment with ganciclovir and aciclovir was administered. A diagnosis was made of lower gastrointestinal bleeding secondary to enteritis due to cytomegalovirus in an immunosuppressed patient; in addition patient had herpes virus together with haemorrhagic colitis due to direct cyclophosphamide toxicity with secondary thrombocytopenia. Patient had uncontrollable gastrointestinal bleeding and despite a reasonable response of the kidney disease, she died a month and a half after hospital admission.
MPA is characterised by a constant and early presence of rapidly progressive glomerulonephritis. It is important to bear in mind treatment-related complications due to both direct toxicity and immunosuppression-related toxicities. In our patient's case, although her kidney disease responded well to treatment, there was a fatal complication, cytomegalovirus enteritis.1,2 This led to uncontrollable lower gastrointestinal bleeding and, finally, to her death.3,4
It is not uncommon to find a combination of several autoimmune diseases in a single patient, given their common background. In our case, MPA was diagnosed in a patient with a prior history of primary biliary cirrhosis, even though there are few references in the literature of cases in which these two diseases are combined.5–7
Please cite this article as: Ruiz-Ferreras E, Martín-Arribas A, Tabernero-Fernández G, Lerma-Márquez JL, Fraile-Gómez P, García-Cosmes P, et al. Poliangeítis microscópica en paciente con cirrosis biliar primaria. Complicaciones del tratamiento. Nefrología. 2016;36:78–80.