We present the case of a 64-year-old woman with multiple allergies, poorly-controlled hypertension, frequent headaches being followed by the neurology department, duodenal ulcer with a partial gastrectomy performed more than 20 years ago, and chronic kidney disease (CKD) secondary to IgA nephropathy. She began haemodialysis in May 2004. In November 2004, she received a cadaveric renal transplant; due to recurrence of underlying disease there was a progressive deterioration in renal function. In October 2010 she re-started a dialysis programme in the form of automated peritoneal dialysis (APD).
The patient presented to the emergency department after few hours of sudden-onset epigastric pain, radiating to the back, and with associated nausea. A peritoneal exchange was performed, in which significant haemoperitoneum was observed. It was therefore decided perform further test to investigate the cause of haemoperitoneum.
Blood tests showed a Hb of 9.4g/dL, leukocytes of 11400/μl, normal platelet count, urea of 133mg/dL, creatinine of 9.95mg/dL, and sodium and potassium within normal range. There were no coagulation abnormalities. In the peritoneal fluid analysis, the red cell count was 135000/mm3 and leukocytes were 369/mm3 (79.9% PMNs).
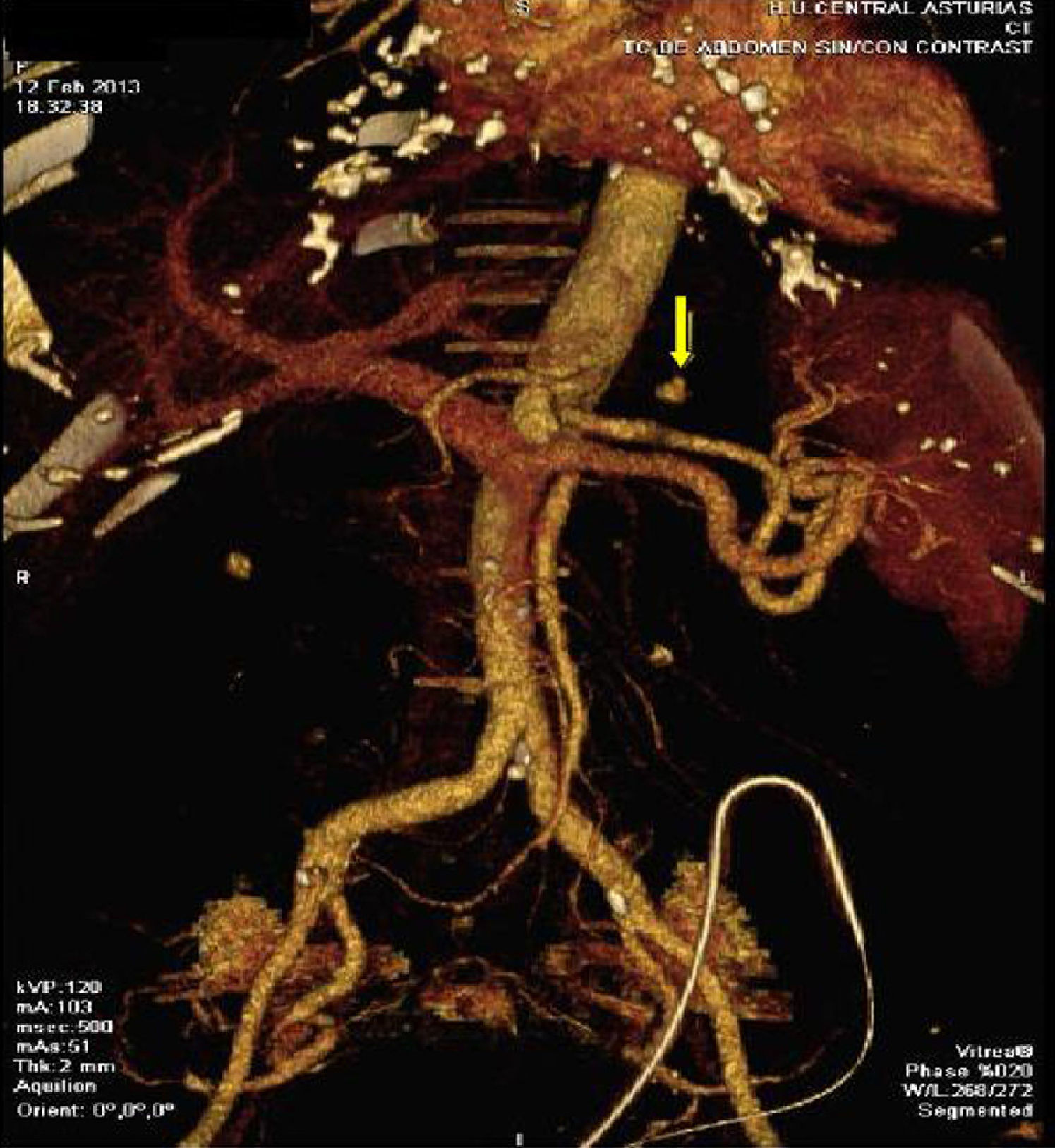
Following review of all the findings, it was decided to perform axial computed tomography (CT) with contrast. This revealed the presence of a hyperdense nodule in the posterior region of the gastric fundus compatible with pseudoaneurysm of the left gastric artery, with an underlying haematoma (Fig. 1). Percutaneous transcatheter embolization of the pseudoaneurysm was performed with the use of coils, with satisfactory control of bleeding as per angiography (Fig. 2).
The patient was subsequently admitted for haemodynamic monitoring; patient had an inguinal haematoma as a complication of the procedure and,required the transfusion of 2 units packed red cells.
She was kept on peritoneal rest, with frequent peritoneal lavage until peritoneal fluid became clear. During this time, haemodialysis was performed via a temporary jugular venous catheter.
She had a low-grade fever related to the haematoma, with negative blood cultures. After one week the patient re-started peritoneal exchanges with no signs of bleeding in the peritoneal fluid. She has had no further complications since this episode.
Haemoperitoneum is an uncommon complication of peritoneal dialysis, and can vary from minimal bleeding to frank haemorrhage causing shock.1–3 The most common cause of bleeding is related to menstruation or ovulation. Less common causes include sclerosing peritonitis, pseudoaneurysm of the splenic artery, polycystic kidneys, laceration of an abdominal organ, acute pancreatitis, and coagulation abnormalities.4
Our patient presented to the emergency department with epigastric pain of sudden onset. The bloody peritoneal fluid gave us a clue as to the cause of the pain, which led to a CT. With percutaneous embolization, the bleeding was stopped.
Peritoneal dialysis is an established renal replacement therapy technique, but among its advantages is the rarely-mentioned possibility of early detection of abdominal bleeding, revealing blood loss that would otherwise go unnoticed.5 In other cases, previously reported, immediate angiography and percutaneous transcatheter embolization helped to control bleeding and avoid laparotomy.1 In our case, due to the peritoneal dialysis technique, we were able to suspect the cause of epigastric pain and treat it appropriately.
Conflicts of interestThe authors declare no conflicts of interest.
Please cite this article as: Hidalgo-Ordoñez C, Sánchez-Alvarez E, Rodríguez-Suárez C. Una causa infrecuente de hemoperitoneo espontáneo en un paciente en diálisis peritoneal. Nefrologia. 2016;36:80–81.