Spain is the country with the greatest incidence of cocaine use in adults,1,2 and consignments of levamisole-contaminated cocaine has increased in the last decade.2,3 Regarding the use of cocaine/levamisole (C/L), a syndrome distinguished by the following has been reported: (1) purpuric, necrotic or ecchymotic skin lesions on the trunk, limbs and earlobes; the histological background is leukocytoclastic vasculitis or thrombotic vasculopathy; (2) leukopenia and neutropenia, and (3) positivity for different immune parameters2,3 (Table 1). Kidney disease due to C/L is found to be scarcely documented.
Clinical and serological characteristics of cocaine/levamisole use syndrome.
| Skin impairmenta: |
| Retiform purpura and skin necrosis (PS: leukocytoclastic vasculitis or thrombotic microangiopathy) |
| Typical location on earlobes and pinnae. Also on limbs, trunk and flanks |
| Musculoskeletal impairment: arthralgiaaand/or arthritisa; myalgia |
| Leukopenia, neutropenia and/or agranulocytosis |
| Serological abnormality: joint presence of multiple autoantibodies: |
| Double positivity for ANCAs; discordance between pattern of immunofluorescence and antibodies by ELISA; atypical ANCAs |
| ACLs, LA, ANAs, anti-DNA antibodies, hypocomplementaemia |
ACLs: anticardiolipin antibodies; LA: lupus anticoagulant; PS: pathology study.
We describe the case of a patient who developed necrotizing glomerulonephritis, with kidney failure and nephrotic syndrome, associated with C/L use. To our knowledge, this would be the first publication with kidney biopsy in Spain.
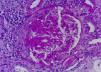
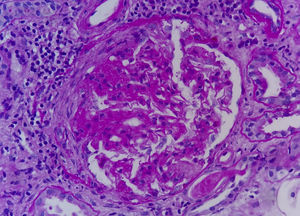
The patient was a 47-year-old male referred for kidney failure and nephrotic syndrome evaluation. Two years earlier, he had had self-limited skin lesions on his right flank and his earlobes, and analyses confirmed neutropenia and positivity for ANAs and ANCAs (MPO and PR3). In the current admission he reported nocturia for the last few months, choluria, intermittent oedema and arthralgia in the left shoulder, elbow and knee. He denied the use of tobacco, toxins or any medicine. Physical examination: afebrile, with a blood pressure of 120/70mmHg and all other parameters within normal limits. Laboratory test: haemoglobin 9.2g/dl, leukocytes 3190μl (neutrophils 54.6%), platelets 248,000μl, prolonged APTT (41.7min), Cr 2.66mg/dl, albumin 2.9g/dl, triglycerides 336mg/dl, cholesterol 207mg/dl, CK 167U/l; rheumatoid factor, C3–C4, serum electrophoresis and thyroid hormones negative/normal. Antinuclear antibodies positive at 1/160, anti-DNA antibodies negative, lupus anticoagulant positive, IgG anticardiolipin antibodies negative, IgM 18.8MPL/ml (positive>18MPL/ml), cryoglobulins negative, c-ANCAs negative, p-ANCAs positive, MPO 17IU/ml (positive>10), PR3 35IU/ml (positive>3). HLA-B27 negative. Serology for hepatitis B, hepatitis C and HIV viruses negative; previous exposure to cytomegalovirus, Epstein–Barr virus and parvovirus B19. Chest X-ray, echocardiogram and abdominal–pelvic CAT scan with no significant findings. Determination of toxins in urine was positive for cocaine. Sediment with 60–100 erythrocytes per field with 20%–30% dysmorphic, 6–12 leukocytes per field, culture negative, proteinuria 7680mg/24h with a non-selective glomerular pattern. The patient was questioned again and admitted to use of inhaled cocaine in the previous months. The kidney biopsy comprised 27 glomeruli: 3 with ischaemic changes, one with a fibrous crescent and the rest with segmental capillary tuft necrosis (Fig. 1); immunofluorescence was not significant. Methylprednisolone (1.5g IV), cyclophosphamide (750mg IV) and oral prednisone 60mg/day were administered in a decreasing regimen. After one month, serum creatinine level was 1.31mg/dl.
The percentage of cocaine samples contaminated with levamisole was 80% in the United States in 2011,2 and 48% in Spain between August and December 2009.4 It seems that cocaine is cut with levamisole because levamisole is a cheap powder with organoleptic characteristics similar to those of cocaine, and would increase cocaine's dopaminergic and sympathomimetic effects.1,5
Levamisole is an anthelmintic agent that was used as an immunomodulator in humans until 2000. It promotes immune manifestations through various mechanisms: (1) it facilitates the actions of macrophages, B lymphocytes and T lymphocytes, and neutrophil chemotaxis; (2) it would alter immune tolerance and (3) it has direct toxicity on neutrophils and endothelial cells.1,6 Cocaine in itself also may cause immune phenomena; therefore, it is possible for cocaine and levamisole to enhance each other. A jumbled or discordant immune pattern may be a key to diagnosis.1 ANCAs, ANAs, lupus anticoagulant and IgM anticardiolipin antibodies have been described; the presence of anti-DNA antibodies and hypocomplementaemia is rarer.1,3,6,7 Regarding ANCAs, positivity for both MPO and PR3 may be seen. Discordance between the pattern by immunofluorescence and ELISA may also be seen,1,6 and indeed was observed in this case.
Levamisole is difficult to detect in urine due to its short half-life2; however, demonstrated cocaine use plus characteristic clinical and laboratory abnormalities are sufficient to diagnose C/L syndrome.3
According to the series, both skin and/or joint manifestations (arthritis or arthralgia), which were present in our patient, are very common. Neutropenia is also common. A genetic susceptibility due to positivity for the HLA-B27 antigen has been shown in certain cases.1,3 Neutropenia tends to improve upon suspending drug use.2 Kidney manifestations due to C/L are asymptomatic urinary abnormalities, nephrotic syndrome and acute kidney failure.5,7,8 Although biopsied cases are few in number, pauci-immune extracapillary necrosing glomerulonephritis is the most common histological pattern,6–9 and may or may not be accompanied by pulmonary haemorrhage.8 Abstention from C/L is the mainstay of treatment and, in addition, various immunosuppressants have been used.8,9 The patient's clinical course is not always good, and he or she may require maintenance dialysis.8
It would be appropriate to alert medical professionals to the onset of C/L use syndrome, above all in the presence of neutropenia and multiple autoimmune phenomena. Given that cocaine use is illegal and patients tend to deny it, it is important to maintain a high degree of clinical suspicion to reach a diagnosis.
Please cite this article as: Sirvent AE, Enríquez R, Andrada E, Sánchez M, Millán I, González C. Glomerulonefritis necrosante en el síndrome por consumo de cocaína y levamisol. Nefrologia. 2016;36:76–78.