To the Editor:
The diagnosis and treatment of hyponatremia in the hospitalized patient is often challenging. Errors in volemic classification and diagnosis are frequent, and can induce inadequate therapy. More specifically, adrenal insufficiency (AI) is often overlooked as a cause of euvolemic hyponatremia, and is therefore underdiagnosed.
Glucocorticoid therapy (GC) is widely used in medical practice. Patients on chronic GC run the risk of developing AI if their doses are not increased when under stress, or if their doses are reduced or therapy discontinued when hospitalized for anotherr condition. We present the case of a woman previously on chronic inhaled glucocorticoid therapy, treated with dexamethasone following diagnosis of meningitis, who subsequently developed secondary AI as a consequence of withdrawal of steroid therapy.
CASE DESCRIPTION
A 78-year-old woman is admitted to the hospital with the diagnosis of pneumococcal meningitis, and an acute confusional state. The patient has a history of hypertension, asthma, ischemic heart disease, and post-surgical primary hypothyroidism, treated with valsartan (80 mg q.d., inhaled budesonide 0.5 mg t.i.d., diltiazen 60 mg t.i.d., clopidogrel 75 mg q.d., levothyroxine 100 mcg q.d. The physical examination reveals a temperature of 38 C, and temporo-spatial desorientation. Laboratory findings include an elevated WBC: 20,600 ul (>11,000 ul), INR: 1.3 (0.8-1.2), Serum creatinine (SCr): 0.86 mg/dl (0.6-1.35 mg/dl), serum urea: 31 mg/dl (10-50 mg/dl), Serum sodium (SNa): 138 mmol/l (135-145 mmol/l), Serum potassium (SK): 3.5 mmol/l (3.5-5.5 mmol/l). A cerebral Computerized Tomography (CT) was normal. Lumbar puncture was diagnostic of bacterial pneumococcal meningitis, and the patient was started on 5% dextrose iv (1500 ml daily), 0.9% iv isotonic saline solution (1000 ml daily) with 40 mEq of potassium chloride, iv meropenem (2g q.8.h.), iv dexamethasone (8 mg q.6.h.) and iv vancomycin ( 1 g q.8.h.).
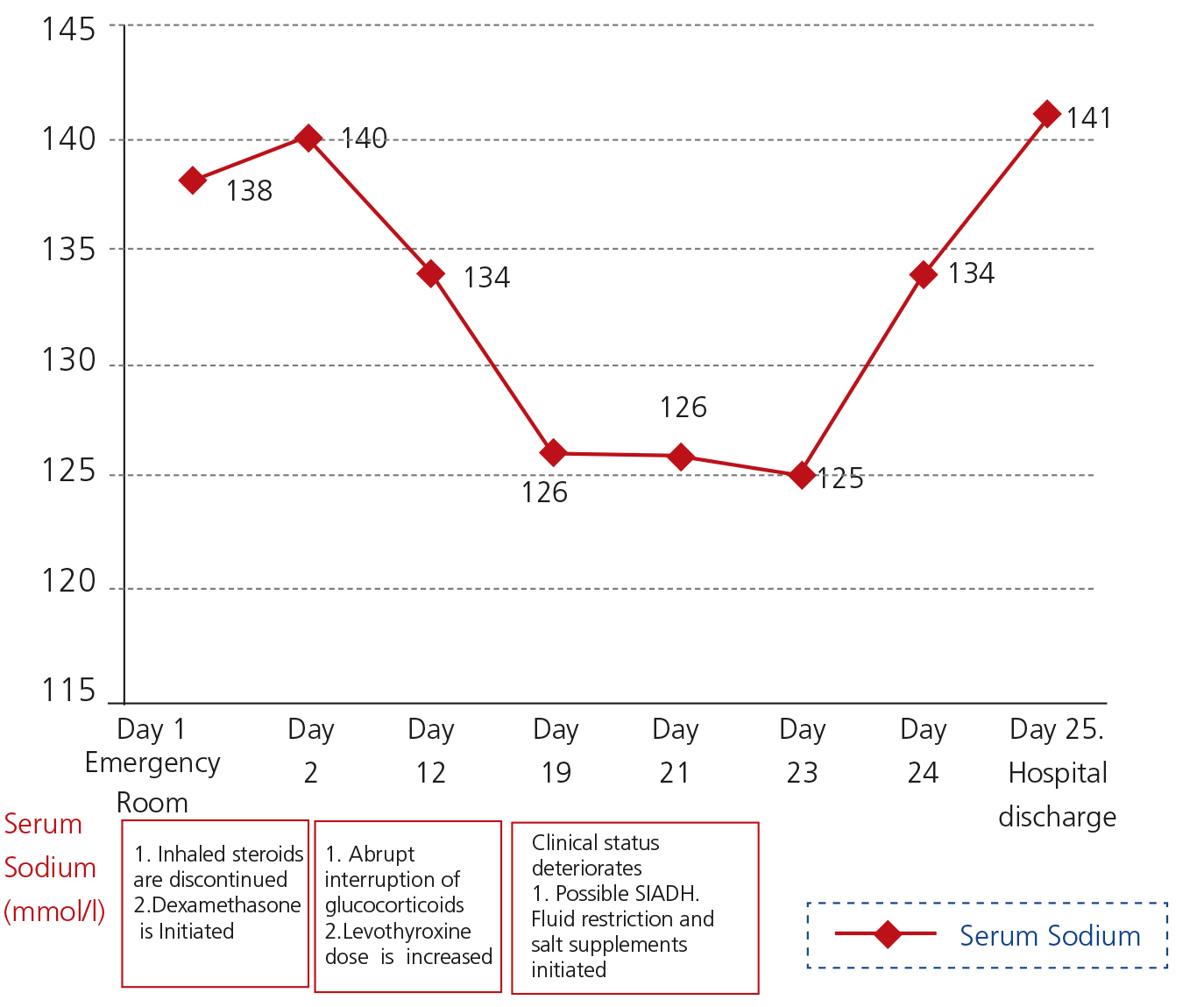
Dexamethasone therapy was abruptly discontinued on the 10th day following admittance, when the patient was on a iv dose of 4 mg q.6-h. Iv dextrose and saline solution were also interrupted at that time. On the 19th day of hospitalization, the patient was drowsy, and presented low blood pressures. A CT scan revealed no alterations. Laboratory tests revealed a SNa: 126 mmol/l, SCr: 0.71 mg/dl, Surea: 40 mg/dl, venous blood gas with a pH: 7.39 y K: 4.1 mmol/l. The diagnosis of SIADH was made, fluid intake was restricted to a liter daily, and salt supplements were added (2 g t.i.d.). The patient did not improve, maintaining a SNa: 126 mmol/L, Urine Na. 79 mmol/L, Plasma osmolality: 253 mOSm/kg, (275-290). Urine osmolality: 285 mOsm/kg (> 100). The patient was euvolemic, with bradypsychia, and disoriented. Her blood pressure was low, and was her fasting serum glycemia (60 mg/dl). An eight o´clock serum cortisolemia was ordered as part of the routine workup of euvolemic hyponatremia: 2,5 mcg/dl (5-25 mcg/dl). Plasma Corticotropin (ACTH): 21.6 pg/ml (10-46 pg/ml), indicating the presence of central AI (ACTH deficit)1, secondary to abrupt interruption of dexamethasone therapy. Oral Hydrocortisone was initiated (20 mg t.i.d.), with an initial SNa of 125mmol/l. Following 24 hours of therapy, SNa had risen to 134 mmol/l. Forty eight hours after starting the patient on hydrocortisone, she was discharged, eunatremic. (Fig. 1, Table 1).
Hyponatremia induced by the antidiuretic hormone (ADH) is frequent in hospitalized patients. Causes include nausea, pain, SIADH, and hypocortisolism. Before establishing the diagnosis of SIADH, other causes of ADH-mediated euvolemic hyponatremia must be ruled out, assuring adequate thyroid and adrenal function2.
Chronic high-dose glucocorticoid therapy inhibits the hypothalamic-pituitary-adrenal axis (HPA), and patients are at a risk of developing adrenal failure when steroids are inadequately discontinued. In fact, interruption of glucocorticoid medication is currently one of the most common causes of adrenal insufficiency. High GC doses given chronically inhibit hypothalamic synthesis of Corticotropin Releasing Factor (CRH), thereby interruptig CRH trophic and secretagogue stimilation of anterior pituitary corticotrophs3, that stop secreting ACTH. Without ACTH stimulation, the adrenal cortex undergoes atrophy, and cortisol is not secreted. However, the renin-angiotensin axis maintains stimulus of adrenal aldosterone secretion, and hyerkalemia/acidosis do not ensue.
When evaluating a patient with AI, all routes of steroid administration must be taken into account, including oral, iv, ophthalmic, inhaled, transdermic, intramusuclar, or intraarticular therapy. 4,5.
In the presence of hypocortisolemia, once steroids are discontinued, CRH and ADH synthesis and secretion are stimulated in the dorsomedial parvocelular portion of the paraventricular hypothalamic nucleus, and act on the anterior pituitary corticotrophs to recuperate ACTH secretion. Recuperation of the HPA can be slow, taking days or even months. The high levels of parvocelular ADH will stimulate the opening of Aquaporin-2 channels into the renal collecting duct, inducing antidiuresis. Parvocelular AVP is not inhibited by a descent in blood osmolality, and can thus cause euvolemic hyponatremia.
The differential diagnosis of a patient with meningitis and hyponatremia includes Cerebral Salt-Wasting, SIADH, hypothyroidism, and central (secondary) adrenal insufficiency. Serum hemodilution and clinical euvolemia will rule out Salt-Wasting. Hyponatremia secondary to hypothyroidism is extremely rare, and hypothyroidism must be severe to induce it6. The diagnosis of SIADH must always be made after having ruled out other disorders, although this golden rule is often overlooked.
Our patient was on chronic budosine therapy, discontinued upon admittance. This medication can inhibit the HPA when used at high doses chronically. Interruption of inhaled GC has been described to be a cause of acute central AI7. Interruption of both budesonide and iv dexamethasone would have contributed to her development of central AI.
Clinical symptoms of central AI can be non-specific: fatigue, nausea, abdominal pain, hypotension, hypoglycemia, can be seen8. AI often goes undetected when not specifically thought of.
The clinical and analytical response of a patient with central AI started on GC therapy is dramatic. Negative GC feedback on parvocelular AVP secretion rapidly inhibits its secretion, and marked aquaresis ensues, with a risk for overcorrection of SNa during the first 24 to 48 hours of GC treatment9. Given the risk for overcorrection inducing Osmotic Demyelination Syndrome, patients' rise in SNa must be closely monitored during initial treament.
We present this case to highlight the importance of considering central AI in patients whose chronic CG therapy has been discontinued, and to underline the fact that other causes of euvolemic hyponatremia must be ruled out before establishing a diagnosis of SIADH.
Conflicts of interest
The authors declare that they have no conflicts of interest regarding the contents of this article
Figure 1. Evolution of Serum Sodium during hospitalization in a patient with hyponatremia induced by hypocortisolism