To the Editor,
Residual renal function (RRF) has prognostic value in patients treated with peritoneal dialysis (PD) due to its beneficial effect on patient survival and technique1,2. One of the objectives of treatment is control and prevention of factors that can cause a decrease in RRF3. Peritonitis episodes may contribute to deterioration of RRF both due to the inflammatory reaction and possible nephrotoxicity of antibiotics used. However, it is a subject not frequently addressed and the limited results available are controversial4,5.
In the present study we analyse the impact on RRF of episodes of peritonitis occurring during the first 12 months on PD.
MATERIAL AND METHOD
From 2007 to 2011, 70 patients began PD consecutively in our unit. According to our clinical protocol, RRF is measured routinely in all patients treated with dialysis by determining the glomerular filtration rate estimated as the arithmetic mean of urinary urea and creatinine clearances. The first determination is usually done in the first week of renal replacement therapy and is considered the baseline glomerular filtration rate. It is then repeated every two months until diuresis is less than 100ml/day. From that moment the patient is considered anuric and RRF is zero. The rate of decline in glomerular filtration rate (ml/min/month) was established as follows: the difference between the value of baseline glomerular filtration rate and last value of glomerular filtration rate obtained before considering this had disappeared (less than 100ml/day urine output), or the value of glomerular filtration prior to the end of PD treatment (due to transplant, death, recovery of renal function or referral to haemodialysis [HD]), or the value of glomerular filtration rate at the time this study ended (30 June 2012). This difference was divided by the number of months of the period analysed.
Nineteen patients had at least one episode of peritonitis during the first twelve months (11 patients: 1 episode; 5 patients: 2 episodes; 3 patients: 3 episodes), and these constitute the study group. The remaining 51 patients did not experience any episodes of peritonitis in the first year and constitute the control group. All received as empirical treatment, until culture results were available, and according to the unit protocol: vancomycin (2g every 4 days) and intraperitoneal tobramycin (150mg loading dose + 16mg x exchange).
Results are expressed as mean ± standard deviation for normally distributed data. The decrease in glomerular filtration has a normal distribution and the results are expressed as median and 25th and 75th percentiles (interquartile range). Quantitative variables were compared with Student's or Mann-Whitney tests. Qualitative variables were compared with Fisher's test.
RESULTS
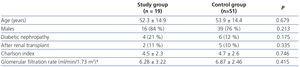
At baseline there were no differences between both groups in relation to age (52 vs. 54 years), sex, comorbidity (Charlson 4.5 vs. 4.7), origin of non-functioning transplant or glomerular filtration rate (6.28 vs. 6.87ml/min). The prevalence of diabetic nephropathy was higher in the group of patients with peritonitis (21%) compared to the group without peritonitis (12%), but the difference was not statistically significant (Table 1).
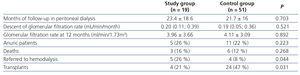
Follow-up time on PD was similar in both groups, with no differences in mortality. Episodes of peritonitis had no effect on the rate of decline of glomerular filtration rate, glomerular filtration rate after one year of treatment, or the rate of anuric patients. However, the exit from the PD programme due to renal transplant was lower in the study group. Five patients were referred to HD after suffering 1 episode of peritonitis (2 patients), 2 episodes (2 patients) and 3 episodes (1 patient). The referral to HD was 18% in patients who had 1 episode of peritonitis (2 of 11) and 38% (3 of 8) in those which had more than 1 episode. The reasons for referral to HD were catheter removal in two cases and loss of independence in three patients. None of the patients referred to HD subsequently returned to PD. Obviously, the referral to HD was higher in the group that suffered at least one episode of peritonitis with regards to the control group (Table 2).
On average, patients with peritonitis received two doses of vancomycin of 2g each and 5 days of tobramycin.
DISCUSSION
Maintenance of RRF on dialysis has an important prognostic value. Diabetes mellitus, obesity, high initial transport, high protein intake and coronary disease are risk factors associated with rapid loss of residual function5,6. In our series, the number of diabetic patients in the group with episodes of peritonitis was double than among those without peritonitis. However, only 1 diabetic patient with peritonitis was referred to HD (5.2%), compared to 4 (7.8%) with non-diabetic peritonitis. Therefore, the presence of diabetes was not significant, although the small sample size precludes definitive conclusions. Aminoglycoside nephrotoxicity is well known. Nonetheless, aminoglycosides are still used as empirical treatment in peritonitis due to their bactericidal properties, activity against gram-negative bacteria, low price, low allergenic profile and low resistance. According to our experience, and that of other authors6, empirical treatment of peritonitis episodes with aminoglycosides did not affect renal function. On the one hand, peritonitis meant less time on PD, since 26% of patients had to migrate to HD. On the other hand, they had less chances of receiving a transplant, since patients are excluded from the transplant list during peritonitis and kept off it for a minimum of one month after peritonitis is considered cured.
CONCLUSIONS
In our study we did not observe that peritonitis during the first year of PD treatment has a deleterious effect on RRF, despite using potentially nephrotoxic antibiotics, but it decreases the likelihood of kidney transplant and continuation on PD.
Conflicts of interest
The authors declare that they have no conflicts of interest related to the contents of this article.
Table 1. Clinical and laboratory data at the start of treatment with peritoneal dialysis
Table 2. Progression data