Antecedentes: Las complicaciones asociadas con el catéter en diálisis peritoneal causan disminución en su eficacia e interrupción de ésta, conversión a hemodiálisis, hospitalizaciones y necesidad de cirugía para cambiar el catéter. Objetivos: Determinar factores de riesgo para la disfunción temprana del catéter que hace necesario su cambio. Métodos: Se incluyeron 235 catéteres colocados con técnica quirúrgica abierta en línea media infraumbilical. Dentro de los posibles factores de riesgo se incluyó: edad, género, índice de masa corporal, área de superficie corporal, diabetes, enfermedad poliquística renal, cirugía previa, tiempo quirúrgico, omentectomía, omentopexia, infección de la herida y hernia posincisional. Resultados: El cambio del catéter por disfuncionalidad ocurrió en 47 pacientes (20%) durante el primer año. La complicación más frecuente fue: migración del catéter y peritonitis (4,3% en ambos casos), además de obstrucción por el omento (3,7%). En el análisis univariado, los pacientes que presentaron disfunción del catéter/cambio eran jóvenes con índice de masa corporal y área de superficie corporal bajos (p < 0,05). La infección de la herida y la hernia posincisional estaban asociados significativamente con el cambio de catéter. La omentectomía fue asociada a baja incidencia de disfunción de catéter/cambio en el análisis univariado y regresión logística (razón de momios: 0,275, intervalo de confianza: 95%, 0,101-0,751, p < 0,012). Conclusiones: Nuestra técnica de inserción de catéter ofrece bajas tasas de complicaciones y buenos resultados el primer año posquirúrgico. Además de la omentectomía, en nuestro estudio no se encontró un factor de riesgo para cambio de catéter en nuestra población. La omentectomía tuvo un efecto protector en términos de cambio de catéter.
Introduction: Catheter-related complications in patients on peritoneal dialysis lead to decreased effectiveness and discontinuation of the technique, conversion to haemodialysis, hospitalisation, and surgical interventions to replace the catheter. Objectives: Determine risk factors for early catheter dysfunction that result in the need for replacement. Methods: We analysed 235 catheters placed by open surgery using an infra-umbilical midline incision. Possible risk factors included the following: age, sex, body mass index, body surface area, diabetes, polycystic kidney disease, previous surgery, time of surgical procedure, omentectomy, omentopexy, wound infection and postoperative incisional hernia. Results: During the first year, 47 patients (20%) required a catheter replacement due to poor function. The most common complications were catheter migration and peritonitis (4.3% in both cases), followed by obstruction from omental wrapping (3.7%). Univariate analysis showed that patients with catheter dysfunction or requiring catheter replacement were younger, with a lower body mass index and body surface area (P<.05). There was a significant association of wound infection and post-operative incisional hernia with catheter replacement. Omentectomy was associated with a low incidence rate of catheter dysfunction/replacement in the univariate and logistical regression analyses (odds ratio: 0.275; 95% confidence interval: 0.101-0.751; P<.012). Conclusions: Our catheter placement technique offers a low complication rate and good results in the first year after surgery. Except for omentectomy, we did not discover any risk factors for catheter replacement in our study population. Omentectomy had a protective effect in terms of catheter replacement.
INTRODUCTION
Continuous ambulatory peritoneal dialysis (PD) has become an established option for treating patients with end-stage renal disease. This therapy requires the insertion of a permanent PD catheter. An estimated 25% of the world population on PD lives in Latin America. In particular, Mexico is the country with the highest use of this technique in the world.1
PD catheters are inserted using various techniques. Open surgical approaches can involve midline,2-4 paramedian infra-umbilical laparotomy5,6 or multiple laparoscopic approaches.7-10 Although laparoscopy has become the surgical method of choice for placing PD catheters, open surgery techniques remain as an important option when laparoscopic resources are limited, whether due to the lack of laparoscopic equipment in different hospitals due to costs, or due to operator limitations.
Complications associated with PD contribute significantly to morbidity and mortality rates, interruption of treatment, and decreased efficacy of dialysis, in addition to causing the need for conversion to haemodialysis, hospitalisation, and subsequent surgeries. Early and late complications such as surgical wound infection, peritonitis, and catheter dysfunction due to migration, obstruction, bleeding, granuloma, or post-incisional hernia limit the long-term survival of the PD catheter in 35%-51% of cases after 24 months.11 An 80% catheter survival rate after one year has been recommended as a target for PD centres,5,8,12 and can be reached using the most economical resources available and techniques appropriate for each PD unit. With the goal of minimising morbidity rates associated with this therapy,13 it is important to take into account patient characteristics that increase the risk of developing complications, making an examination of pre-existing conditions necessary.
Several studies associated complications with different factors including age, gender, diabetes, sepsis, prolonged duration of surgery, and previous abdominal surgery5,14-17. Several authors observed that an omentectomy and/or omental wrapping prevents catheter dysfunction, while other studies showed no correlation between previous omentectomy or abdominal surgery and postoperative complications.3,7,18-20
The aim of this article was to present the results from our experience in the insertion of PD catheters and to determine which factors involve a higher risk for early catheter dysfunction and affect 1-year survival rates.
METHODS
Patients
We performed a retrospective review of clinical histories from patients with end-stage renal disease that underwent open surgery for catheter placement in preparation for the start of PD.
All procedures were performed by a single surgeon between January 2004 and January 2010. Demographical data, patient characteristics, surgical records, and catheter complications during the first year requiring catheter replacement were collected and analysed. We received approval from the Institutional Review Board and the Bioethics Committee for data collection and analysis, respectively.
Surgical procedure
Each patient was administered cefotaxime (1g intravenously in a single dose) for preoperative prophylaxis. All catheters used were standard Dacron double-cuff straight Tenckhoff catheters. Anaesthetic technique was determined on a case-by-case basis by the attending anaesthesiologist. Each catheter was inserted by mini-laparotomy through a vertical midline infra-umbilical incision of approximately 3cm-4cm. The peritoneum was exposed using an open surgical technique, and the catheter was placed directly in the pelvic cavity. After placement, the internal cuff was joined to the peritoneum with a 2/0 chromic suture and permeability was verified. The linea alba was closed using size 1 polyglycolic acid suture. The catheter was removed from the peritoneal cavity through the wound, and the end of the catheter was tunnelled subcutaneously, passing through the skin in a small para-umbilical incision with the external Dacron cuff in the subcutaneous tissue. The subcutaneous tissue and skin were closed using standard procedure. Dialysate solution was immediately infused into the peritoneal cavity while in the operating room in order to ensure there was no leakage of dialysate fluid. The decision to perform an omentectomy was left to the surgeon’s judgement, depending on whether the omentum was accessible through the incision, the size of the omentum, and whether it could reach the catheter and obstruct it. Recently (since 2010), omentopexy has been performed using the same criteria as omentectomy. Omentopexy involves anchoring the omentum to the abdominal wall above the infra-umbilical incision with interrupted absorbable sutures (2/0 chromic) from the omentum to the peritoneum wall and bilaterally around the navel. The majority of patients started on PD within 24 hours of catheter placement, using continuous ambulatory PD with a predetermined infusion volume of 2000cc in all cases. Catheter replacement was requested by the nephrology department, once salvage treatment was determined to have failed.
Statistical analysis
We performed a simple descriptive analysis of the data. Categorical variables were described using proportions, and continuous variables with a normal distribution were described using mean (standard deviation). We used Student’s t-tests and Mann-Whitney U-tests to evaluate differences for catheter dysfunction between continuous variables with normal and non-normal distribution, respectively. Categorical variables were analysed using chi-square tests or Fisher’s exact tests to identify variables associated with catheter dysfunction. We determined odds ratios (OR) and created a logistic regression model in order to determine the risk factors in the univariate analysis. We considered a P-value <0.05 to be statistically significant, and used SPSS™ software, version 17.0, for all statistical analyses (SPSS, Chicago, IL, USA).
RESULTS
Patient and surgical registry characteristics
During the study period, a total of 235 patients were placed catheters (118 women and 117 men). Mean patient age was 51.4±17.5 years (range: 13-86 years), mean body mass index (BMI) was 26.3±4.2kg/m2 (range: 14.4-40), and mean body surface area21 (BSA; Mosteller) was 1.7±0.1m2 (range: 1.06-2.1). Some 43% of patients (n=101) had diabetic nephropathy, and only 3% (n=7) had autosomal dominant polycystic kidney disease.
Forty-six of the 235 patients (19.6%) had a history of previous abdominal surgery. Of these, only 26 had previously undergone one surgical procedure before, 12 patients had undergone two previous surgical procedures, 4 had undergone three previous surgical procedures, and 4 patients had undergone more than 3 previous surgical procedures. Regional anaesthesia was used in 95.8% of cases (n=225) during catheter placement; and general and local anaesthesia protocols were used evenly (2.1%, n=5 each). Mean duration of surgery was 43.7±14 minutes (range: 15-120). An omentectomy was performed in 37.9% of catheter placements (n=89), and an omentopexy was performed in 10 patients (4.3%). Dialysis was started within 24 hours of catheter placement in 97% of patients (n=230).
Peritoneal dialysis catheter complications and results
Catheter dysfunction that eventually required catheter replacement occurred in 47 patients (20%), and 80% of catheters were incident-free after one year.
Catheter dysfunction appeared after a mean 6.8±22.6 days (range: 0-120). The most common causes of catheter dysfunction were migration (4.3%, n=10) and peritonitis (4.3%, n=10), followed by obstruction of the catheter by omental wrapping in 9 patients (3.7%). Eight patients (3.4%) suffered surgical wound infection, and all of them required catheter replacement at some point. Other causes for changing the catheter included bleeding (haemoperitoneum) (2.1%, n=5) and fibrin clots in the catheter (2.1%, n=5). The 8 patients with surgical wound infections (3.4%) also had dialysate fluid leaks. Four patients (1.7%) had only one dialysate fluid leak and did not require PD catheter replacement. Another complication that did not require catheter replacement was granuloma in the exit site with subcutaneous tunnel infection in 1.7% of patients (n=4). Ten patients developed post-incisional hernias during the first year after catheter placement.
Factors associated with catheter dysfunction
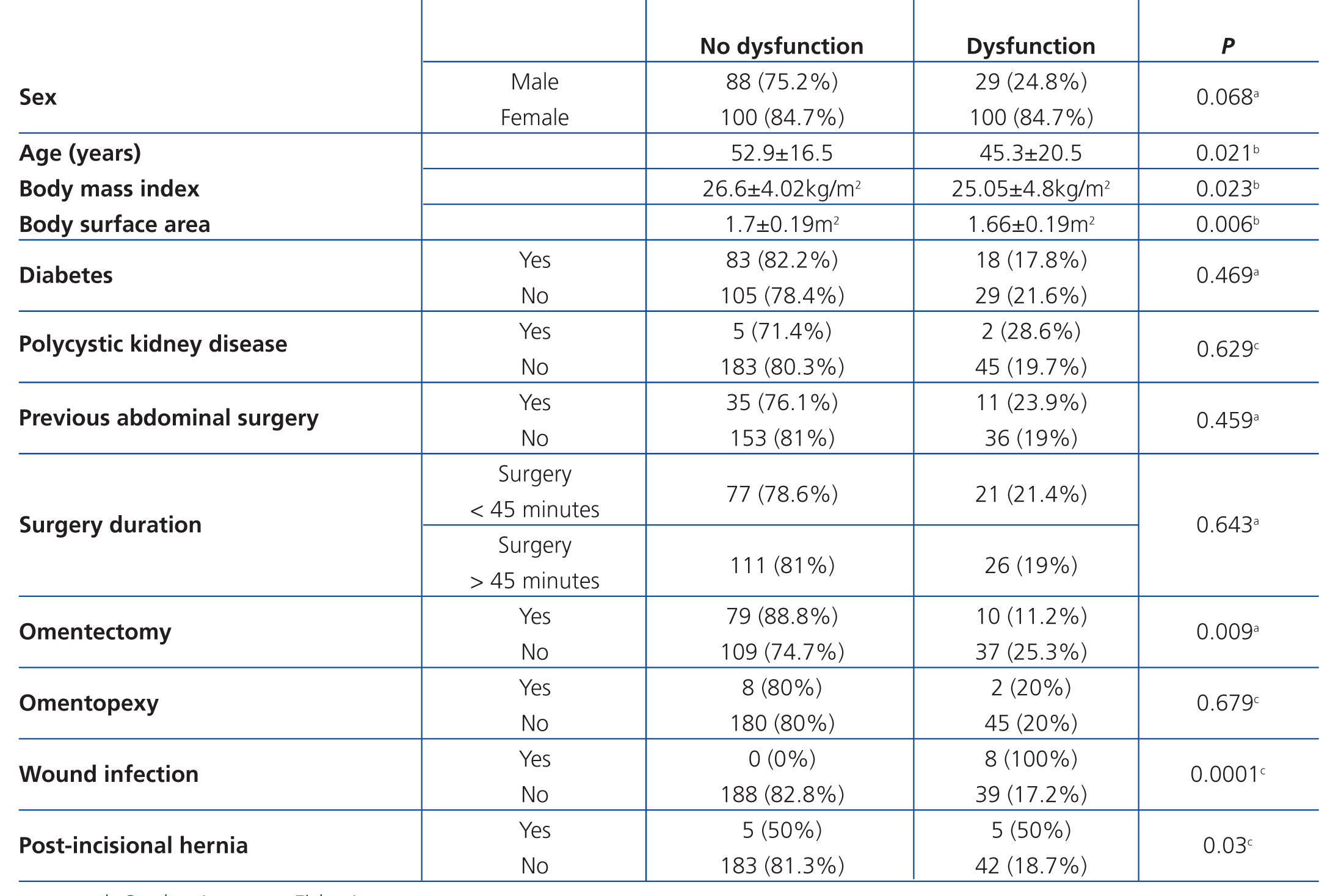
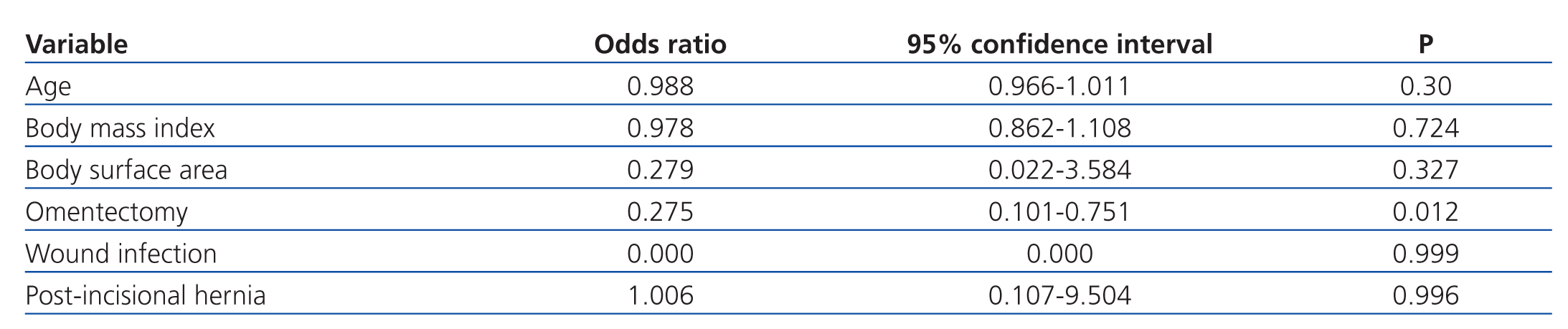
We compared patients with and without catheter dysfunction, searching for factors associated with this phenomenon (Table 1). Patients with dysfunction were younger, with lower BMI and BSA than those without dysfunction (P<.05). There were no differences between groups with and without diabetes and autosomal dominant polycystic kidney disease. We did not find any correlation between previous abdominal surgery and catheter dysfunction, or the duration of the surgical procedure when using a 45-minute cut-off point. Patients that underwent an omentectomy had a lower incidence of catheter dysfunction (11.2%) than patients that did not undergo an omentectomy (25.3%) (P<.009). We did not observe a similar association for omentopexy. Patients that developed a post-incisional hernia developed catheter dysfunction in half of all cases (P<.03), and all patients with surgical wound infection required catheter replacement (P<.0001). The logistic regression analysis showed that having undergone an omentectomy was a statistically significant protective factor against catheter dysfunction (P<.05). No other variables that were significant in the univariate analysis for catheter dysfunction had a significant positive or negative impact on risk factors in the multivariate analysis (Table 2).
DISCUSSION
Our study showed a considerable level of effectiveness and safety in PD catheter placement using an open surgical approach with an infra-umbilical midline incision. In addition, certain patient variables, such as age, BMI, BSA, and surgical aspects, such as wound infection and post-incisional hernia, were associated with early catheter dysfunction and catheter replacement, contrasting with the protective effect of an omentectomy, which reduced the probability of catheter dysfunction.
We observed a wide range of complications that affected the incidence of catheter replacement. The incidence of catheter migration (4.3%) was lower than that of 7.6% reported by Liu et al,4 and those high rates (22%-24%) reported in other studies.5,8 In a similar manner, omentum or fibrin obstruction occurred at a combined incidence of 5.8%, lower or similar to rates reported in other studies.4,5
As regards infectious complications, our rate of surgical wound infection was lower than in other studies, and few patients in our study had peritonitis, as compared to an unusual rate of 30% reported in other studies.3,5 However, we must be cautious in interpreting our results, taking into account that the majority of our complications resulted in catheter replacement, except for 4 patients with dialysate fluid leaks and those patients with complications at the catheter exit site. This may reveal suboptimal salvage manoeuvres, such as anti-infection treatment and catheter recovery using fluoroscopic guidance.
One of the intrinsic properties of the omentum is that, when it comes into contact with a foreign body, it attempts to surround and isolate it. Omental wrapping was a very common cause of catheter dysfunction in our study (3.7%). Some authors have suggested performing an omentectomy during catheter placement to avoid wrapping and the need for secondary interventions,19 since 27% of patients that do not undergo an omentectomy develop catheter obstruction. We also observed a significant difference in catheter dysfunction and replacement when an omentectomy was performed. In our study, omentectomy had a protective effect against catheter dysfunction and replacement in both univariate and multivariate analyses, probably due to the reduced rate of obstruction from omental wrapping.
The majority of studies assessing PD catheter placement place special emphasis on a previous history of abdominal surgery as a potential risk for PD complications. Tiong et al5 analysed several factors related to catheter dysfunction and found that patients with a background of diabetes, glomerulonephritis, or previous abdominal surgery had a higher probability (OR: 3.24; 6.52; 3.42, respectively) of early complications (within 30 days after catheter placement) in a population with a prevalence rate of 43.8% for previous surgery. A longer duration of the surgical procedure was also associated with early complications. Another study examining hernias as a potential complication of PD catheter placement17 found that patients with polycystic kidney disease had a 2.5 times higher risk of complications, and that female sex was a protective factor against the occurrence of hernias. Although we observed several factors, including age, BMI, BSA, wound infection, and post-incisional hernia that were associated with catheter dysfunction in the univariate analysis, none were associated with a higher risk of catheter dysfunction and replacement in the logistic regression analysis. Crabtree et al22 observed that abdominal scarring and previous history of peritonitis did not predict the severity of adherences and should not be used for deciding whether or not to use PD. We did not observe any relationship with other aspects of surgery, such as previous abdominal surgery or pre-existing medical conditions (for example, diabetes mellitus, polycystic kidney disease) that might affect selection criteria for entering our PD programme in the future. Currently, we do not assess patients based on previous abdominal surgery in order to use PD as a renal replacement therapy, despite the low prevalence of previous abdominal surgery (19.6%) as compared to other studies.5,22 We should point out that in several of the previously mentioned studies the PD catheters were placed by several different surgical teams, whereas in our study only one surgical team performed all procedures, which partially standardises the results, ensuring that the same criteria were used for performing an omentectomy or omentopexy and that the procedure was systematic.
Our study had several limitations, primarily those related to the retrospective design of the study, such as a biased sample selection, no control group, and difficulties in measuring and recording data for the different variables assessed. Another issue in our results lies in the open approach used for catheter placement: laparoscopic techniques are used more and more frequently7,9,10,19,20,22; however, several centres, mainly from Asia, still use open techniques with good results.2-6,17 In particular, we used an open approach for several reasons: firstly, we have limited use of laparoscopic techniques due to equipment and financial limitations, and secondly, both the open technique using a midline incision and the subjective criteria used for deciding to perform an omentectomy are easy to learn and reproduce by the residents at our hospital. In addition, our results are similar or better than the results from Asian studies involving open techniques in terms of mechanical complications4,5,8 and even better than results from laparoscopic techniques,7,9,10 so we have continued to use an open surgical approach.
In conclusion, PD catheter placement using an open surgical approach with an infra-umbilical midline incision offers good results with few surgical complications after one year. In our study, we did not find significant risk factors for early catheter replacement. Omentectomy had a protective effect against catheter dysfunction and replacement. A prospective, randomised study evaluating omentectomy and PD catheter placement would confirm our conclusions.
Conflicts of interest
The authors affirm that they have no conflicts of interest related to the content of this article.
Table 1. Comparison of patients with peritoneal dialysis catheter dysfunction and those without
Table 2. Predictive factors for peritoneal dialysis catheter dysfunction