Antecedentes: Los pacientes con enfermedad renal crónica (ERC) tienen con frecuencia patología cardíaca asociada. La coincidencia de ambos procesos puede potenciar la inflamación, aumentando los requerimientos de eritropoyetina (EPO) y empeorando la supervivencia. Objetivos: Conocer la prevalencia de patología cardíaca, su influencia en la dosis de EPO y la de ambos factores sobre la mortalidad en pacientes con ERC 4-5 no-D (no diálisis). Métodos: 134 pacientes (68% con EPO al inicio y el 72,3% a lo largo del seguimiento) seguidos durante 36 meses. Para evaluar la respuesta a la EPO se utilizó su índice de resistencia a la eritropoyetina (IRE): dosis de EPO semanal/peso/hemoglobina (Hb); el IRE se estimó basalmente y durante el período de los seis meses precedentes a la finalización del estudio. Resultados: 39 pacientes (29,1%), antecedentes de cardiopatía; 22 (16,4%), episodios de insuficiencia cardíaca (IC). El IRE fue superior en los pacientes con antecedentes de cardiopatía, con IC y en los tratados con inhibidores de la enzima convertidora de angiotensina/antagonistas de los receptores de angiotensina II; en el análisis multivariante (IRE como variable dependiente) compusieron el modelo final: ferritina, Hb, función renal y episodios de IC. Durante el período de seguimiento, 39 pacientes fallecieron. La supervivencia (Kaplan-Meier) a los 36 meses fue inferior en los pacientes con un IRE superior a la mediana (2,6 UI semana/kg/g de Hb en 100 ml) (p = 0,002), los que habían sufrido episodios de IC (p = 0,001) y los que tenían antecedentes de cardiopatía (p < 0,001). Conclusiones: Los pacientes con antecedentes cardiológicos en general y de IC en particular tienen un IRE aumentado. Tanto la presencia de estos antecedentes como un mayor IRE se asocian a la disminución de la supervivencia, pudiendo considerarse el IRE como marcador de riesgo de muerte a corto-medio plazo.
Introduction: Patients with chronic kidney disease (CKD) frequently suffer from heart disease as well. The combination of the two processes can exacerbate inflammation, resulting in increases in both resistance to erythropoietin (EPO) and mortality. Objectives: The aim of this study was to determine the prevalence of heart disease in a representative group of non-dialysis patients with stage 4-5 CKD, and the influence of that entity on EPO requirements and on mortality during a period of 36 months. Methods: 134 patients (68% on EPO at the beginning, increasing to 72.3% during follow-up) were monitored for 36 months. To evaluate the dose-response effect of EPO therapy, we used the erythropoietin resistance index (ERI) calculated as the weekly weight-adjusted dose of EPO divided by the haemoglobin level. The ERI was determined both initially and during the last six months before the end of the study. Results: 39 patients (29.1%) had history of heart disease; 22 (16.4%) had suffered from heart failure (HF). The ERI was higher in patients with a history of heart disease or HF and those treated with drugs acting on the renin-angiotensin system (ACE inhibitors or ARBs). Using ERI as the dependent variable in the multivariate analysis, the variables that composed the final model were ferritin, haemoglobin, glomerular filtration rate and history of HF. The 36 month mortality rate (n=39 patients) was higher in the group having ERI above the median (2.6IU/week/kg/gram of haemoglobin in 100ml) (P=.002), and in the groups with heart disease (P=.001) or HF (P=.001) according to the Kaplan-Meier survival analysis. Conclusions: Patients with history of heart disease or HF have a higher ERI, and all of these characteristics are associated with lower survival. ERI can be considered a marker for risk of death in the short to-medium term.
INTRODUCTION
The main factor causing the anaemia associated with chronic kidney disease (CKD) is a decrease (both absolute and relative) in the synthesis of erythropoietin (EPO). Inadequate response to treatment with exogenous EPO is described in 10% of patients with CKD.1 Anaemia is also common in patients with heart disease in general and heart failure (HF) in particular2; the most common form is anaemia associated with chronic disorders.3 In this case, we observe a relative EPO deficit — resistance to endogenous EPO — in conjunction with inhibition of iron uptake, and both conditions are largely provoked by an increase in cytokines.4 Inflammatory processes are usually accompanied by an increase in hepcidin which impedes the release of iron by intestinal cells and those in the mononuclear phagocyte system. Inflammation is an important factor in HF and CKD. In the latter process, the increase in hepcidin is favoured by the reduction in the amount excreted renally.5 In both conditions (CKD and HF), decreased availability of Fe is a factor that exacerbates anaemia.
In patients who suffer from both conditions simultaneously (chronic cardiorenal syndrome types IV and V, according to the Ronco classification6), EPO resistance is logically more common. These patients need to take larger doses of EPO in order to maintain similar haemoglobin (Hb) levels, as seen in prior studies conducted in patients on haemodialysis with a history of HF.7
This study has a dual purpose: a) to examine the prevalence of heart diseases in general and HF episodes in particular, and determine their influence on the EPO doses administered in a representative sample of our stage 4-5 CKD patients; b) use this CKD population to prospectively study the influence of pre-existing heart disease and EPO requirements on patients’ 3 year survival rates.
MATERIAL AND METHOD
The study was both cross-sectional (for the prevalence analysis) and longitudinal (for the survival analysis), and included all patients attended in sequential order in our Advanced Chronic Kidney Disease (ACKD) Unit from the beginning of January to the end of February 2008. The follow-up period ended on 28 February 2011 and included the patient’s status at the end of that period (outpatient monitoring, on dialysis, transplant recipient or deceased). No patients were excluded from the overall study of heart disease prevalence and survival. We recruited 134 patients, representing 16% of the 824 patients attended in our Unit throughout 2008. One patient was positive for the hepatitis B virus and another for hepatitis C. We excluded 2 patients from the baseline analysis of the subgroup of patients on EPO treatment (n=91) due to severe associated conditions (cirrhosis of the liver with advanced portal hypertension in 1 case; chronic infectious process associated with an enterocutaneous fistula following radiotherapy in the other) and who required EPO doses higher than 20 000IU/week. The baseline study therefore contained the remaining 89 patients. In addition, 6 patients who were not being treated with EPO at the time of recruitment either began or returned to treatment throughout the 3-year follow up period. The study of survival according to EPO dose therefore contained 97 patients. In summary, 89 patients participated in the baseline study and 97 participated in the study of survival according to EPO dose.
Using patients’ medical histories, we recorded demographic and anthropometric data, mean blood pressure, CKD aetiology, history of heart disease including ischaemic heart disease (acute myocardial infarction or angina diagnosed and monitored by the Cardiology department), severe valvular heart disease or arrhythmia (atrial fibrillation in all cases) and history of heart failure episodes, defined as left ventricular failure manifesting as dyspnoea of cardiac origin which required hospital treatment, and was considered or diagnosed as such in the patient's medical history. We also gathered data regarding treatment with angiotensin converter enzyme inhibitors (ACE inhibitors) or angiotensin II receptor blockers (ARB), date of death and cause of death when known. During follow-up, 39 patients died (33 in the outpatient monitoring programme and 6 after beginning dialysis).
All patients undergoing treatment received subcutaneous EPO beta (erythropoietin beta) EPO requirements were measured using the erythropoietin resistance index (ERI): weekly units of EPO/weight in kg/Hb in g per 100ml. The baseline ERI recorded at the beginning of the study was used to analyse survival in patients who started dialysis or died during the first year of follow-up. For patients who began dialysis or died after the first year, we used mean ERI, referring to the arithmetic mean of the baseline ERI and final ERI. The latter refers to indices calculated with data gathered during the 6 months prior to death, initiation of dialysis or the end of the follow-up period. As a result, mean ERI corresponds in some cases to baseline ERI and in others to the mean of baseline ERI and final ERI in the survival study.
We analysed the following parameters: C-reactive protein (CRP), homocysteine, haemogram, Fe deposits, renal function as measured by creatine clearance in urine over 24 hours and the estimate given by the Cockcroft-Gault equation normalised according to body surface area (calculated using the Mosteller formula), uric acid, Ca-P metabolism, parathyroid hormone and proteinuria. The Charlson comorbidity index was used to indicate comorbidity.
Statistical analysis was performed using IBM SPSS software version 18. The descriptive population study used absolute and relative frequencies for categorical variables; quantitative variables were represented by the median and typical deviation for the total population, while median, 25th percentile and 75th percentile were used in study subgroups since they did not follow a normal distribution. When comparing groups according to ERI being above or below the median, we used the Mann-Whitney U-test for quantitative variables and chi-squared for qualitative variables. Spearman's rank correlation coefficient was used to study correlations between EPO dose and different variables. Variables with an effect on ERI were analysed using forward stepwise linear regression, with ERI as a dependent variable. The survival study was carried out using Kaplan-Meier curves (log-rank test).
RESULTS
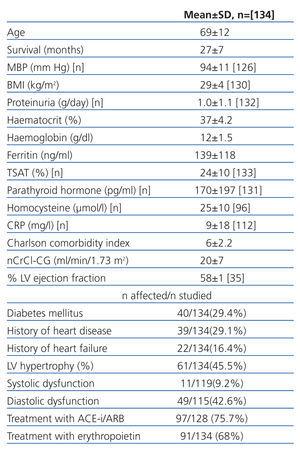
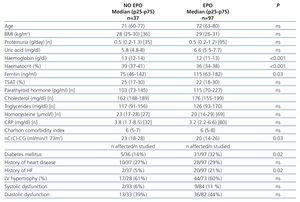
Causes of CKD among the 134 patients in the study (51% men, 49% women) were as follows: 36% vascular nephropathy; 27% diabetic nephropathy; 10% tubulo-interstitial nephritis of different aetiologies; 10% unknown causes; 8% chronic glomerular disease diagnosed by renal biopsy; 4% polycystic renal disease; 5% systemic conditions (systemic lupus erythematosus, rheumatoid arthritis, Sjögren’s syndrome, atypical haemolytic-uraemic syndrome). At the beginning of the follow-up period, 91 patients were being treated with EPO (68%); 97 received treatment at some point during that period (72.3%). High blood pressure was present in 96% of patients, and 75.7% of these patients were treated with ACE inhibitors/ARB. A history of heart disease was present in 39 patients (29.1%) and 22 patients (16.4%) had a history of HF episodes. According to echocardiographic data, 61 patients (45.5%) had left ventricular hypertrophy, 49 (42.6%) had diastolic dysfunction and 11 (9.2%) had systolic dysfunction. Table 1 lists this data and other data of interest for the entire group.
Subgroup of patients with erythropoietin
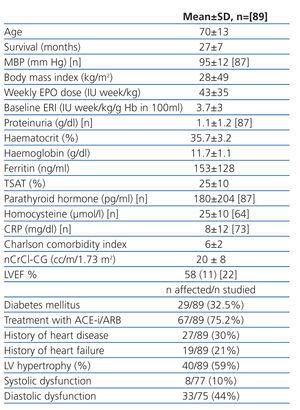
Baseline data for the subgroup of 89 patients (56% women, 43% men) treated with EPO at the outset of the study, after exclusion of the 2 patients mentioned previously, are shown in Table 2.
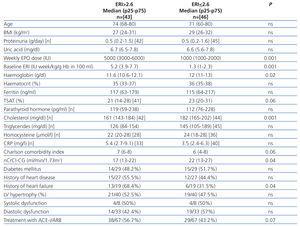
When comparing these patients according to whether baseline ERI was above or below the median (2.6IU/kg/g in 100ml) (Table 3) we find significant differences in their cholesterol levels (P<.001), renal function estimated using the Cockcroft-Gault equation normalised for a body surface area of 1.73 m2 (P=.04) and Hb (P=.007). TSAT and the Charlson comorbidity index almost reached the statistical significance level (P=.06 in both cases).
Comparison of different qualitative variables revealed that the percentage of patients with a history of HF was higher in the group whose ERI was above the median (P=.04). There were no significant differences with regard to sex, percentage of diabetes mellitus, history of heart disease in general, echocardiographic abnormalities, or in the percentage of patients treated with ACE inhibitors/ARB. However, patients treated with ACE inhibitors/ARB had a higher baseline ERI than the untreated group: median 2.3 (p25-75: 1.1-4.9) vs 3.6 (p25-75: 2.5-7) IU/kg/g Hb (P=.01).
We found a significant correlation for baseline ERI which was positive for P levels (r=0.246; P=.02) and negative for CrCl (r=–0.373; P<.001), Hb (r=–0.323; P=.002), haematocrit (r=–0.216; P=.04), cholesterol (r=–0.442; P<.001) and triglycerides (r=–0.200; P<.03).
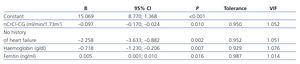
Multivariate analysis was conducted using forward stepwise linear regression and the range of variables traditionally related to each dose of EPO (measured by the baseline ERI): Charlson comorbidity index, Hb, ferritin, transferrin saturation index, renal function estimated using the Cockcroft-Gault equation normalised for body surface area, history of HF (analysed as absence of HF history) and history of heart problems in general, diabetes mellitus and sex. Of the variables listed above, ferritin, Hb, renal function and lack of history of HF were the variables used in the final model (Table 4).
Evolution at 36 months
During the 36 month period in which 134 patients were monitored, 31 (23%) began dialysis, 4 received pre-emptive transplants (3%) and 66 (49%) remained in the ACKD Unit. There were 39 deaths (29%): 33 in an ACKD unit outpatient monitoring programme and 6 after beginning renal replacement therapy. None of the patients receiving transplants died. Causes of death among all 39 patients were as follows: cardiovascular, 18 (46%); infection, 7 (18%); neoplasia, 6 (15%); other, 2 (5%) (1 patient due to cirrhosis and the other due to digestive tract haemorrhage); cause unknown in 6 (15%) (occurred at home or another hospital, or we were unable to contact the family, or the family did not know cause of death).
As mentioned in the “Material and Method” section, when analysing 3 year survival according to EPO dose, measured as mean ERI (97 patients, mean: 3.3±2.5IU/kg/g Hb; range: 0.5-13.1IU/kg/g Hb; median: 2.5IU/kg/g Hb) we considered all patients receiving EPO treatment at the time of recruitment plus the other 6 who began EPO treatment at a later date, for a total of 97 patients.
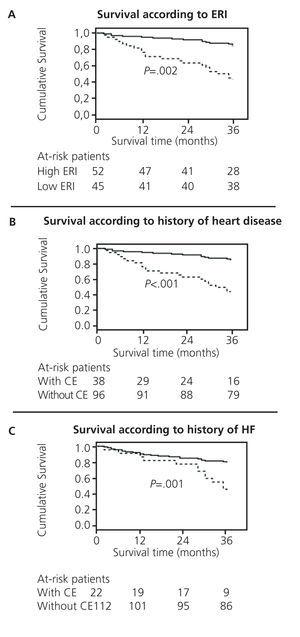
The Kaplan-Meier survival study showed that patients whose mean ERI was higher than the median (2.6IU/kg/g Hb) had lower survival rates (log-rank P=.002) (Figure 1). Likewise, patients with a history of HF also had lower survival rates: log-rank P=.001 (Figure 2), as did patients with a history of general heart disease, with log-rank P=<.001 (Figure 3).
Patients not treated with erythropoietin
Different quantitative and qualitative variables were compared between the groups of patients treated with EPO (97 patients) and those who never received EPO (37 patients) during the 3 year follow-up or prior to that follow-up period. Statistically significant differences were found for levels of Hb, Hct (both higher in patients without EPO), ferritin (lower in patients without EPO) and renal function (higher in patients without EPO). There were also lower percentages of diabetes mellitus (DM) and history of HF among patients without EPO treatment. Results are shown in Table 5.
There were no statistically significant differences between survival of patients treated with EPO and survival of untreated patients according to the Kaplan-Meier survival study (log-rank test P=.1).
DISCUSSION
This study shows that a representative sample of non-dialysis CKD patients in stages 4-5 undergoing regular monitoring by our ACKD Unit had high comorbidity - 6 on the Charlson index - and a high prevalence rate for heart disease. The sample is representative because it consists of patients seen at the clinic in sequential order, without any type of selection process. Atherosclerosis increases with age; CKD may be just another sign of that process, as is true for atherosclerosis in other locations (heart, brain, peripheral arteries). Ageing of the population as life expectancy increases is also extending exposure time to CKD risk factors, and this causes the alarming increase in CKD worldwide.8,9
Response to EPO was evaluated by using ERI, as has been done in prior studies.10,11 This index relates the dose administered per kg body weight with the Hb level achieved; high values indicate the presence of mechanisms that slow erythrocyte response. It also serves a prognostic purpose, since increased EPO resistance is associated with increased risk of death among patients on haemodialysis.7,12 Our study also confirms its usefulness in ACKD outpatients not on dialysis, since the percentage of patients with an ERI above the median (2.6IU/kg/g Hb) was higher among patients who died. This tendency is confirmed by the survival analysis. A recent article,13 drawing on data from the TREAT study14 conducted in diabetic patients with stage 3-4 CKD, evaluates response to darbepoetin by means of the percentage of change in Hb after the first 2 doses. The article observed increased mortality and increased incidence of cardiovascular events among patients in the lowest quartile for Hb response to darbepoetin.
Our study clearly shows that patients with a history of HF need larger doses of EPO. This fact was confirmed by the multivariate analysis in a model containing history of HF, renal function parameters and Hb and Fe deposits. We believe that this supports the existence of a relationship between ERI and HF in our group of patients. Resistance to EPO in patients with HF has already been observed in patients on haemodialysis.7 This would explain why the simultaneous presence of both diseases gives rise to a low-grade state of inflammation, with increased production of inflammatory cytokines (IL-1, IL-6, TNF, interferon, etc.) which induce apoptosis in erythroid progenitor cells and decrease Fe availability by stimulating hepcidin production.4
When we analyse and compare different characteristics between patients with and without EPO treatment, we observe that patients with EPO have lower incidence rates of HF and DM, as well as higher Hb levels. However, having this patient profile, which is theoretically healthier, does not result in differences in survival, or at least this is true in our group. We cannot rule out the possibility that in a larger sample, patients who do not need EPO could show better survival rates than those treated with EPO.
Although CRP level, which is considered an inflammation parameter, was higher among patients with a more elevated baseline ERI, the difference was not significant. This fact could be explained by a considerable dispersion among the values that were recorded; the median CRP value in patients with a higher ERI was clearly superior to that in the lower ERI group. The study mentioned above13 which made use of TREAT study data from diabetic patients with stage 3-4 CKD also observed higher CRP levels in patients with the most moderate response to the first doses of darbepoetin. Likewise, this relationship between EPO response and inflammation has also been observed with levels of endogenous EPO. A recent study analysed endogenous EPO levels in patients with DM and CKD (mean CrCl 50cc/min), examining different parameters and their effect on mortality after a 7 year follow-up period. That study showed higher endogenous EPO levels in patients with higher CRP levels and a history of cardiovascular disease, as well as increased mortality in that patient group.15
Homocysteine levels tend to be high during renal failure because of the decrease in urinary elimination.16,17 Although increase in homocysteine levels is associated with higher vascular risk, we found no significant differences in patients with a higher ERI. This could be because the factor with the greatest effect on homocysteine serum levels is renal function, and this was similar in both groups.
Baseline ERI was negatively correlated with renal function (also true in the linear regression model), as might be expected, since synthesis of endogenous EPO is primarily renal and depends on critical functioning renal mass.1 However, a study carried out in patients with stage 3-4 CKD in which response to EPO was evaluated at doses of less than 100IU/kg/week did not find this inverse relation between EPO dose and renal function.18 This could be explained by the fact that these patients had higher glomerular filtration rates (25-60ml/minute) than our own patients. Given these levels of renal function, other factors (age, prior Hb level, Fe deposits, ACE inhibitor treatment, body mass index, proteinuria) could have a greater influence on response to EPO.
In our study, treatment with renin-angiotensin system blockers was shown to have an effect on ERI, which is higher in patients receiving such treatments. This effect was previously described both in patients on EPO, who needed higher doses, and in patients who developed anaemia after beginning ACE inhibitor or ARB treatment.19 Although the underlying mechanism is not completely understood, we know that angiotensin II regulates circulating EPO levels in both normal individuals and CKD patients, and that activation of the RAS increases EPO levels. Therefore, using renin-angiotensin system blockers will decrease endogenous EPO levels, exacerbate anaemia and increase the need for exogenous EPO.20
The serum cholesterol level was inversely correlated with baseline ERI. This relationship has been described in patients on haemodialysis,21 and the reason is that low cholesterol levels are a marker for the presence of malnutrition and inflammation. This in turn would explain lower survival in these patients, which is contrary to what occurs in the population without CKD. The same trend occurs with obesity among haemodialysis patients (this has not been found consistently among patients on peritoneal dialysis). In this group, obesity does not increase cardiovascular risk, unlike what happens in the general population; this is part of the so-called “reverse epidemiology” described by the DOPPS study.22
When evaluating the relationship between EPO dose, ERI and Hb level in patients with CKD and HF, it is important to keep in mind the complexity of administering EPO treatment in this situation, which is becoming increasingly common. The Hb level may fall and rise in an “unreal” way depending on the intensity of diuretic treatment and the simultaneous presence of oedemas (haemoconcentration and haemodilution). Due to these reasons, the EPO dose may change without variation in the real mass of red blood cells, and therefore the nephrologist must adjust the EPO dose for these patients, while considering the effect which changes in plasma volume will have on the Hb concentration.23-25
One of this study’s limitations is that it contains a small number of patients. It does, however, have the advantage of being homogenous, since it was conducted in one centre with a single observer and a consecutive array of patients who had the same therapeutic criteria, and these characteristics reduce population and observer biases. To compensate for the bias occurring from correlating baseline ERI with a patient’s evolution over 3 years of follow-up, we took a second ERI measurement (in the 6 months prior to exitus, beginning dialysis or the end of follow-up for patients still treated on an outpatient basis) and used the mean ERI for studying survival. With this approach, we are able to reconcile ERI with the evolution we observed. All things considered, this study and its conclusions have the same limitations as any survival analysis, including the low rate of events in some groups which does not permit us to calculate median survival, risk over time, etc.
One aspect that makes this study a useful contribution to the literature is that few studies analyse the progression of patients with advanced CKD (non-dialysis stage 3-4 CKD) with regard to cardiac morbidity, which is very prevalent and likely to increase given the population profile and its current tendencies.
Although some of the findings from studies of patients on dialysis mirror those in earlier stages of CKD, important differences are present. ERI and EPO dose per kg in non-dialysis CKD stage 4-5 are much lower to those recorded for patients on haemodialysis. In the article by López Gómez7 describing a multi-centre Spanish study of patients during the first year of inclusion in a haemodialysis programme, mean ERI was 10.2±7.3IU/kg/g Hb, while ERI in our study was 3.7± 3IU/kg/g Hb, just over a third of the other index. It is likely that better renal function among our patients and absence of the negative effects of haemodialysis are the main factors accounting for this difference, since comorbidity (the Charlson comorbidity index), the percentage of heart disease and age are quite similar.
As a group, patients with CKD and a high ERI have the following profile: history of heart disease in general or, more specifically, episodes of HF; higher Charlson comorbidity index and ferritin levels; lower renal function, Hb and cholesterol levels.
In summary, this study shows a high prevalence of heart disease among patients attended by the ACKD outpatient unit. Simultaneous presence of CKD and HF increases the need for EPO, both in terms of absolute value and with regard to Hb levels, expressed as the resistance index. Likewise, both a history of heart disease/HF episodes and high ERI seem to be associated to poorer survival, and both may be considered markers of increased risk of mortality over the short to medium term. High ERI may be a marker for patients requiring increased diagnostic and therapeutic intensity.
Conflicts of interest
The authors affirm that they have no conflicts of interest related to the content of this article.
Table 1. Patient characteristics (full group)
Table 2. Patient characteristics (subgroup on erythropoietin)
Table 3. Erythropoietin resistance index (ERI)> or &
Table 4. Forward stepwise linear regression analysis
Table 5. Patients with or without erythropoietin treatment
Figure 1. Survival analysis