Introducción: En la insuficiencia renal aguda (IRA), la dosis administrada no suele controlarse y se estima que resulta inferior a la prescrita. Objetivo: Evaluar la diferencia entre la dosis prescrita y la dosis administrada en pacientes con IRA en Unidades de Cuidados Intensivos (UCI), así como los factores que la determinan, utilizando la determinación del Kt por dialisancia iónica. Material y método: Se incluyeron 394 terapias de reemplazo renal (TRR) en 105 pacientes adultos, con IRA oligúrica ingresados en UCI, con requerimiento de TRR , tratados con hemodiálisis intermitente (HDI) y/o extendida (HDE). Las TRR fueron realizadas con un monitor de aclaramiento on line (OCM®, Fresenius) para la determinación del Kt. Se registraron las características de los pacientes, la prescripción y el desarrollo de TRR. Todas estas variables fueron incluidas en un modelo uni y multivariado, teniendo como variable dependiente la incapacidad de lograr la dosis umbral u objetivo (DU). Resultados: Edad 66 ± 15 años, 37% del sexo femenino, etiología más frecuente: sepsis (70%), hipotensión y/o requerimientos de inotrópicos (71%), asistencia respiratoria mecánica (70%); el índice de severidad individualizado promedio fue de 0,7 ± 0,26. Se efectuaron 201 HDI y 193 HDE, la vía de acceso vascular más frecuente fue la femoral (79%). El Kt prescrito fue de 53,5 ± 14 litros, y un 21% de las prescripciones estaban por debajo de DU. En el 61% no se logró el nivel de cumplimiento de la DU (31 ± 8 litros), vs. 56 ± 12 litros en el subgrupo que logró el nivel de cumplimiento. El Kt obtenido por las HDE fue significativamente mayor (46 ± 16 litros vs. 33 ± 9 litros en HDI). En el análisis univariado, el nivel de cumplimiento insuficiente estuvo relacionado con la edad (> 65 años), el sexo (masculino), la presencia de hipotensión intradiálisis, no lograr el flujo de sangre prescrito, la inversión de las ramas del catéter y la HDI. Las mismas variables estuvieron independientemente relacionadas en el modelo multivariado, con excepción de la edad y el género. Conclusiones: La dosis de diálisis administrada fue significativamente inferior a la prescrita. Las HDE exhibieron un Kt más cercano a DU y significativamente mayor que las HDI. El funcionamiento adecuado del acceso vascular, sin la necesidad de inversión de las ramas del catéter, y el hecho de evitar la inestabilidad hemodinámica durante la TRR constituyen dos de los factores más importantes para lograr la DU, particularmente en ancianos y varones. Debe prescribirse y controlarse la dosis de diálisis en pacientes críticos con IRA.
Background: Estimating the dialysis dose is a requirement commonly used to assess the quality of renal replacement therapy (RRT) in patients with chronic kidney disease (CKD). In patients with acute kidney injury (AKI), this value is not always evaluated and it has been estimated that the prescribed dose is seldom obtained. Reports addressing this issue in AKI individuals are scarce and most have not included an adequate number of patients or treatments, nor were patients treated with extended therapies. Kt values obtained by the ionic dialysance method have been validated for the evaluation of the dialysis dose and it has also been shown that, compared with Kt/V, this is the most sensitive strategy for revealing inadequate dialysis treatment in critically ill AKI individuals. The main aim of this study was to assess the difference between the prescribed and the administered dialysis dose in critically ill AKI patients, and to evaluate what factors determine this gap using Kt values assessed through ionic dialisance. Material and Method: Data from 394 sessions of renal replacement therapy in 105 adult haemodialysis (HD) patients with oliguric acute kidney injury and admitted to ICU were included in this analysis. RRT was carried out with Fresenius 4008E dialysis machines equipped with on-line clearance monitoring (OCM® Fresenius), which use non-invasive techniques to monitor the effective ionic dialysance, equivalent to urea clearance. The baseline characteristics of the study population as well as the prescription and outcome of RRT were analysed. These variables were included in a multivariate model in which the dependent variable was the failure to obtain the threshold dose (TD). Results: The main baseline characteristics of the study population/treatments were: age 66±15 years, 37% female, most frequent cause of AKI: sepsis (70%). Low BP and/or vasoactive drug requirement (71%), mechanical ventilation (70%) and average individual severity index: 0.7±0.26. Two hundred and one intermittent HD (IHD) and 193 extended HD (EHD) sessions were performed; the most frequently used temporary vascular access was the femoral vein catheter (79%). Prescribed Kt was 53.5±14L and 21% of prescriptions fell below the TD. Sixty-one percent of treatments did not fulfill the TD (31±8L) compared with 56±12L obtained in the subgroup that achieved the target. Compared to IHD, EHD provided a significantly larger Kt (46±16L vs 33L±9L). Univariate analysis showed that inadequate compliance was associated with age (>65y), male gender, intra-dialytic hypotension, low Qb, catheter line reversal, and IHD. The same variables with the exception of age and gender were independently associated in the multivariate analysis. Conclusions: The dialysis dose obtained was significantly lower than that prescribed. EHD achieved values closer to the prescribed KT and significantly higher than in IHD. Ionic Kt measurement facilitates monitoring and allows HD treatments to be extended based upon a previously established TD. Besides the chosen strategy to dispense the dose of dialysis, a well-functioning vascular access allowing for optimal blood flow and other approaches aimed at avoiding hemodynamic instability during RRT are the most important factors to achieve TD, mainly in elderly male patients. The dialysis dose should be prescribed and monitored for all critically ill AKI patients.
INTRODUCTION
Acute kidney injury (AKI) is a highly prevalent entity among patients admitted to intensive care units (ICU). According to the population at-risk being studied and the definition used; AKI occurs in 5%-15% of these patients.1-5
Although more than 60 years have passed since the first haemodialysis session was successfully carried out in patients with AKI, the mortality rates associated with this condition in critical patients still range between 30% and 60%,1-6 particularly in patients requiring some type of renal replacement therapy (RRT),1 making AKI an independent risk factor for mortality in this group.2,3,5,6
The different types of RRT used in AKI patients can be classified into intermittent (IHD), extended or hybrid (EHD), continuous, or peritoneal dialysis.7 This last technique is not commonly applied in adult patients, and patients treated with continuous methods are rare in Spain, with IHD and EHD being the most common, taking first and second place, respectively.8
While haemodialysis dosage is important for patients on chronic dialysis, threshold doses (TD) for RRT in patients with AKI in the ICU have not been established.9-12 A study at one hospital showed higher survival and renal recovery rates in patients with daily IHD sessions13; however, the dose administered per session was 0.94Kt/V, far below the recommendations for patients with chronic kidney disease (CKD). A multi-centre study showed that, above a Kt/V of 1.3, no benefits were observed in terms of reduced patient mortality.14 As such, the TD in patients with AKI is generally considered to be close to the applicable target values in patients with CKD, which entails a Kt/V equal to or greater than 1.2, a percent reduction in urea (PRU) equal to or greater than 65%, or a Kt greater than 45 or 40 in males and females, respectively.15-17
However, in normal clinical practice, in contrast to patients with CKD, the doses administered to AKI patients go uncontrolled, and it is widely estimated that we do not reach the prescribed dose.18,19 Few studies have evaluated this issue as a primary objective in patients on IHD with an adequate number of patients and treatments, and none has performed such an evaluation in EHD. In this context, critical patients would be at an even greater risk of not receiving the prescribed dose.20
The most commonly used methods for evaluating the dose administered in patients with AKI have been the Kt/V formula or URR. The Kt/V formula, which is routinely used in CKD patients, has limited applications in critical patients, since this group tends to have a varying and unpredictable urea distribution volume.21 While determining URR is a simple process, the calculation is made retrospectively, making it impossible to monitor levels during treatment to verify reaching the prescribed dose.22 Calculating dialysis dose through direct quantification of dialysate would be the most reliable method to use in AKI patients, compared to other options.23 Measuring Kt through ionic dialysance provides a direct measurement of the dialysis dose being administered without the need for blood or dialysate samples for measuring urea levels, and this method has been validated for patients with both chronic and acute kidney injury.24-26 It has recently been shown that measuring the dose of dialysis using Kt as determined through ionic dialysance is more sensitive for revealing inadequate treatment than Kt/VUREA in critical patients with AKI.27
The difference between the prescribed and the administered dose as well as the factors related to this difference are normally monitored in patients on chronic dialysis treatment, Identifying these factors and understanding and correcting them allows for optimizing the dosage given to these patients.
Our objective was to evaluate the differences between prescribed and administered doses in critical patients with AKI and the factors that influence these differences, using Kt measurements through ionic dialysance.
MATERIAL AND METHOD
Our research team was composed of members of the Nephrology, Cardiology, and Intensive Care departments, and the study took place in the Intensive Care Unit (ICU) and Intensive Coronary Care Unit (ICCU) at the Hospital Italiano de Buenos Aires. The study was conducted according to the regulations established by good clinical practices and the Declaration of Helsinki with the modifications established by the Nuremberg and Tokyo Conventions, and was approved by an Institutional Review Board (IRB) - Comite de Protocolos de Investigación (CEPI) - Hospital Italiano.
This was a prospective and observational study involving RRT-requiring adult AKI individuals admitted to the ICU or ICCU, and being treated with intermittent and/or extended haemodialysis. Patients in the ICCU were included due to the extensive cardiological care provided at the Hospital Italiano de Buenos Aires. All baseline characteristics, including sequential organ failure assessment (SOFA), aetiology and classification of the AKI, and the severity of AKI using the individual severity index (ISI) were recorded.28 The type and duration of dialysis was not modified for the purposes of the study, and was administered according to the indications by the attending physician and the type of treatment (intermittent or extended dialysis), registering all of the different parameters of the prescription. Patients were administered dialysis using Fresenius 4008 S monitors equipped with OCM® biosensors (On-line Clearance Monitoring, Fresenius Medical Care AG), devices that use non-invasive methods to measure effective ionic dialysance with conductivity probes. Water used for haemodialysis was obtained through a portable reverse osmosis device (FG Ingenieria). The dialysate flow rates for IHD and extended dialysis were 500ml/min and 300ml/min, respectively. Sterile bicarbonate powder was also used. In all cases, RRT was administered using Fresenius FX® 60 dialysers (helixone filters of 1.4m2, KoA urea 960ml/min). In all cases, the vascular access used were non-tunnelled central venous catheters of 11.5Fr, placed using the Seldinger technique in the femoral vein or internal jugular vein, at 19cm or 16cm, respectively. In the absence of any contraindications, patients were administered standard anticoagulation using sodium heparin in a continuous infusion with a loading dose of 1000 units and a maintenance dose of 500 units per hour. Kt was automatically determined through the aforementioned method, and calculated prescribed Kt based on the type of RRT, blood flow, and time prescribed on dialysis along with in vivo dialyser clearance, which was previously determined in a series of CKD patients on stable haemodialysis.20,29
The following parameters were registered throughout each dialysis session: type of RRT, compliance with the duration prescribed, temporary or definitive suspension, ultrafiltration (millilitres), nominal blood flow, type and location of vascular access, need for catheter line reversal, recirculation of the vascular access, intra-dialysis hypotension (defined as a drop in mean blood pressure of 10mm Hg), need for hypotension treatment (defined as an increase in inotropic drugs and/or saline solution), use of heparin, and coagulation of the dialyser or system. Recirculation of the vascular access was measured by determining plasma urea levels in arterial, venous, and peripheral lines using the low-flow method.30
All data are expressed as mean ± standard deviation or proportions, unless otherwise indicated. Considering a target Kt of 40 for women and 50 for men, we determined compliance with this target for both the prescribed dose and administered dose in each case. We performed a univariate analysis with the dependent variable of compliance and the independent variables were components of the RRT performed and patient characteristics. A a P-value <.05 was considered statistically significant. All variables that had statistical significance or clinical relevance were included in a multiple logistic regression model, with level of compliance with dosage as the dependent variable. Taking into account the number of variables mentioned, we estimated a minimum number of 200 RRT sessions with Kt measurements. We used STATA software version 8.0 for all statistical analyses.
RESULTS
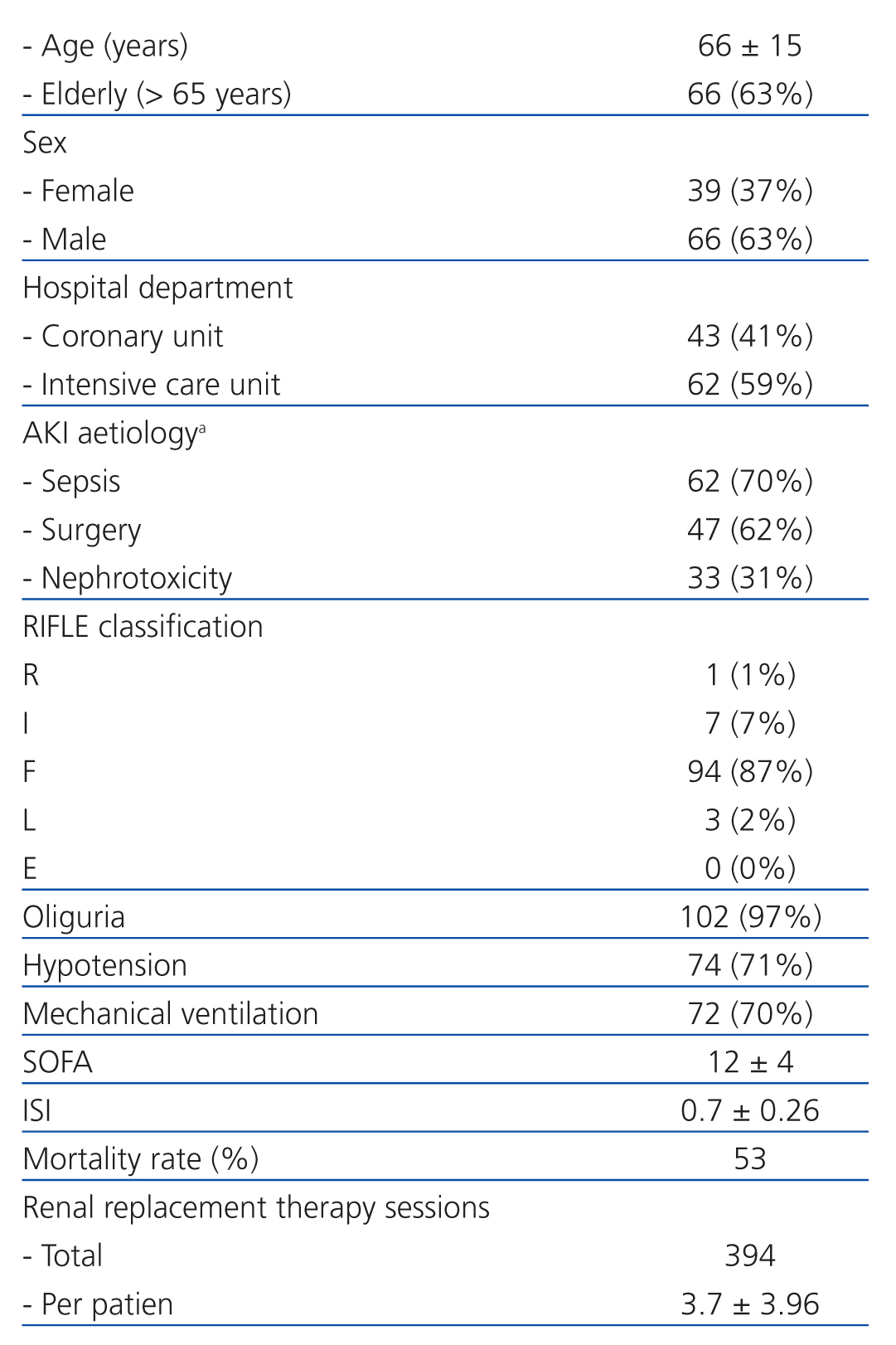
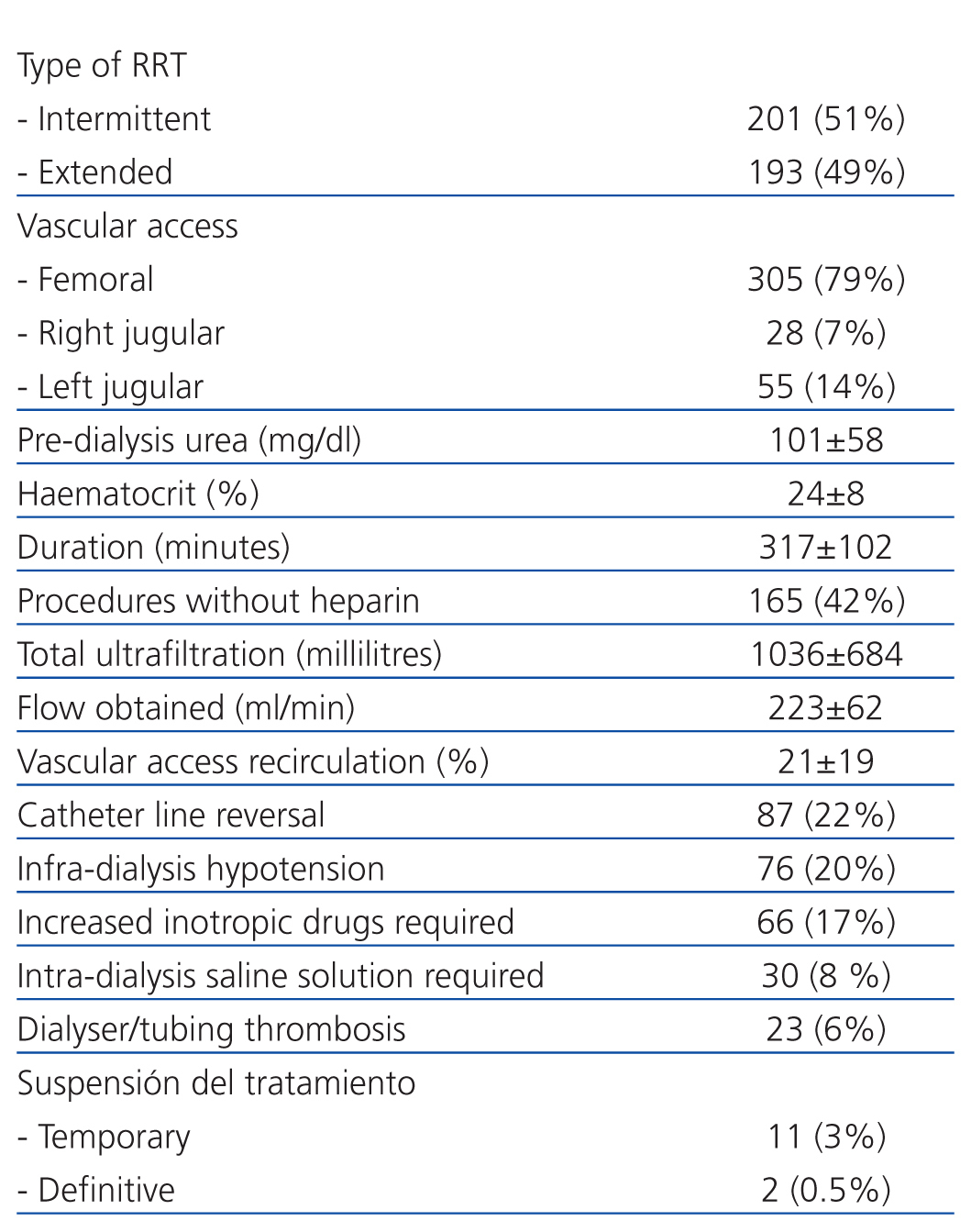
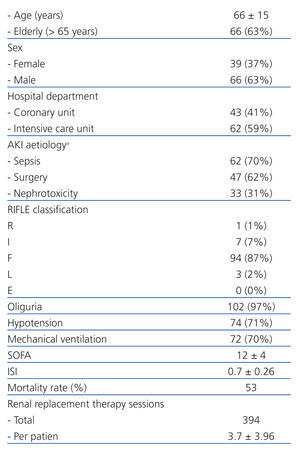
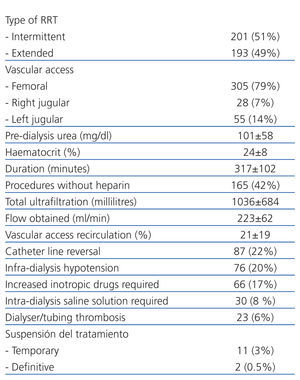
A total of 395 RRT sessions were recorded in 105 patients with AKI in the ICU (3.7±3.96 sessions per patient) from June 29, 2010 through May 24, 2011, Table 1 summarises the characteristics of the study population: mean age: 66±15 years, 37% female, 97% with oliguric AKI, and the most common aetiology was sepsis (70%). These were critical patients, the majority of which had hypotension and/or requirements for inotropic drugs (71%) and required mechanical ventilation (70%). The mean ISI was 0.7±0.26, and the mean SOFA score was 12±4. A total of 201 IHD and 193 EHD sessions were performed, and the most commonly used vascular access was the femoral vein (79%). Serum levels of urea at the start of each haemodialysis session were 101±58mg/dl, and the haematocrit was 24±8 %. Heparin was not administered in 165 sessions (42%), the treatment duration was 317±102 minutes (extended: 408±73 minutes), and the blood flow was 223±62ml/min (extended: 186±17ml/min) whereas the total ultrafiltration per session was 1036±684ml (62% above 1000ml). Vascular access recirculation occurred in 21±19% of cases, with a recirculation of more than 15% in 53% of accesses evaluated. Catheter line reversal was required in 22% of procedures, and recirculation was significantly more common in this instance than when the reversal was not required (recirculation: 25±21 vs 20±18; P<.05). Intra-dialysis hypotension occurred in 20% of RRT sessions, requiring an increased dosage of inotropic drugs in 17% and/or saline solution in 8%. Coagulations occurred in the dialyser in 23 sessions, 11 required temporary suspensions of treatment and then completed the indicated effective time, and 2 required definitive suspension (Table 2).
Mean prescribed Kt was 52.26±13 litres, and 21% of all prescriptions were below the dosage compliance level (lower than 40 litres in women and 45 litres in men). There were no significant differences between the proportion of men and women with a prescribed Kt below the level of dosage compliance (21% in women vs 23% in men).
As regards the dose of Kt administered with an adequate prescription, 185 sessions (61%) did not comply with the prescribed dose, with mean Kt in this sub-group being 31±8 litres vs 56±12 litres in the sub-group that did reach the compliance level.
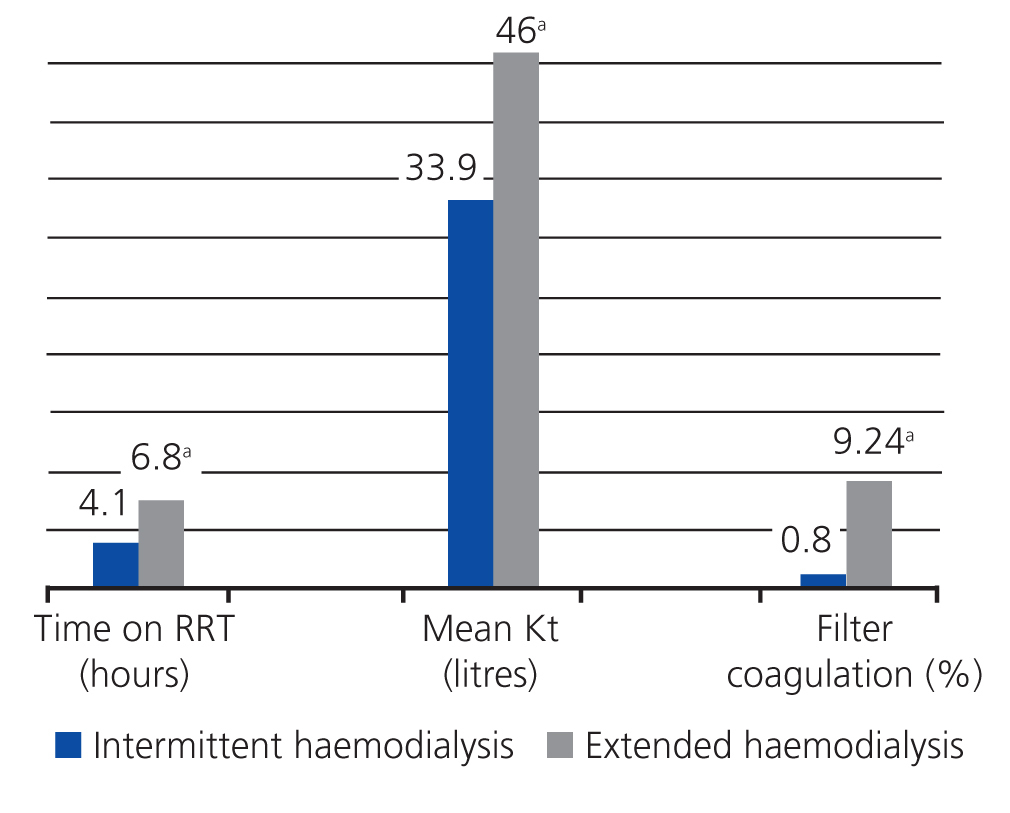
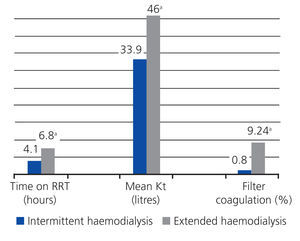
The Kt obtained in EHD sessions was significantly higher than in IHD: 46±16 litres vs 33±9 litres, respectively (Figure 1).
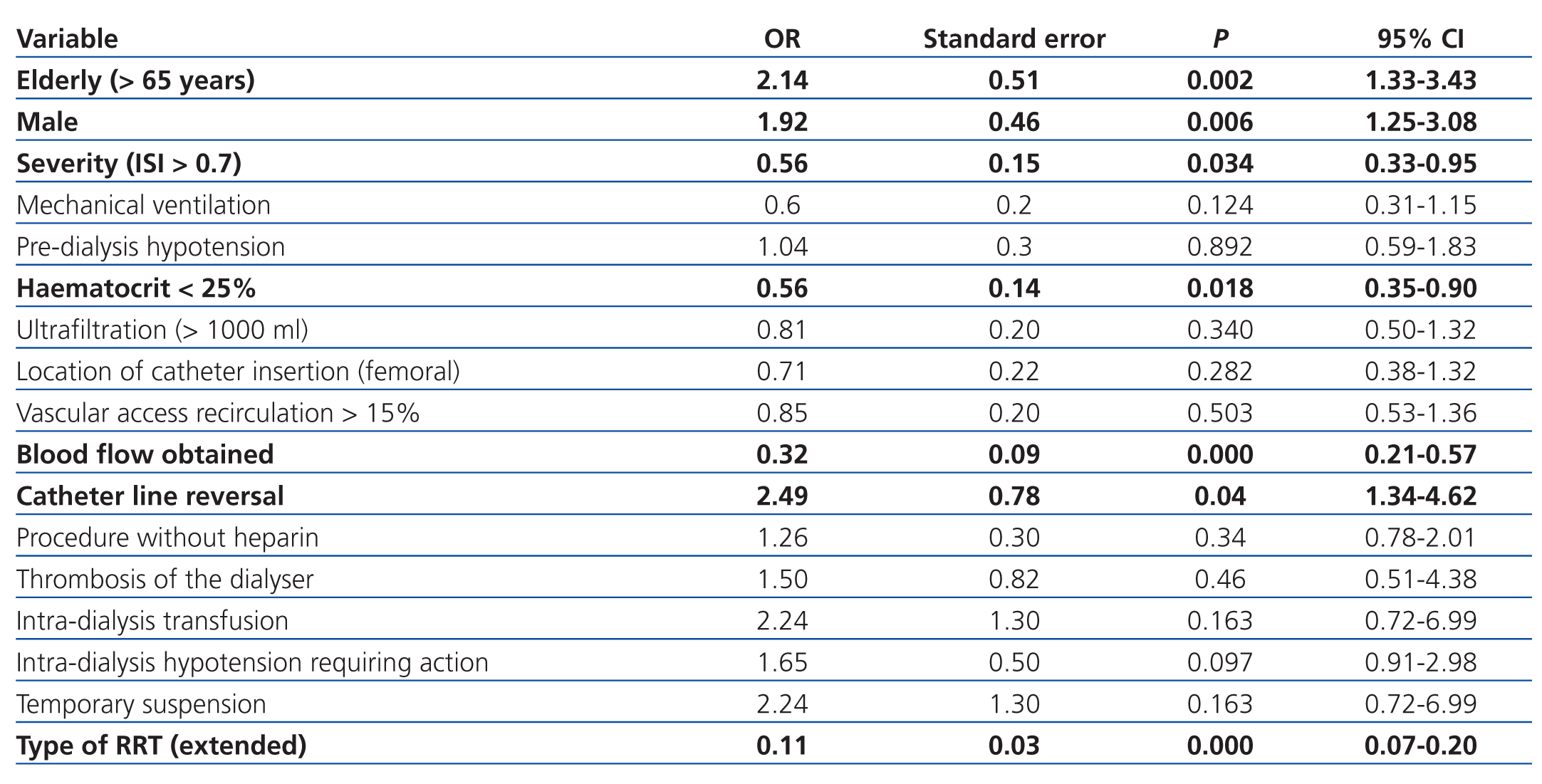
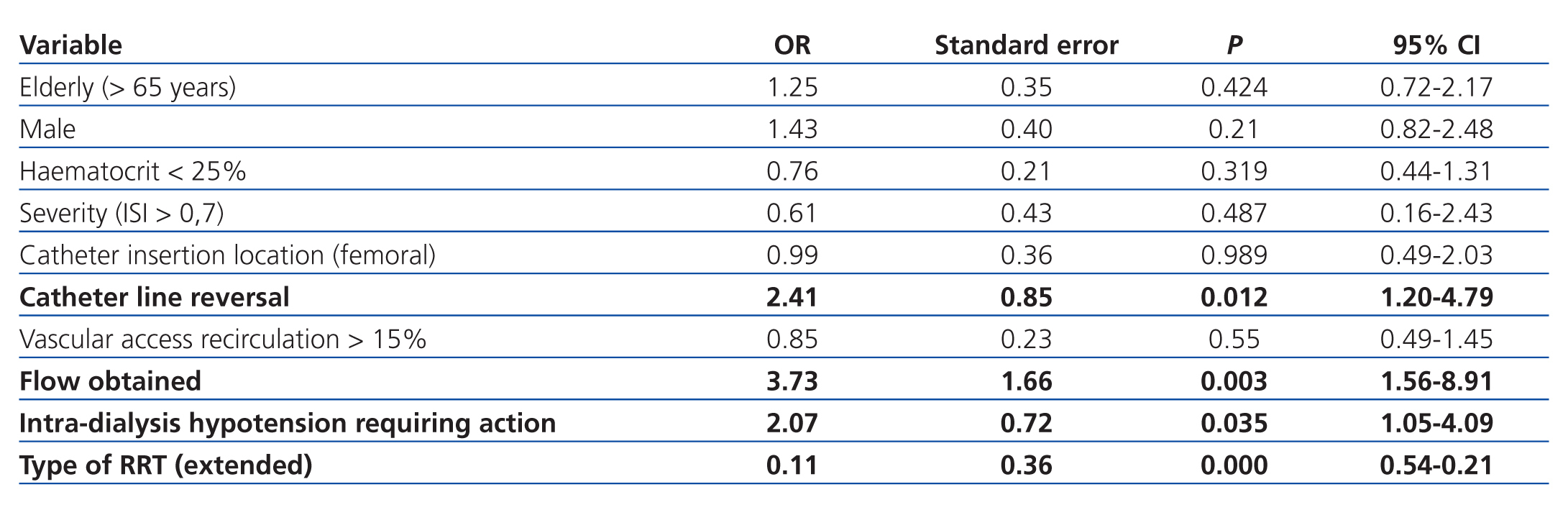
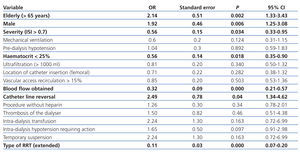
In the univariate analysis, an insufficient level of compliance was significantly correlated with age (older than 65 years), sex (male), severity of illness, anaemia (haematocrit <25), failure to achieve the prescribed blood flow, catheter line reversal, and the type of RRT (IHD) (Table 3).
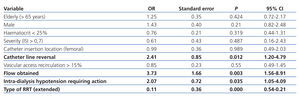
In the multivariate analysis, an insufficient level of compliance was independently correlated with the presence of intra-dialysis hypotension, failure to achieve the prescribed blood flow, catheter line reversal, and intermittent haemodialysis (Table 4).
DISCUSSION
This study demonstrates that a substantial proportion of RRT sessions in critical patients with AKI are inadequately prescribed, and that an even greater proportion does not reach full compliance with the dose prescribed. This is the first study in which ionic dialysance has been applied in a large number of critical patients with AKI in order to achieve the proposed objectives.
As regards our method of measurement for the dosage of dialysis, we believe that it is adequate for this type of patient and treatment. Urea kinetic modelling assumes stability characterised by a neutral nitrogen balance and similar pre-dialysis urea values for each cycle of treatment (haemodialysis). However, this is not valid for patients with AKI, since the majority of critical patients are hyper-catabolic and have a negative nitrogen balance.31 Regional blood flow abnormalities, particularly in unstable patients receiving vasoactive drugs, can produce a disequilibrium In the intercompartmental distribution of urea, which would invalidate the normal single-compartment models for urea,31 over-estimating the dose of dialysis when calculated through blood samples.32 This disequilibrium would be lower in the case of patients treated with extended dialysis,33 and so calculating dialysis dosage through urea kinetic modelling could not be used to compare between intermittent and extended therapies. In contrast, ionic dialysance, using the same principle of direct measurements of solute purification in the dialysate, is an applicable, sensible method that allows for comparing doses between IHD and EHD.25-27
In our study, all variables that could be related to an inadequate dialysis dose were taken into account; the fact that none of these were correlated with non-compliance in both univariate and multivariate analyses (for example, not using heparin) does not imply that these are not important. With regard to the severity of the patients’ conditions, while this has been associated with a greater proportion of insufficient dialysis doses,20 our patients were in severely critical states, since this was part of the primary objective of our study, and this variable is also masked by the type of treatment provided, since the severity of the patient’s condition at the start of treatment was higher in EHD than IHD (ISI: 0.83±0.16 vs 0.69±0.26; and SOFA: 15±3 vs 7±3, respectively).
Age and sex were correlated in the univariate model; a previous study showed that male sex was associated with a higher risk of insufficient dialysis,18 but both variables were not significantly associated in our multivariate model.
The vascular access is of fundamental importance. All patients with AKI require temporary catheters, and, as demonstrated by our results, these imply a high rate of recirculation, regardless of the location of insertion.
While recirculation was more common in femoral catheters than jugular catheters, this difference was not significant, and recirculation was higher than 15% in both cases (22%±19% vs 19%±19%, respectively). Line reversal, which is a common practice when we are unable to achieve proper flow rates, was a prevalent cause for inadequate dialysis, with a high rate of recirculation regardless of the site of insertion. These factors, together with an incapacity to achieve the prescribed blood flow rate, makes the vascular access one of the most important factors in considering the dialysis dose to prescribe in critical patients. As such, when faced with an inability to achieve optimal flow rates, we must consider modifying the treatment regimen by increasing the duration of the session34 and/or the frequency of treatments, or consider using longer catheters (equal to or longer than 20cm for femoral vein insertion) or wider catheters (13Fr).
Independently of other variables, haemodynamic instability during dialysis, which is a common complication in these patients, was another primary cause of inadequate dialysis. This was significantly more common in patients on EHD (23% vs 10% in IHD), which is probably due to the severity of the patient`s conditions, not to the type of RRT per se.
Finally, patients on EHD reached a higher level of compliance than those on IHD. A multi-centre study did not observe this difference,14 but this study had the bias of being a controlled study, since the primary objective was to reach a specific dialysis dosage. Our study attempted to reflect what actually occurs in daily practice, and together with the aforementioned study, supports the arguments set forth by expert opinion: regardless of the controversy surrounding thresholds and methodologies in measuring dialysis dosage, it must indeed be controlled and monitored.9,35 However, EHD is not without its disadvantages; in a secondary analysis, patients on EHD had a significantly higher proportion of dialyser coagulations (Figure 1). However, we should point out that the indication for EHD is related to the haemodynamic state and overall severity of the patient, and this type of RRT allows for reaching objective dosage even in critical patients, with the resources normally available in IHD.36 In our experience, the duration and compliance with time prescriptions for RRT are very important.
Our study had certain limitations, most notably the fact that it was carried out at one single hospital, did not incorporate body weight and surface area for the patients analysed, possibly involved a certain level of heterogeneity in the study population, and Kt was considered to be optimal at its lower limit; however, we used an adjusted fit model, and no previous studies exist in the medical literature of this magnitude in which Kt was used as a measurement of the dialysis dose in critical patients with AKI. Prospective studies that include a comparison of the duration of hospital stay and mortality with weekly Kt doses might better respond to the question of limits for Kt dosage in critical patients with AKI.
In conclusion, the prescribed dialysis dose in critical patients with AKI should be monitored. Ionic dialysance facilitates such supervision, as well as the estimation of extended treatments based on target doses and TD. In addition to the method used for measuring and controlling dialysis dosage, a better functioning vascular access (ensured optimal blood flow without the need for catheter line reversal) and haemodynamic stability during RRT would be the most important factors for achieving TD and other objectives in critical patients with AKI.
Conflicts of interest
The authors have no conflicts of interest to declare.
Figure 1. Comparison of intermittent and extended haemodialysis regimens
Table 1. Characteristics of the study population
Table 2. Characteristics of the treatment provided
Table 3. Univariate analysis of insufficient compliance
Table 4. Multivariate analysis of insufficient compliance