Online haemodiafiltration (OL-HDF) has been associated with increased survival. To date, the influence of the inner diameter of the hollow fibers of the dialyzer on convective volume has not been well established. The objective of the study was to evaluate the effect of increasing the inner diameter of the dialyzer on the convective volume and removal capacity.
Material and methodsWe included 16 patients in postdilutional OL-HDF. Each patient was analyzed in 4 sessions in which the inner diameter varied; 185μm (FX60 Cordiax and FX80 Cordiax) vs. 210μm (FX600 Cordiax and FX800 Cordiax). Different solutes were measured at the beginning and end of each dialysis session.
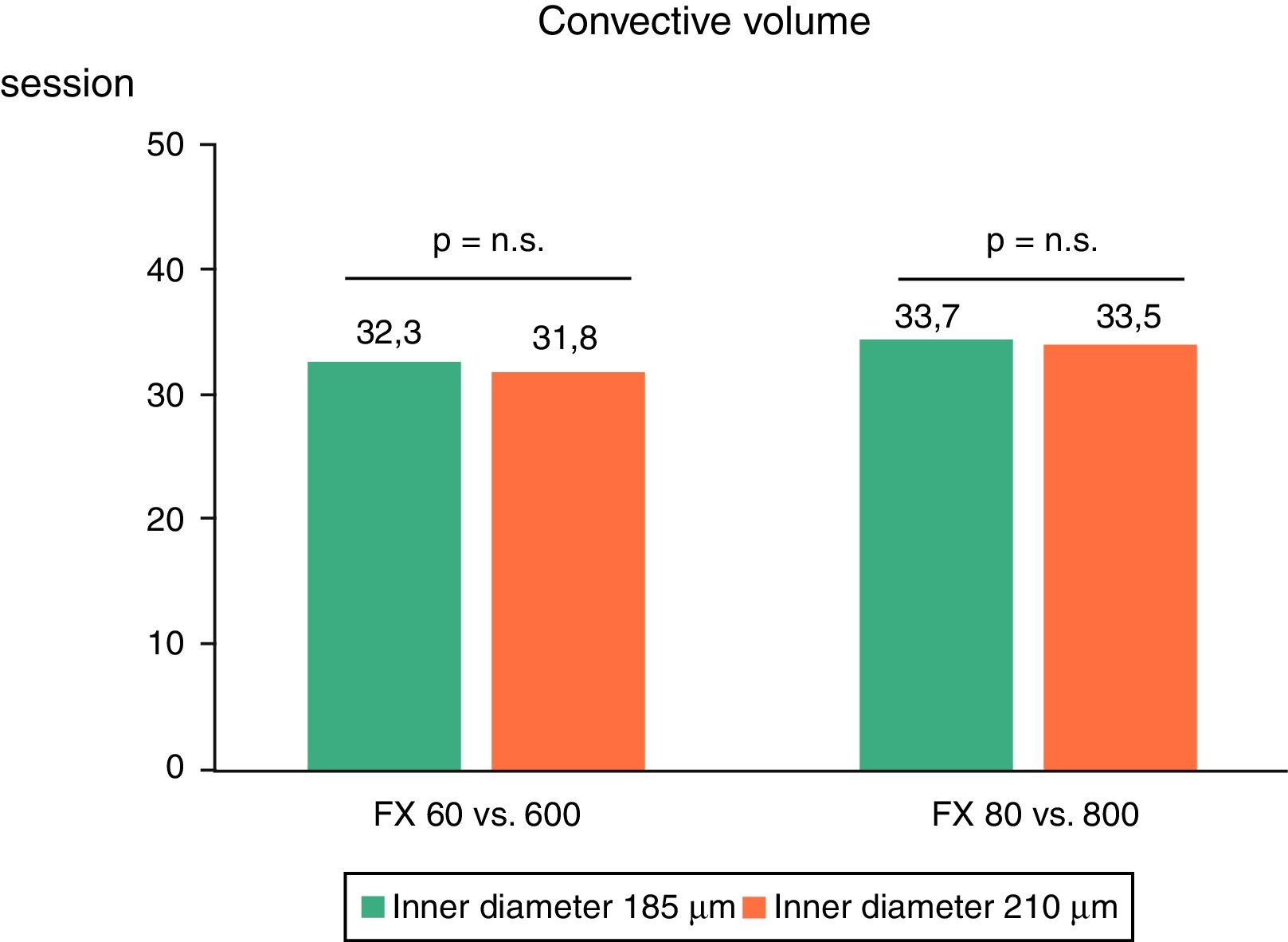
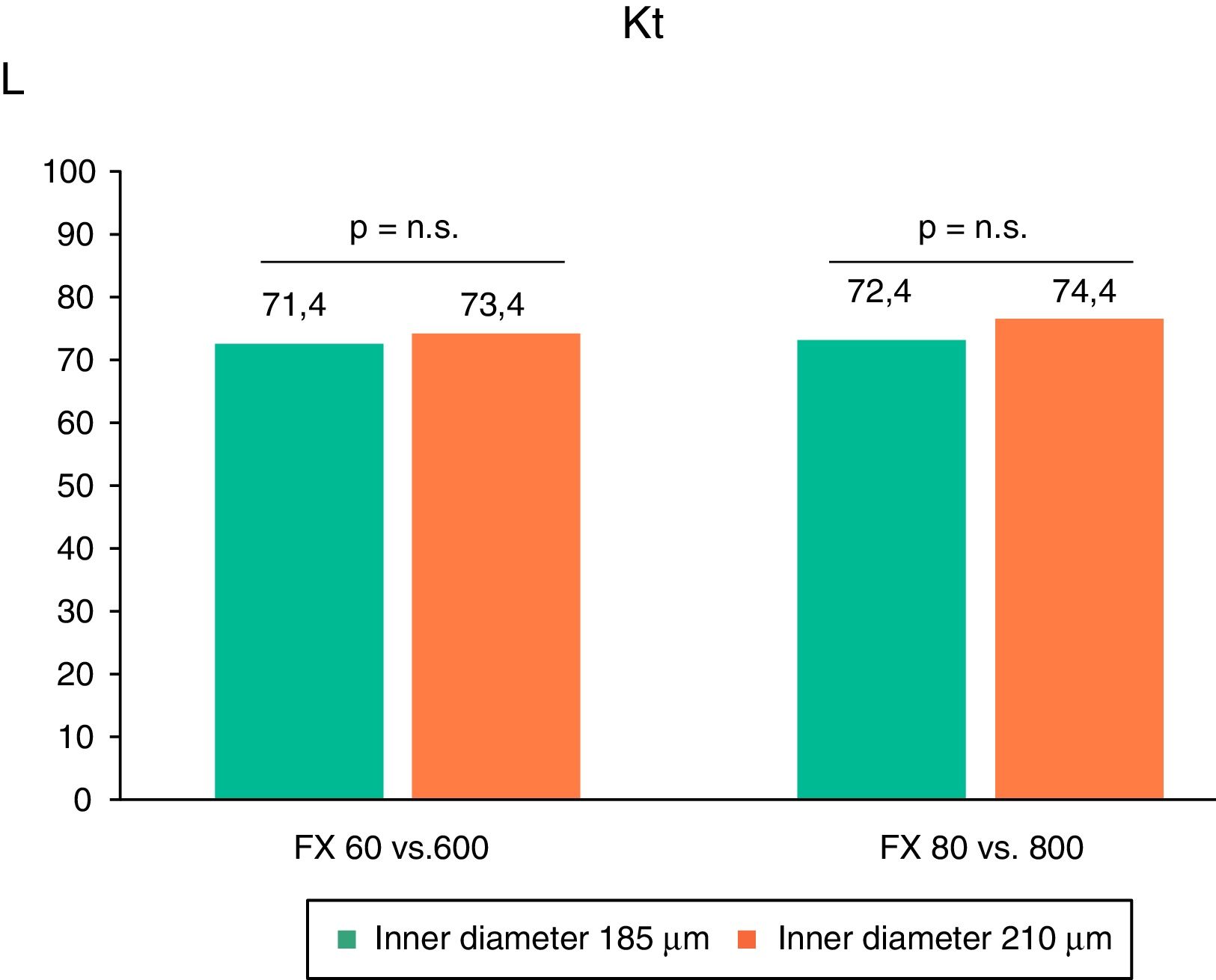
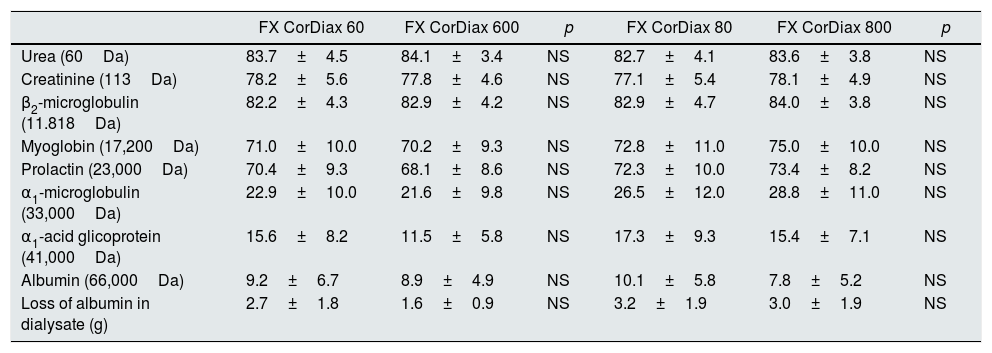
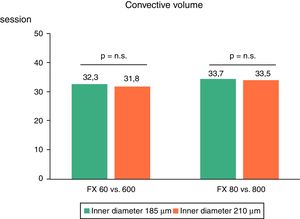
ResultsNo differences in the convective volume were found with an increased inner diameter: 32.3±3.1 vs. 31.8±3.6L/session (FX60 vs. FX600) and 33.7±4.3 vs. 33.5±3.8L/session (FX80 vs. FX800). The reduction ratios also did not differ: urea 83.7±4.5 vs. 84.1±3.4 for FX60 and FX600, and 82.7±4.1 vs. 83.6±3.8 for FX80 vs. FX800; creatinine similar 78.2±5.6 vs. 77.8±4.6 and 77.1±5.4 vs. 78.1±4.9; β2-microglobulin 82.2±4.3 vs. 82.9±4.2, and 82.9±4.7 vs. 84.0±3.8; myoglobin 71.0±10 vs. 70.2±9 and 72.8±11 vs. 75.0±10; prolactin 70.4±9 vs. 68.1±9, and 72.2±10 vs. 73.4±8.2; and α1-microglobulin 22.9±10 vs. 21.6±10, and 26.5±12 vs. 28.8±11, respectively.
ConclusionThe increase in the inner diameter of the hollow fibers did not result in improved convective volume and removal capacity.
Se ha asociado la hemodiafiltración on-line (HDF-OL) a un aumento de la supervivencia. Hasta el momento no está bien establecida la influencia del diámetro interno de las fibras capilares del dializador sobre la capacidad convectiva. El objetivo del estudio fue valorar el efecto del aumento del diámetro interno del dializador sobre el volumen convectivo y la capacidad depurativa.
Material y métodosSe incluyeron 16 pacientes en HDF-OL posdilucional con reposición automática. Cada paciente recibió 4 sesiones, en las que se varió el diámetro interno, 185 μm (FX60 Cordiax y FX80 Cordiax) versus 210 μm (FX600 Cordiax y FX800 Cordiax). En cada sesión se determinaron diferentes solutos al inicio y al final de la diálisis.
ResultadosEl incremento de diámetro interno entre FX60 vs. FX600 y FX80 vs. FX800 no reflejó diferencias en el volumen convectivo: 32,3 ± 3,1 vs. 31,8 ± 3,6 y 33,7 ± 4,3 vs. 33,5 ± 3,8 L/sesión, respectivamente. Los porcentajes de reducción tampoco mostraron diferencias: urea 83,7 ± 4,5 vs. 84,1 ± 3,4 para FX60 y FX600 y 82,7 ± 4,1 vs. 83,6 ± 3,8 para FX80 vs. FX800; creatinina similar 78,2 ± 5,6 vs. 77,8 ± 4,6 y 77,1 ± 5,4 vs. 78,1 ± 4,9; β2-microglobulina 82,2 ± 4,3 vs. 82,9 ± 4,2 y 82,9 ± 4,7 vs. 84,0 ± 3,8; mioglobina 71,0 ± 10, vs. 70,2 ± 9 y 72,8 ± 11 vs. 75,0 ± 10; prolactina 70,4 ± 9 vs. 68,1 ± 9 y 72,2 ± 10 vs. 73,4 ± 8,2; y α1-microglobulina 22,9 ± 10 vs. 21,6 ± 10 y 26,5 ± 12 vs. 28,8 ± 11, respectivamente.
ConclusiónEl incremento del diámetro interno de las fibras capilares no ha significado una mayor eficacia en el volumen convectivo ni en la capacidad depurativa.
On-line hemodiafiltration (OL-HDF) with a high volume of replacement combines diffusive with convective treatment, allows a greater clearance of solutes of medium and high molecular weight and improves intradialysis hemodynamic tolerance.1,2 The ESHOL3 study demonstrated that post-dilution OL-HDF reduces mortality from any cause with respect to hemodialysis (HD) in prevalent patients on HD. The inclusion of the main randomized clinical trials in a pooling project with more than 2700 patients4 and several meta-analysis5,6 has confirmed the reduction in overall and cardiovascular mortality. In a post hoc analysis, the 3 clinical trials that had mortality as the main variable3,7,8 observed an association between convective volume and survival. Taking into consideration these results, it has been recommended to achieve a replacement volume greater than 21L/session.9
The main factors limiting the achievement of high convective volumes are blood flow (Qb), time and dialyzer. The pharmaceutical industry has improved the dialyzers optimizing the pore size to obtain greater volumes of substitution and greater purification.10,11 However, the question of the effect of inner diameter of the capillary fibers of these dialyzers is contradictory. In the year 2000, Ronco et al.,12 in an in vitro and in vivo study in HD, showed that the reduction of the inner diameter was associated with an increase in proximal filtration and a distal backfiltration, which improved the removal of large molecules, through a greater internal convective volume. They recommended reducing the inside diameter from 200μm (standard in those years) to a lower one, provided that an ultrapure dialysis fluid was available. However, with the progressive advance of OL-HDF, the pharmaceutical industry offers again capillary fibers with a higher inner diameter, probably to reduce the pressure of blood entering the dialyzer, since, in some monitors, it conditions the transmembrane pressure. To clarify this issue, the present study was performed to determine the effect of increasing the inner diameter of the capillary fibers on convective volume and depurative capacity.
MethodsStudy performed in one single center in stable patients on OL-HDF. We included 16 patients (12 men and 4 women) with a mean age of 64.1±13 years (range 42–91 years) who were in the HD program for an average of 64±67 months (interval 5–251 months). The etiology of chronic renal failure was chronic glomerulonephritis (n=4) (10.8%), diabetic nephropathies (n=3) (8.1%), polycystic kidney disease (n=2) (5.4%), vascular nephropathies (n=2) (5.4%), urological causes (n=3) (8.1%), systemic disease (n=1) (2.7%) and unknown etiology (n=1) (2.7%). All patients were dialyzed through arteriovenous fistula except one, which was dialyzed through a prosthetic fistula. The anticoagulation used was heparin of low molecular weight (tinzaparin) in 50%, heparin sodium in 25% of the patients and the remaining 25% were dialyzed without heparin.
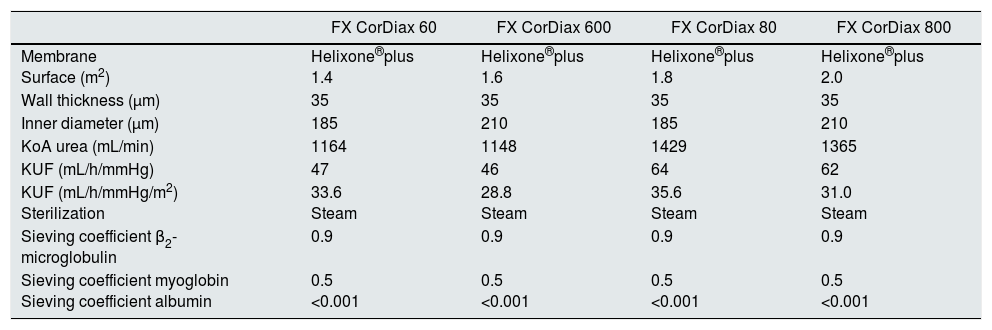
Each patient was analyzed in 4 sessions, always mid-week, in which the inner diameter of the capillary fibers of the dialyzer was changed: 185μm (FX60 Cordiax and FX80 Cordiax) vs. 210μm (FX600 Cordiax and FX800 Cordiax). The characteristics of the dialyzers are shown in Table 1. The dialysis parameters were kept constant in each of the studied sessions: helixone plus membrane; dialysis time, 293±17min (240–300min); dialysate flow (Qd) 400mL/min and monitor 5008 Cordiax, post-dilution OL-HDF with auto-substitution system. The order of the sessions was randomized. The dialysis parameters collected in each session were: programmed time, real duration, dialyzer, Qb, Qd, caliber of the needles, Kt automatically measured by ionic dialysance, recirculation index measured by the temperature module, arterial pressure, venous pressure, transmembrane pressure, initial and final hematocrit, ultrafiltration, volume of blood processed and substitution volume.
Characteristics of the dialyzers.
| FX CorDiax 60 | FX CorDiax 600 | FX CorDiax 80 | FX CorDiax 800 | |
|---|---|---|---|---|
| Membrane Surface (m2) | Helixone®plus 1.4 | Helixone®plus 1.6 | Helixone®plus 1.8 | Helixone®plus 2.0 |
| Wall thickness (μm) | 35 | 35 | 35 | 35 |
| Inner diameter (μm) | 185 | 210 | 185 | 210 |
| KoA urea (mL/min) | 1164 | 1148 | 1429 | 1365 |
| KUF (mL/h/mmHg) | 47 | 46 | 64 | 62 |
| KUF (mL/h/mmHg/m2) Sterilization | 33.6 Steam | 28.8 Steam | 35.6 Steam | 31.0 Steam |
| Sieving coefficient β2-microglobulin | 0.9 | 0.9 | 0.9 | 0.9 |
| Sieving coefficient myoglobin Sieving coefficient albumin | 0.5 <0.001 | 0.5 <0.001 | 0.5 <0.001 | 0.5 <0.001 |
KUF: ultrafiltration coefficient; KoA: mass transfer coefficient.
Laboratory measurements included the concentrations of urea (60Da), creatinine (113Da), β2-microglobulin (11,800Da), myoglobin (17,200Da), prolactin (23,000Da), α1-microglobulin (33,000Da), α1-acid glycoprotein (41,000Da) and albumin (66,000Da) in serum at the beginning and at the end of each session to calculate the percentage reduction of these solutes. The final concentration of β2-microglobulin, myoglobin, prolactin, α1-microglobulin, α1-glycoprotein and albumin were corrected for the degree of hemoconcentration and the volume of distribution (approximately extracellular volume) according to Bergström and Wehle.13 Urea, creatinine and albumin concentrations were measured by molecular absorption spectrometry on the ADVIA 2400 analyzer (Chemistry System from Siemens Healthineers, Tarrytown, USA). β2-microglobulin and α1-acid glycoprotein were measured by immunonephelometry with the Dimension Vista analyzer (Siemens Healthineers) and α1-microglobulin by immunonephelometry with the BNII analyzer (Siemens Healthineers). Myoglobin concentrations were measured by “sandwich” enzyme immunoassays with the Dimension EXL analyzer (Siemens Healthineers). Prolactin concentrations were measured by “sandwich” enzyme immunoassay with the ADVIA Centaur analyzer (Siemens Healthineers).
In all cases, specific reagents were used. The reference values in our laboratory are 10–50mg/dL for urea, 0.3–1.3mg/dL for creatinine, 0.1–2.3mg/L for β2-microglobulin, 0–100ng/mL for myoglobin, 2.8–15ng/mL for prolactin, 5–25mg/L for α1-microglobulin, 0.38–1.18g/L for α1-acid glycoprotein and 34–48g/L for albumin.
Likewise, a proportional part of the dialysis fluid was collected to quantify the loss of solutes and also of albumin. Urea, creatinine and prolactin were measured as in serum. However, since the concentrations of β2-microglobulin and albumin were very low, it was necessary to analyze these values with the same technology, but with the methods of determination used in urine samples to increase the analytical sensitivity. The β2-microglobulin was measured with more sensitive method: 0.004625mg/L.
The results are expressed as the arithmetic mean±standard deviation. For the analysis of the statistical significance of quantitative parameters, the Student t test for paired data and ANOVA for repeated data were used. A p<0.05 was considered statistically significant.
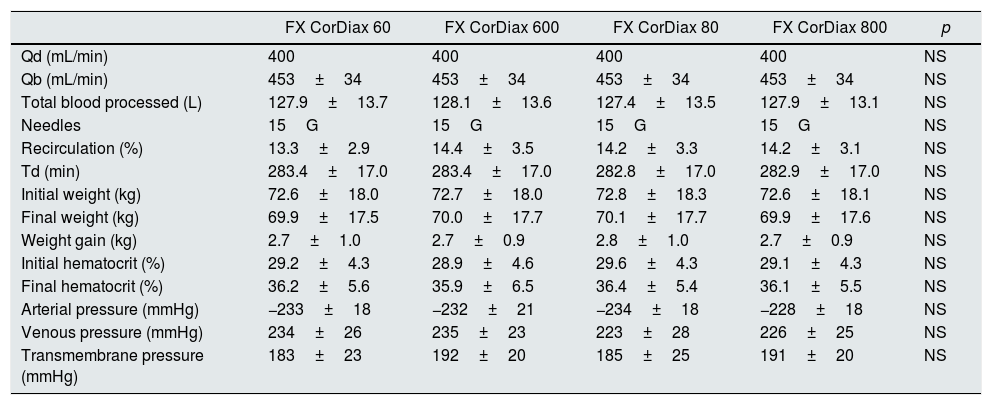
ResultsAll dialysis sessions were performed without notable clinical incidents. Clothing of the lines or dialyzed was not observed. There were no differences in dialysis parameters: Qb, total blood processed according to the monitor, Qd, real duration of sessions, initial weight, final weight, weight gain, measurements by the dialysis monitor of the initial and final hematocrit, size of the needles, recirculation of the vascular access, arterial pressure, venous pressure or transmembrane pressure (Table 2).
Comparison of dialysis parameters during the 4 different sessions.
| FX CorDiax 60 | FX CorDiax 600 | FX CorDiax 80 | FX CorDiax 800 | p | |
|---|---|---|---|---|---|
| Qd (mL/min) | 400 | 400 | 400 | 400 | NS |
| Qb (mL/min) | 453±34 | 453±34 | 453±34 | 453±34 | NS |
| Total blood processed (L) | 127.9±13.7 | 128.1±13.6 | 127.4±13.5 | 127.9±13.1 | NS |
| Needles | 15G | 15G | 15G | 15G | NS |
| Recirculation (%) | 13.3±2.9 | 14.4±3.5 | 14.2±3.3 | 14.2±3.1 | NS |
| Td (min) | 283.4±17.0 | 283.4±17.0 | 282.8±17.0 | 282.9±17.0 | NS |
| Initial weight (kg) | 72.6±18.0 | 72.7±18.0 | 72.8±18.3 | 72.6±18.1 | NS |
| Final weight (kg) | 69.9±17.5 | 70.0±17.7 | 70.1±17.7 | 69.9±17.6 | NS |
| Weight gain (kg) | 2.7±1.0 | 2.7±0.9 | 2.8±1.0 | 2.7±0.9 | NS |
| Initial hematocrit (%) | 29.2±4.3 | 28.9±4.6 | 29.6±4.3 | 29.1±4.3 | NS |
| Final hematocrit (%) | 36.2±5.6 | 35.9±6.5 | 36.4±5.4 | 36.1±5.5 | NS |
| Arterial pressure (mmHg) | −233±18 | −232±21 | −234±18 | −228±18 | NS |
| Venous pressure (mmHg) | 234±26 | 235±23 | 223±28 | 226±25 | NS |
| Transmembrane pressure (mmHg) | 183±23 | 192±20 | 185±25 | 191±20 | NS |
NS: no significant; Qb: blood flow; Qd: dialysate flow; Td: duration of dialysis.
The increase in inner diameter in the 2 series of comparisons did not show an increase in the replacement volume (29.61±33.5 with FX60 Cordiax vs. 29.07±33.8L/session with FX600 Cordiax and 30.99±4.5 with FX80 Cordiax vs. 30.83±4.1L/session with FX800 Cordiax); and, as expected, the total convective volume was not changed (Fig. 1).
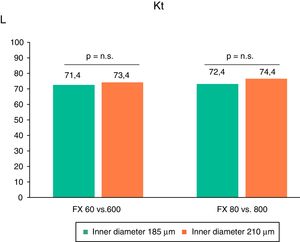
The difference in the inner diameter of the dialysis fibers did not produce significant effect in the dialysis dose, expressed as Kt (71.4±5.7 with FX60 Cordiax vs. 73.4±5.9L with FX600 Cordiax and 72.4±70 with FX80 Cordiax vs. 74.4±7.7L with FX800 Cordiax) (Fig. 2), nor as the percentage of urea reduction (Table 3).
Percent of solute reduction during hemodialysis.
| FX CorDiax 60 | FX CorDiax 600 | p | FX CorDiax 80 | FX CorDiax 800 | p | |
|---|---|---|---|---|---|---|
| Urea (60Da) | 83.7±4.5 | 84.1±3.4 | NS | 82.7±4.1 | 83.6±3.8 | NS |
| Creatinine (113Da) | 78.2±5.6 | 77.8±4.6 | NS | 77.1±5.4 | 78.1±4.9 | NS |
| β2-microglobulin (11.818Da) | 82.2±4.3 | 82.9±4.2 | NS | 82.9±4.7 | 84.0±3.8 | NS |
| Myoglobin (17,200Da) | 71.0±10.0 | 70.2±9.3 | NS | 72.8±11.0 | 75.0±10.0 | NS |
| Prolactin (23,000Da) | 70.4±9.3 | 68.1±8.6 | NS | 72.3±10.0 | 73.4±8.2 | NS |
| α1-microglobulin (33,000Da) | 22.9±10.0 | 21.6±9.8 | NS | 26.5±12.0 | 28.8±11.0 | NS |
| α1-acid glicoprotein (41,000Da) | 15.6±8.2 | 11.5±5.8 | NS | 17.3±9.3 | 15.4±7.1 | NS |
| Albumin (66,000Da) | 9.2±6.7 | 8.9±4.9 | NS | 10.1±5.8 | 7.8±5.2 | NS |
| Loss of albumin in dialysate (g) | 2.7±1.8 | 1.6±0.9 | NS | 3.2±1.9 | 3.0±1.9 | NS |
The percent reduction of the rest of the solutes (creatinine, β2-microglobulin, myoglobin, prolactin, α1-microglobulin and α1-acid glycoprotein) is shown in Table 3. Neither, the inner diameter of the fibers nor the 2 types of dialyzers being compared produces a significant difference in the percent reduction of solutes. No significant differences were observed in the albumin eliminated through the dialysate in any of the 2 comparison series: 2.7±1.8g for FX60 Cordiax vs. 1.6±0.9g with FX600 Cordiax and 3.2±1.9g with FX80 Cordiax vs. 3.0±1.9g with FX800 Cordiax.
DiscussionThe present study shows that, in post-dilution OL-HDF, the comparison of 2 series of dialyzers with inner capillary fiber diameters of 185 and 210μm showed no differences on convective volume and depurative efficacy. After reviewing the literature, this study represents the first study in OL-HDF in which the inner diameter is compared without changing the rest of the dialysis parameters. The convective volume reached, which varied between 29 and 31L/session, was adequate, although no statistically significant differences were observed in any of the 2 standards compared. In terms of efficacy, no significant differences were observed in the reduction of solutes of small and high molecular weight.
The effectiveness of HD treatment is measured in terms of survival, morbidity and quality of life obtained during both the dialysis session and the interdialysis period. OL-HDF combines diffusive transport and allows a considerable increase in convective transport,14 with a greater clearance of medium and high molecular weight toxins.15,16 OL-HDF is a safe technique that improves intradialysis hemodynamic tolerance1,3 contributing, among others, to the correction of anemia, the chronic inflammation, amyloidosis, hyperparathyroidism, oxidative stress and the lipid profile,17–19 and increases survival3–6 and quality of life.4,20
During the last few years, new dialyzers have been developed with greater surface area, better geometric arrangement of capillary fibers, variation of wall thickness, larger pore size, in order to achieve greater removal of both small and medium-large molecules. The ideal hemodialyzer should achieve the following characteristics: high clearance of small molecules; high sieving coefficient for β2-microglobulin and myoglobin; low sieving coefficient for albumin; low transmembrane pressures that do not limit the infusion flow; great power to trap endotoxins and a good price.21
The convective capacity of the dialyzers follows the Hagen–Poiseuille law, Δp = Qb×8ηl/πr4, the drop of pressure inside the dialyzer fiber is directly proportional to the Qb, the lengthl and the blood viscosity and inversely proportional to the inner diameter. A pressure drop inside the fiber will increase the pressure gradient between the blood compartment and the dialysis compartment, leading to greater convective transport. Taking into account that, a minimum reduction in the diameter of the capillary fiber has a great impact on the pressure drop inside the capillary fiber that will increase the pressure gradient between the blood and the dialysis fluid along the entire length of the fiber, with improvement of both diffusion and convection. In terms of efficacy, while the increase in diffusion hardly implies variation in the clearance of small molecules, a greater convective transport causes a greater clearance of f high molecular weight molecules.
In a previous study22 it was shown that the increase in Qb is probably the best method to reach the highest convective volume. For every 50mL/min of Qb increase, the convective volume increases more than half a liter per hour. The Qb increases the removal capacity of small molecules and favors that of β2-microglobulin and myoglobin. In another study23 the effect of increasing the dialyzer surface was evaluated, and it was concluded that the increase in the dialyzer surface caused a small increase in the convective volume without evidencing an improvement in the removal capacity, especially if the ultrafiltration coefficient was higher at 45mL/h/mmHg. In the present study, we did not observe significant variations of convective volume in any of the 2-series compared. Unlike the previous study, in our study, in addition to an increase in the inner diameter of the capillary fiber from 185μm to 210μm, there was a small increase of 0.2m2 in the surface of the dialyzer (1.4m2 for FX CorDiax 60 vs. 1.6m2 for FX CorDiax 600 and 1.8m2 for FX CorDiax 80 vs. 2.0m2 for FX CorDiax 800). Therefore, the non-variation observed in the convective volume may be the result of the opposite variations of simultaneous increase in area and diameter that can compensate for each other.
The publications on the effects of the variation of the inner diameter of the capillary fibers in relation to the convective volume and the removal capacity of the dialyzers are limited. Dellanna et al.24 tested in 10 high-flow HD patients 3 types of polysulfone dialyzers with identical number and length of fibers, with inner diameters of 175, 200 and 250μm, surfaces of 0.55, 0.65 and 0.79m2 respectively, and sieving coefficients for β2-microglobulin 0.82, 0.79 and 0.71, respectively. With Qb 250 and Qd 500mL/min they hardly observe any variation in the clearance of small molecules such as urea or creatinine. By contrast, the dialyzer with the smallest diameter (175μm), despite having the smallest surface, showed a clearance of β2-microglobulin twice that of the dialyzer of 200μm and almost 5.6 times higher than that of 250μm. Ronco et al.,12 also in HD, compared in vitro and in vivo 2 types of high flow dialyzers with hollow fiber of polysulfone, of 0.7m2 of surface, the standard with a diameter of 200μm and another modified to an inner diameter of 175μm. With dialysis parameters of Qb 300 and Qd 500mL/min in vitro, it was observed an increase in internal filtration and backfiltration from 23.1mL/min in the fibers of 200μm diameter to 48.2mL/min in the 175μm dialyzer. The in vivo studies showed that the reduction in inner diameter produced an increase of 30% in the clearance of intermediate solutes such as vitamin B12 or inulin. Similar results were obtained by Mineshima et al.25 In an analytical-experimental study they analyzed the effects of the inner diameter of the capillary fibers on the internal filtration and the efficiency in the elimination of solutes in HD. They evaluated 5 dialyzers of the same surface (1.5m2) and inner diameters of 150, 175 and 3 sessions with 200μm varying the number and length of the capillary fibers. They observed that a decrease in the inner diameter of the capillary fibers increased internal filtration and increased the clearance of myoglobin. In this same study they show that an excessive reduction of the inner diameter may increase the risk of hemolysis and transfer of biological contaminants, so they proposed that the reduction of the inner diameter should not produce an internal pressure drop superior to 150mmHg, for the patient's own safety.25
We have not found in the literature comparative studies of the inner diameter in OL-HDF. In a study that analyzed the factors associated with the achievement a greater convective volume, Marcelli et al.26 observed a convective volume of 25.1±4.1L in 325 patients with FX60 as compared to 27.3±4.6L in 2572 patients with FX600. However, these 2.2L of difference cannot be attributed to the change in inner diameter but to the increase in Qb (352±54 vs. 361±70mL/min) and to the duration of treatment (241±11 vs. 255±19min).
We conclude that the increase of the inner diameter of the capillary fibers in OL-HDF has not produced a greater efficiency in the convective volume nor in the depurative capacity. Therefore, the inner diameter in dialyzers with high ultrafiltration coefficient does not seem to be a limiting factor in convective volume, as it is the blood flow or dialysis time.
Conflicts of interestThe authors declare to have no conflicts of interest.
We would like to express our gratitude to all the patients who have participated, as well as to all the staff of the Dialysis Section of the Hospital Clínic of Barcelona for their collaboration and enthusiasm in this study.
Please cite this article as: Maduell F, Ojeda R, Belmar L, Munguía P, Sango C, Martinez-Díaz AI, et al. Valoración del diámetro interno del dializador en hemodiafiltración on-line. Nefrologia. 2018;38:34–40.