The skin conditions which can occur in chronic kidney disease patients are: xerosis, pruritus, calciphylaxis, pseudoporphyria, uraemic frost and acquired perforating skin disorders; the latter are characterised by presenting transepidermal elimination of material from the dermis, and consist of Kyrle disease, reactive perforating collagenosis and elastosis perforans serpiginosa.1
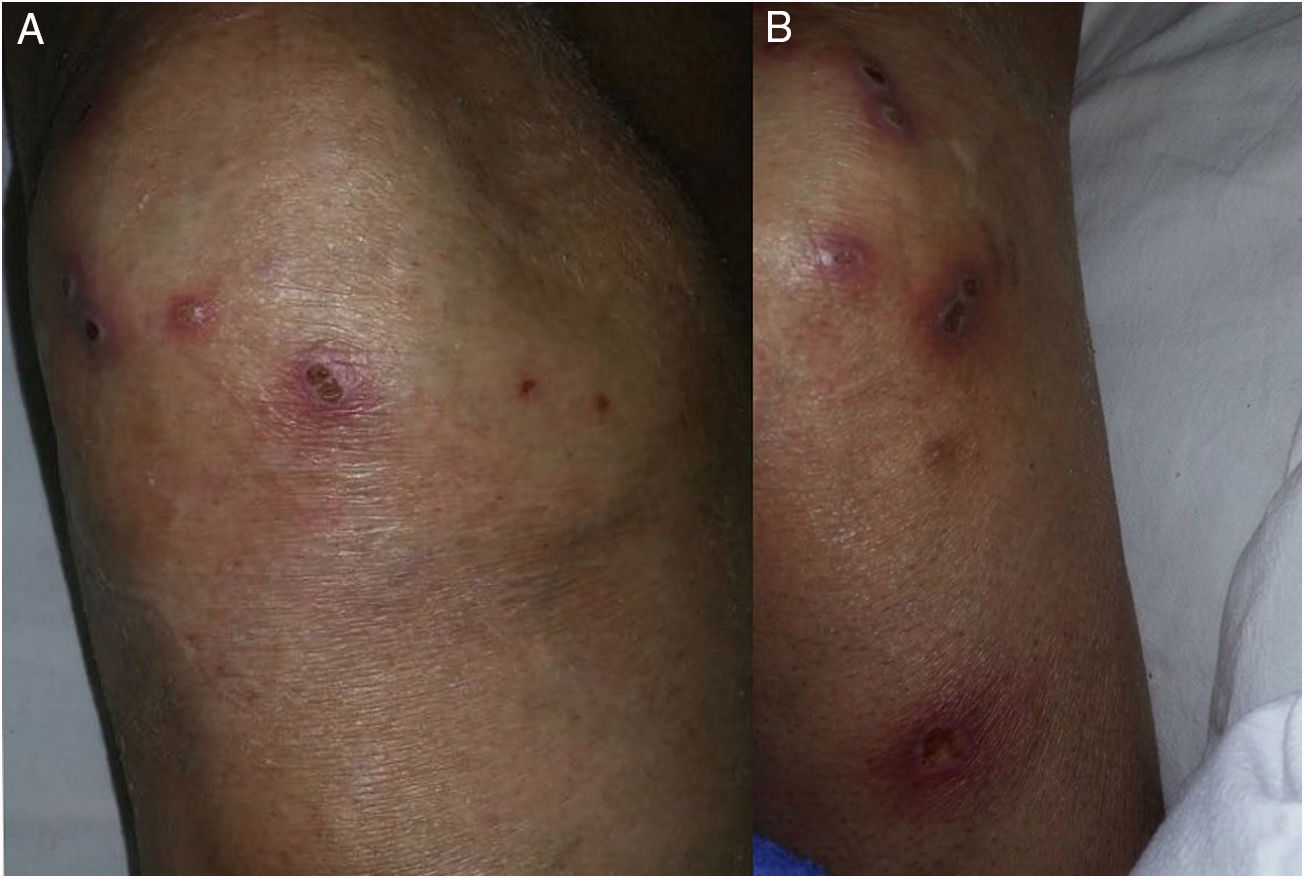
We present the case of a 78-year-old male with a history of type 2 diabetes mellitus, systemic hypertension, long-term hypothyroidism and chronic kidney disease on replacement therapy with peritoneal dialysis for the past five years, with adequate control. The patient was hospitalised due to healthcare-associated pneumonia. We were consulted due to a disseminated, bilateral and symmetrical dermatosis which affected the lateral side of both arms and the anterior side of the knees, made up of multiple plaques measuring 0.5–1cm in diameter which were circular, erythematous, had a crateriform appearance with a haematic scab on their surface, were itchy and had first appeared six weeks previously (Fig. 1).
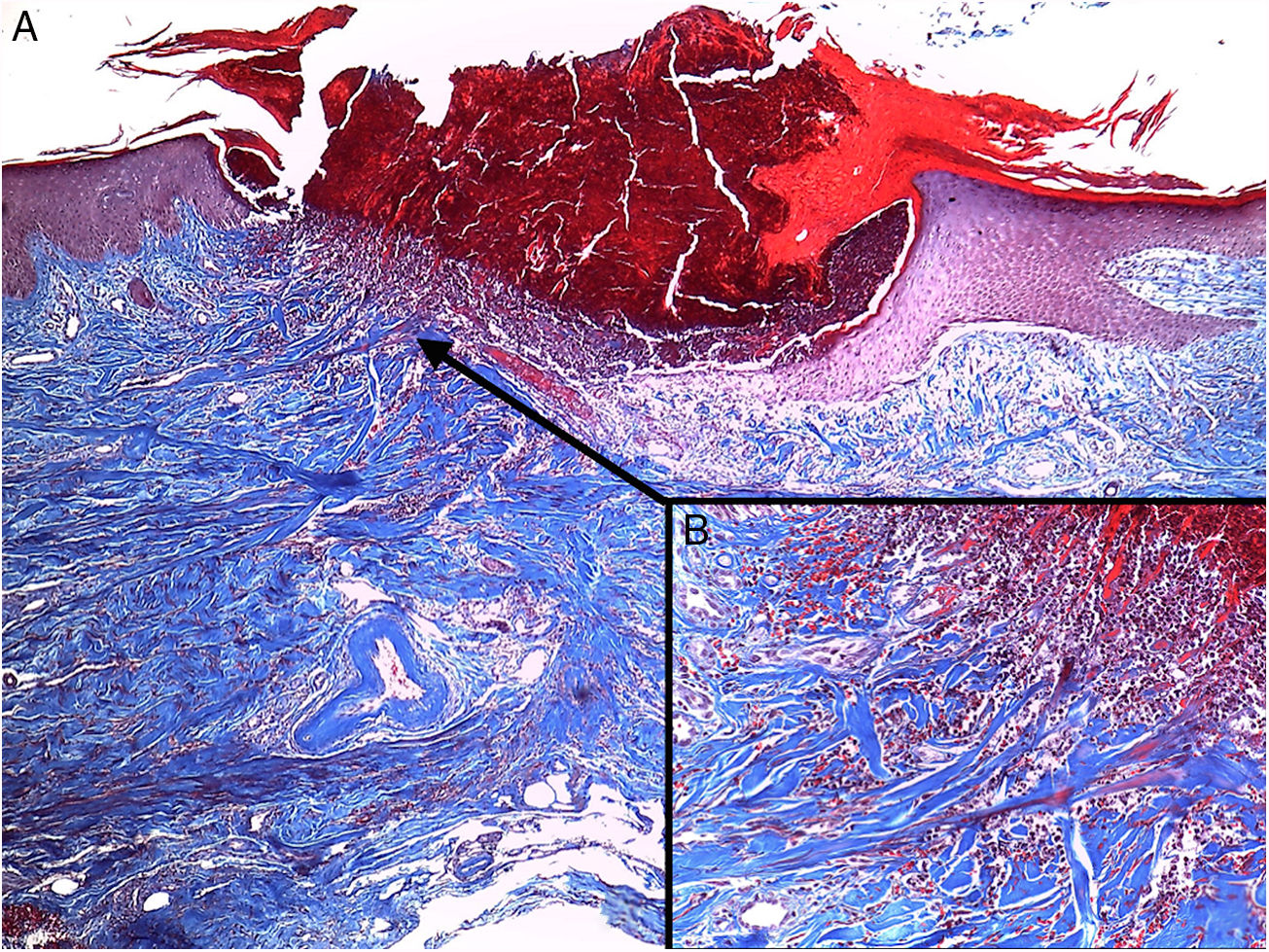
A biopsy of one of the lesions was performed which showed in the haematoxylin and eosin stain: epidermis with moderate acanthosis which surrounded a plug made up of the scab, keratinous detritus and inflammatory cells; in the base of this plug, flattened epidermis with introduction of collagen fibres running vertically from the dermis could be seen; with Masson's trichrome stain, the presence of transepidermal elimination of collagen fibres was confirmed (Fig. 2). With these findings, the diagnosis of acquired reactive perforating collagenosis (ARPC) was made. The patient was treated with fluocinolone acetonide cream 0.01% every 12h plus levocetirizine tablets 2.5mg/day, with an adequate response in treatment weeks, an interval during which his symptoms of pneumonia resolved and he was discharged. The patient remained under follow-up by our department.
ARPC is an entity commonly associated with patients with diabetes mellitus and chronic kidney disease on replacement therapy; however, it can also be observed in Hodgkin's lymphoma, scabies, atopic dermatitis, tuberculosis, systemic lupus erythematosus, AIDS, systemic hypertension and chronic venous insufficiency; it mainly affects patients between the third and fifth decades of life. This entity is more common than its hereditary counterpart, which presents in the paediatric population and has few reported cases in the medical literature.2
Its pathophysiology includes the presence of receptors for advanced glycation end products (RAGE), which cause the cross-linking of collagen fibres and an increase in TGF-β 3 and metalloproteinase-1, which cause changes in the metabolism of extracellular proteins and delayed epithelialisation, combined with the presence of occasional microtrauma and chronic pruritus, which perpetuate the lesions.3
The lesions generally present on the trunk and extensor areas of the limbs; they are made up of multiple plaques of various centimetres in diameter, are circular, erythematous, of crateriform appearance, with haematic scabs or keratosis on their surface, are itchy and, due to continuous trauma, are associated with the Koebner phenomenon. The histological findings show acanthosis which surrounds a plug composed of basophilic material that contains keratin, cellular detritus and inflammatory cells; below this a flattened epidermis with the presence of collagen fibres which are introduced from the dermis is observed; they are viewed with greater accuracy with the Masson's trichrome stain.4 To make the diagnosis, it is necessary for the patient to be over the age of 18, manifest characteristic features of dermatosis and for there to be evidence of transepidermal elimination of collagen.5 Calciphylaxis, another entity that can be found in this group of patients, is clinically different due to the presence of pain that precedes the appearance of livid or violet plaques, which evolve to ulceration and necrosis, and can be found in central areas (abdomen and thighs) and peripheral areas (fingers and even the penis). The biopsy reveals calcification of the arterioles and the small-medium sized arteries, fibroblastic proliferation of the intimal layer and narrowing of the lumen.6
The cornerstone of treatment is to avoid trauma; this measure leads to reduction of new lesions, which are generally self-limiting in six to eight weeks; due to the substrate of chronic pruritus, the use of antihistamines is recommended. Due to the low frequency of this disease, the use of topical and oral retinoids, topical corticosteroids, emollients and narrow-band UVB radiation have been tried in case reports with moderate response7; allopurinol has been used in a series of 12 patients at doses of 100–300mg/day, under the premise of reducing cross-linking of collagen fibres by inhibiting xanthine oxidase, with the consequent reduction in the production of free radicals and RAGE, with improvement in seven patients after four weeks and the rest with improvement in the subsequent four months.8
The importance of presenting this case lies in showing another variety of dermatosis that may occur in patients with chronic kidney disease, to alert the treating physician to its presence, and to carry out the appropriate diagnosis and treatment due to the impact that it has on the quality of life of this patient population.
Please cite this article as: Villela-Segura U, Miranda-Aguirre AI, Estrada-Aguilar L. Placas crateriformes en un paciente con enfermedad renal crónica. Un caso de colagenosis perforante reactiva adquirida. Nefrologia. 2020;40:358–360.