Nephrogenic systemic fibrosis (NSF) is a rare fibrosing disorder was first described in renally impaired patients as a scleromyxedema-like disorder in 2000 by Cowper et al.1 It is characterized by progressive diffuse fibrotic changes of the skin bilaterally and symmetrically on the extremities, and occasionally on the trunk. Ninety-five percent of NSF cases are associated with exposure to gadolinium-based contrast agents in renal dialysis patients.2 Calciphylaxis is seen generally in patients with kidney failure and presents with livedo racemosa, indurated plaques, hemorrhagic bullae, skin ulcers, and necrosis located mostly on abdomen, breasts, buttocks and extremities.3 Association of these two rare entities was published in three cases in the literature.4,5
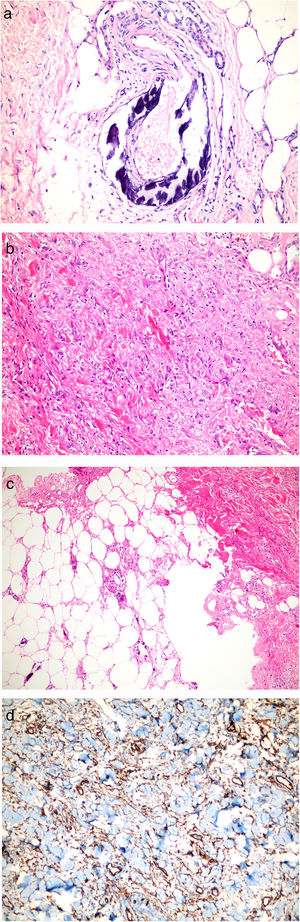
We describe the case of a 44-year-old female with bilateral painful, erythematous swellings and thickening of abdominal skin for three weeks. She had suffered from hypertension, diabetes, asthma, and hypothyroidism for 10 years and end-stage renal disease (ESRD) for 5 years. She was a hemodialysis patient for one week. She had been using doxazosin and furosemide for hypertension, subcutaneous insulin for diabetes, inhaler steroid for asthma, levothyroxine for hypothyroidism, antacid and calcium containing antiphosphate for ESRD, and subcutaneous erythropoietin for anemia for years. She was obese with mass index (BMI) 51kg/m2. She had no history of magnetic resonance imaging (MRI). On dermatologic examination, violaceous and painful plaque-like subcutaneous nodules surrounded by livedo reticularis-like patches were observed on the legs, and some of them progressed to necrotic features. She also had infraumblical sclerotic subcutaneous nodules and peau d’orange appearence (Fig. 1a–c). Histopathologic examination of crural lesions revealed dermal and subcutaneous arteriolar calcification and narrowing of the vascular lumen in subcutaneous tissue. Histopathologic examination of umblical lesion showed a dense spindle cell proliferation, focal sclerosis, thick collagen bundles in the dermis, significant fibrous thickening of the septa in subcutaneous tissue and subcutaneous arteriolar calcification. On immunohistochemical analysis CD34 and Factor 13 positivity were seen, but CD68 was negative (Fig. 2a–d). The histopathological examination and clinical findings were compatible with calciphylaxis on the extremites, and NSF and calciphylaxis on the trunk.
Histopathological examinations. (a) Lesions on legs: Dermal and subcutaneous arteriolar calcification and narrowing of the vascular lumen in subcutaneous tissue (HE stain; original magnification ×200). (b, c) Lesions on infraumblical region: Spindle cell proliferation, focal sclerosis, thick collagen bundles in dermis, fibrous thickening of the septum in subcutaneous tissue and subcutaneous arteriolar calcification (HE stain; original magnification ×40 and ×200 respectively). (d) CD34 positivity.
Laboratory tests were as follows; hemoglobin: 10.0g/dL, erythrocyte sedimentation rate (ESR): 79mm/h, creatinin 5.8mg/L, parathormone (PTH): 564pg/mL, phosphor (P): 7.3mEq/L and Calcium (Ca): 7.8mEq/L. Vasculitis was ruled out with laboratory findings (complement factors (C3, C4), rheumatoid factor (RF), antineutrophilic cytoplasmic antibodies (ANCAs), anticardiolipin antibodies, cryoglobulin, cryofibrinogen), except mild antinuclear antibody positivity (ANA: 1/160 with cytoplasmic pattern). Serum protein electrophoresis was normal. Pulmonary X-rays and echocardiography were normal. Computerized tomography (CT) and scintigraphy could not be performed because of the high BMI. She had no systemic involvement for NSF. Plain X-rays of the extremities showed vascular calcification, but doppler ultrasonography was normal.
The patient received hemodialysis treatment with a low calcium dialysate and discontinue a calcium-containing antiphosphate medication. For wound management wet dressing and topical antibiotics were used and morphine-like medications were used for analgesia. Since hypocalcemia was a possibility, sevelamer was not appropriate for the patient. Cinacalcet and sodium thiosulfate were not availible. Hyperbaric oxygen therapy was contraindicated due to asthma.
NSF and calciphylaxis are rare diseases typically seen in chronic renal failure.3 In literature 95% of NSF cases were associated with exposure to gadolinium-based contrast agents.2 In our case there was no history of MRI prior to skin lesions, but she had been using erythropoietin (EPO) for some years. There were several cases in literature of NSF without gadolinium contrast exposure.6 However it's mentioned that EPO may be associated with NSF.7 The typical clinical feature of NSF is diffuse fibrotic skin changes, but Deng et al. documented a case of NSF localized on one antecubital region because of infusion of EPO.8 The lesions of our case were seen in infraumblical region with localized sclerotic subcutaneous nodules and peau d’orange appearance without systemic involvement, but this area was not correlated with the insulin or EPO exposure sites. Risk factors for the disease are female gender, diabetes mellitus, obesity, malnutrition, using of warfarin, calcium-containing antiphosphate medication and Vitamin D.3 The risk factors for our case are obesity, female gender, diabetes mellitus and calcium-containing antiphosphate medication. Halasz et al. mentioned recently that the diagnosis of calciphylaxis may be done by radiologic techniques such as direct radiography, mammography or CT prior to receiving histopathological results.9 Radiography of the extremities in our case showed linear vascular calcification.
Coexistence of these two rare entities- NSF and calciphylaxis- was published in three cases in the literature.4,5 Edsall et al. documented a report of two cases who were clinically typical of NSF with evident vascular calcification on skin biopsy like calciphylaxis, but had no clinical features of calciphylaxis. They mentioned NSF may be a predisposing factor for calciphylaxis in early stages, or calcification may play a role in the pathophysiology of NSF. They also thought fibrosis and calcification in kidney failure may be the result of increased activity of transforming growth factor-b/Smad signaling cascades.4 Lewis et al. reported a case of NSF and calciphylaxis with pseudoxanthoma elasticum-like changes in the same localization.5 In our case the infraumblical-localized lesion of our patient revealed the diagnosis of NSF with vascular calcification-like calciphylaxis. By describing this case we want to emphasize that, although microscopic calcification has been reported in the skin biopsies of NSF, coexistence of the calciphylaxis and nephrogenic systemic fibrosis with different localizations may be seen. To the best of our knowledge this is the first case of coexistence of the calciphylaxis and nephrogenic systemic fibrosis with different localizations in a hemodialysis patient. This situation may be explained with consociate etiological origin.
Conflict of interestNone.