We present a case of a 57-year old female who complained of progressive weight loss, general weakness, dysphagia and mild bilateral leg swelling. She had a history of asthma, arterial hypertension, hypothyrosis due to Hashimoto thyroiditis and axonal sensorimotor polyneuropathy of unknown cause. She had no family history of renal disease. General and systemic examination was unremarkable except minimal peripheral leg edema and mildly atrophic lower limb musculature. She had no nail or patella dysplasia.
Blood test results: creatinine 110μmol/L; CKD-EPI glomerular filtration rate 48ml/min/1.73m2, cystatin C 2.8mg/dL, mildly elevated gamma glutamyl transferase and alkaline phosphatase, hypoalbuminemia 32g/L, positive ANA H+ (1:160).
Urine test results: microhematuria and proteinuria 4g per day.
Diagnostic procedures revealed mild to moderate pulmonary hypertension, mild pericardial effusion, hepatosplenomegaly, bilateral minimal pleural effusion and ascites (exudate with negative cytology results).
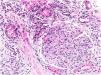
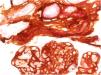
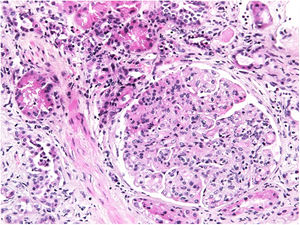
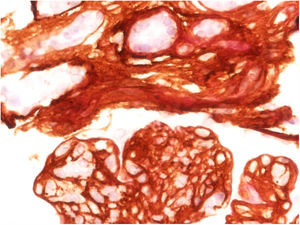
Renal biopsy revealed a diffuse endoproliferative (mesangioproliferative pattern) exudative sclerosing glomerulonephritis with collagen III deposition within mesangium and capillary walls, accompanied with diffuse chronic fibrosing mononuclear tubulo-interstitial nephritis. Immunocomplex glomerulonephritises were excluded (Figs. 1 and 2).
Measurement of N-terminal peptide of type III procollagen (PIIIP) in serum (19.2ng/mL) and urine (53.6ng/mL) was performed (RIA-gnost® PIIIP kit, Cisbio Bioassays).
Our patient was discharged with furosemide and angiotensin-converting-enzyme (ACE) inhibitor. On follow-up her renal function was stable. In a few months she died at home. Unfortunately the autopsy was not performed and the cause of death remained unknown.
Collagen type III nephropathy (Col3NP) is a rare glomerular disease with characteristic accumulation of abnormal collagen type III in glomerular mesangium and subendothelial space and increase in serum PIIIP levels.1 The etiopathogenesis remains unclear, but ethnic and/or genetic factors may play a role.2 Some authors suggested autosomal recessive inheritance pattern, whereas in our case the occurrence of disease was sporadic.3
The most common clinical presentation is proteinuria, which is in the nephrotic range in more than 50% of the patients, with or without associated nephrotic syndrome. Hematuria is microscopic. Arterial hypertension is present in approximately 60% of the patients. Renal function is usually normal or slightly reduced at presentation, but in 50% there is progression to end-stage renal disease (ESRD).3 Our patient presented with nephrotic range proteinuria and microscopic hematuria but without arterial hypertension. She had chronic kidney disease (CKD) stage 3. Our histology findings from renal biopsy were consistent with data from literature presenting patients with Col3NP.2,3
Type III collagen is a structural protein of extracellular matrix and is present in tissues showing elastic properties. In kidney it is normally present only in the interstitium and blood vessels, but not in the glomerulus.4 Although the pathogenesis of this disease is still unknown, two explanations have been proposed. One is the mesangial production of abnormal collagen, another is mesangial accumulation of type III collagen derived from other organs.5
The disease is mainly limited to kidneys, but there are a few isolated reports of extra-renal involvement with Col3NP leading to a hypothesis that renal lesion may be a part of a systemic disease with abnormal metabolism of type III collagen.5 Abnormal collagen III fibers have been found in liver, spleen and kidneys and in some other organs (myocardium, pancreas, thyroid gland, alveoli).5 According to clinical examination and all pathological findings we believed that our patient had some kind of systemic disease. She had multiple organ damage which we could not explained otherwise. She developed hepatosplenomegaly with ascites. Without biopsy of the liver etiology of liver disease in our patient remained unknown, however we excluded other common causes (viral hepatitides, alcohol consumption, cirrhosis, hemochromatosis, cancer, intoxication, etc.). Since there is data from literature that collagen III deposition was found in spleen and liver in some patients with confirmed Col3NP, we assumed that was the cause in our patient as well. Furthermore, unexplained polyneuropathy of our patient may as well be caused by abnormal collagen III deposition in nervous system, since common neurological diseases were excluded. Additionally, there was also unexplained pulmonary hypertension.
Unfortunately, Col3NP is a progressive disease and no specific therapy is available. Supportive measures include control of arterial hypertension, diuretics to relieve edema and renal replacement therapy if needed.4 Steroids, cyclosporine, cyclophosphamide and low-density lipoprotein apheresis had been tried with no benefit.6 The progression of the disease is assumed to depend on the extent of deposition and the amount of tubulointerstitial fibrosis and atrophy.7 In an isolated renal pathology the worst end point is progression to ESRD, whereas in a systemic involvement there is progression to multiorgan failure and death. We can speculate, that in a systemic type of disease with multiple organs affected, the progression is even faster. We assumed that was the case in our patient – she died a few months after the diagnosis.