Dear Editor,
Membranous glomerulonephritis (MGN) is a common cause of nephrotic syndrome in adults which is characterized by formation of subepithelial immune complex deposits with resultant changes to glomerular basement membrane (GBM), most notably GBM spike formation. The onset of this disorder is slow and the clinical course is often benign. Anti-neutrophil cytoplasmic antibody (ANCA)-associated glomerulonephritis is the most frequent cause of rapidly progressive glomerulonephritis and is usually classified as a pauci-immune type characterized by glomerular necrosis and crescent formation. MGN complicated by ANCA-associated glomerulonephritis is an unusual concurrence and only rare cases have been reported previously;1-6 however, none of them was presented in Chinese population and most of the cases reported were related to some backgrounds. Here we first report an elderly Chinese male patient with MGN and myeloperoxidase (MPO)-positive ANCA-associated glomerulonephritis without any detectable backgrounds.
A 64-year-old man presented with arthralgia, shortness of breath, nausea, oliguria, and edema without previous history of disease. Laboratory examinations showed the following results: serum creatinine concentration 350.8μmol/L, serum albumin level 21.3g/L, serum total cholesterol 7.1mmol/L and a 24-hr protein excretion of 5.4g/d. The urinalysis showed 3+ urine protein, 2+ urine blood and RBC casts. MPO-ANCA was detected in serum screening test by indirect immunofluorescence and the serum concentration of MPO-ANCA was subsequently determined by enzyme-linked immunosorbent assay (ELISA) to be 145U/mL (reference range, 0-10U/mL). Other immunological tests showed the decrease of serum complement 3 concentration to 0.571g/L and other autoantibodies including anti-nuclear antibodies (ANAs), anti-Sm antibody, anti-dsDNA antibody, anti-cyclic citrullinated peptide (CCP) antibody, anti-proteinase-3 (PR3)-ANCA and anti-glomerular basement membrane (GBM) antibody were negative. There was no evidence of systemic lupus erythematosus (SLE), infection, malignancy, or drugs. Percutaneous renal biopsy was subsequently performed to determine the diagnosis.
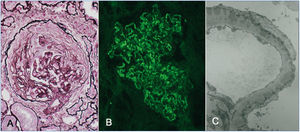
Upon light microscopy, renal biopsy revealed thickening of glomerular capillary wall and 2 out of 19 glomeruli were sclerosed. Four glomeruli showed cellular crescents, 5 showed fibrocellular crescents formation and 2 showed fibrinoid necrosis (Figure 1 A). Immunofluorescence examination displayed granular deposition of IgG and C3 along the glomerular capillary walls (Figure 1 B). Electron microscopy showed thickened glomerular basement membranes with diffuse subepithelial deposits and foot process effacement which was consistent with the stage II of MGN (Figure 1 C). Therefore renal histology and laboratory examinations supported the diagnosis of MGN and MPO-positive ANCA-associated glomerulonephritis.
The patient was treated initially with pulse methylprednisolone 500mg/d for 3 days followed by prednisone (40mg/d) and antihypertensives, anticoagulant were also administrated. Because of no sign of improvement shown a week later, steroid pulse therapy was performed again followed by prednisone (40mg/d) and intravenous cyclophosphamide 0.4g once a week. On review after 1 month of treatment, proteinuria and renal function had improved significantly with urine protein down to 1.9g/d and creatinine down to 182.7μmol/L. MPO-ANCA testing was repeated and showed seronegative. The patient remained stable at a follow-up of 1 year.
As we know, crescent formation and fibrinoid necrosis are rarely encountered in membranous glomerulonephritis. Although MGN associated with ANCA-associated glomerulonephritis has been described previously in white adults and Japanese population, most of the cases reported were related to some rheumatic diseases such as SLE,7 anti-GBM disease,8,9 malignancy such as esophageal carcinoma,10 or drugs.11 The coexistent MGN and ANCA-associated glomerulonephritis without the above backgrounds is a rare occurrence with less case reported. Here we first show the Chinese patient with MGN complicated by ANCA-associated glomerulonephritis without the evidence of underlying backgrounds. Tse WY reported 10 patients with MGN and ANCA-associated glomerulonephritis including 9 males and 1 female and the median age was 63.5 years.2 Cases described by Nasr SH involved 8 males and 6 females and the median age was 58.7 years.5 Added with the case of 64-year-old man we present here, MGN associated with ANCA-associated glomerulonephritis may mainly occur in the elderly patients and the incidence in male seemed to be higher than in female. The clinical course is more aggressive than MGN alone and is characterized by nephrotic syndrome, hematuria and acute renal failure with or without systemic vasculitis involving extrarenal organs. Renal pathology involves both the membranous changes and crescent formation with fibrinoid necrosis. As for the prognosis, Tse WY and Nasr SH reported a similar outcome that 50% of patients reaching endpoints of ESRD or death whether or not treated with immunosuppressive agents;5 however, our patient showed well response to immunosuppressive treatment.
The mechanism of MGN associated with ANCA-associated glomerulonephritis is unknown. Some case reports have noted an association with the presence of anti-GBM antibodies that may play a role in the pathogenesis because the development of glomerular crescents requires disruption of the GBM integrity sufficient to allow the efflux of cells and macromolecules into Bowman’s space.8,9 The autoantibodies in lupus nephritis type III and V or type IV and V may also contribute to the combination of crescentic and membranous glomerulonephritis that is not uncommon in patients with SLE.7 But in case of MGN associated with ANCA-associated glomerulonephritis without anti-GBM nephritis, SLE and other related diseases, the mechanism is difficult to elucidate because of the fact that the pathogenesis of MGN and ANCA-associated glomerulonephritis is distinct from each other. Whether ANCA is associated with the pathogenesis or not remains unclear and whether MPO-ANCA-associated glomerulonephritis is superimposed on idiopathic membranous nephropathy (MN) or MPO-ANCA-associated glomerulonephritis induce a secondary MGN is still unknown. Suwabe and Watanabe examined IgG subclass deposition and found that the cases with MGN and ANCA-associated glomerulonephritis showed both IgG1 and IgG4 deposited on the glomerular capillary walls, which suggested secondary MGN;4,6 however, no disease or drug was found to induce secondary MGN. The fact only a few MPO-positive cells in the glomeruli and MPO stains on the glomerular capillary walls near the MPO-positive cells may suggest that the patient had MPO-ANCA-associated glomerulonephritis superimposed on idiopathic MN.6 But Nasr SH was inclined to regard the co-existence of MGN and ANCA-associated glomerulonephritis as a coincidence.5 Further research is required to clarify the pathogenesis of the rare occurrence.
In summary, MGN with ANCA-associated glomerulonephritis is a rare dual glomerulopathy seen in patients with heavy proteinuria and acute renal failure. In case of nephrotic syndrome with seropositive MPO-ANCA and progressive renal failure even though without evidence of SLE or anti-GBM nephritis, we should consider the coexistence of MGN and ANCA-associated glomerulonephritis. Although prognosis is variable, remission was observed after administration of steroids and cyclophosphamide in this dual glomerulopathy.
This study was supported by grants from Science and Technology Development Plan Project of Jilin Province (No. 20100738) and from Fundamental Scientific Research Fund of Jilin University, China.
Conflict of interest
The author declares that there is no conflict of interest associated with this manuscript.
Figure 1. Renal biopsy findings in membranous glomerulonephritis associated with anti-neutrophil cytoplasmic antibody-associated glomerulonephritis