Introducción: La diálisis peritoneal (DP) es una técnica establecida de tratamiento renal sustitutivo que gracias a los avances tecnológicos y clínicos ha mejorado sus tasas de supervivencia en los últimos años. Objetivos: Evaluar la supervivencia del paciente y la técnica en DP a lo largo de 30 años y según las décadas para consolidar su utilidad sanitaria. Métodos: Estudio retrospectivo de cohorte de todos los pacientes del programa de DP del Hospital Universitario La Paz (Madrid) desde 1980 a 2010. Variables demográficas y clínicas fueron recolectadas de los registros clínicos. Resultados: Se incluyeron 667 pacientes, 54,4 % varones, con edad media de 51,47 años y una mediana de seguimiento de 23,1 meses. Se observó un aumento progresivo de pacientes incidentes, especialmente en DP automatizada (DPA). La supervivencia del paciente a 5 años fue de 54 %, con una mediana de 64,66 meses, con un aumento significativo en la última década (p = 0,000). La edad, la comorbilidad, el sexo masculino, la DP crónica ambulatoria (DPCA) y la diabetes fueron predictores de la supervivencia del paciente. La supervivencia de la técnica a los 5 años fue del 64,2 % y la mediana de 82 meses. El éxito de la técnica fue mayor en jóvenes, en DPA y con menor comorbilidad. Conclusiones: Durante 30 años se observó un aumento de los pacientes incidentes. La edad, la comorbilidad y la diabetes siguen siendo los principales determinantes de la supervivencia.
Introduction: Peritoneal dialysis (PD) is an established renal replacement therapy technique which thanks to the technological and clinical advances has improved its survival rates in recent years. Objectives: The aim of this study was to evaluate patient and technique survival in PD over 30 years, according to the different decades in order to consolidate its usefulness in healthcare. Method: Retrospective cohort study including all patients in the PD programme of the Hospital Universitario La Paz (Madrid), from 1980 to 2010. Demographic and clinical variables were collected from medical records. Results: A total of 667 patients were included, 54.4% male, with a mean age of 51.47 years and a median follow-up period of 23.1 months. There was a progressive increase in PD incident patients, especially in automated PD (APD). Patient survival at 5 years was 54%, with a median of 64.66 months, increasing significantly in the last decade (P=.000). Age, comorbidity, male sex, chronic ambulatory PD (CAPD) and diabetes were predictors of patient survival. Technique survival at 5 years was 64.2% with a median of 82 months. The success of the technique was greater in younger patients on APD and with lower comorbidity. Conclusions: Over 30 years, we found an increase in incident patients. Age, comorbidity and diabetes still continue to be the main determining factors for survival.
INTRODUCTION
Dialysis is a dynamic process subject to the influences of clinical advances and technological innovations. Peritoneal dialysis (PD) is a technique that has been widely used in the treatment of chronic kidney disease (CKD) since the beginning of 1980s, with over 100,000 patients worldwide. In Spain, according to the latest data of the 2011 Renal Disease Registry, the prevalence of CKD was 1078 per million population (pmp), with 5.27% of these patients on PD.1
PD is a valid option for renal replacement therapy, which has shown similar survival rates to haemodialysis (HD), but with major differences in certain groups, particularly in terms of age and the presence of diabetes (DM).2-6 Survival rates in PD are variable, because there are multiple reports of retrospective cohorts with rates ranging from 50% to 70% at five years,7-10 although the longest experience reported to date of 25 years in Turkey9 shows rates of 68.9%, with a significant increase in patient survival in the last period, a phenomenon that has been reported in many series. This improvement in survival experienced by PD in recent years is potentially related to changes in normal practice and the introduction of improvements, enabling better results to be achieved.
The main objective of this study was to assess the survival of the technique and patients over the 30 years in which our PD unit has been operating, comparing the results from the different decades and assessing the main factors that influence mortality in patients.
PATIENTS AND METHODS
All patients who started PD in our unit and were able to be trained for the technique from January 1980 to December 2010 were analysed retrospectively. We evaluated a total of 667 patients and those under 18 years of age were excluded. The cohort was divided into three periods, corresponding to each successive decade (1980-1990, 1991-2000 and 2001-10), and comparative studies were carried out between the three groups with regard to initial comorbidity, patient survival and technique survival.
Data were collected from medical records: age at start of PD, sex, cause of CKD, DM, comorbidity according to the Charlson index,11,12 origin before the start of the technique (transplant, HD, CKD consultation or acute renal failure [ARF]), mean duration of the technique, PD stage (if patients had more than one period on PD after a failed renal transplantation or recovery of renal function), status at the end of follow-up (death, transplantation, transfer to HD or continuation of the technique) and cause of death, if relevant.
Failure of the technique was defined as transfer to HD and the determining factors were categorised as ultrafiltration failure, mechanical problems, patient decision, peritonitis, catheter-related problems and insufficient dialysis.
Statistical analysis
Statistical analysis was performed using the SPSS software version 13.0 (SPSS Inc., Chicago, Illinois, USA). All data are expressed using measures of central tendency and dispersion (means ± standard deviation) for quantitative variables and frequencies for qualitative variables; for statistical inference, data comparison was carried out using the χ2 test and Student’s t test in accordance with the types of variables. We used the Kaplan-Meier method for technique and patient survival and the log-rank test to compare the curves. For multivariate analyses, we used the Cox proportional hazards model. A P value below .05 was considered significant. In patient survival analysis, patients who were lost to follow-up, who received a kidney transplant, recovered renal function or were transferred to HD were censored. In the technique survival analysis, patients who were lost to follow-up, those who recovered renal function, died or received a kidney transplant were censored.
RESULTS
Patient characteristics
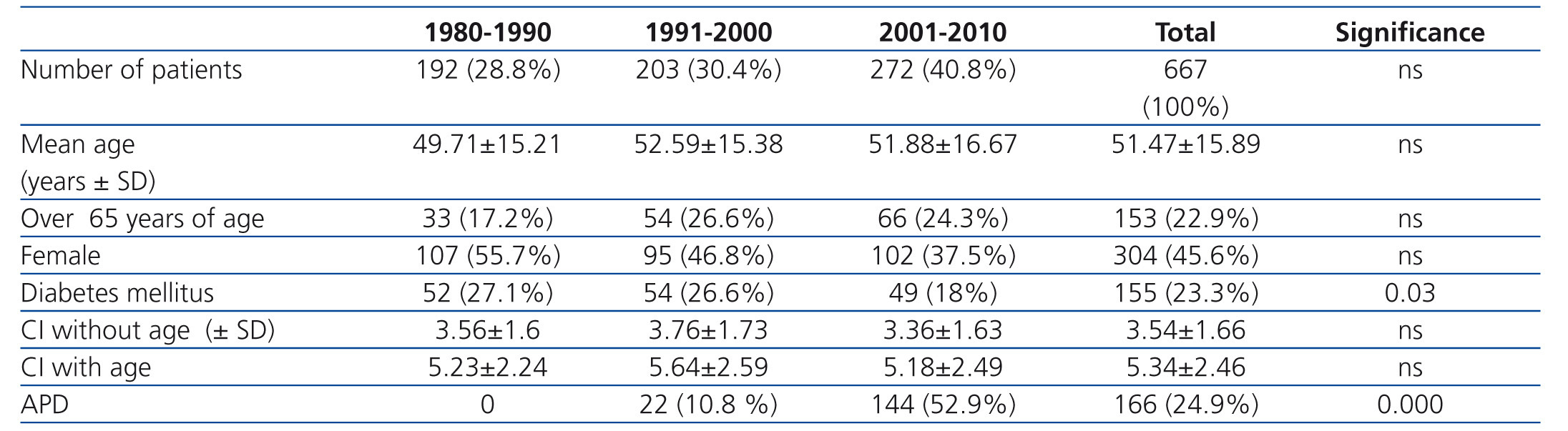
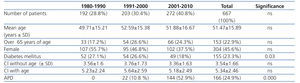
The general profile of the patients is illustrated in Table 1. 54.4% were male, the mean age at the start of PD was 51.47±15.89 years and the follow-up mean was 30.6±28 months (median 23.1 months).
The causes of CKD were in 131 (19.6%) cases, tubulointerstitial nephritis, in 131 (19.6%) cases, diabetic nephropathy, in 114 (17.1%) cases, chronic glomerulonephritis, in 73 (10.9%) cases, unknown, in 66 (9.9%) cases, autosomal dominant polycystic kidney and liver disease, in 61 (9.1%) cases, hypertensive nephropathy, in 59 (8.8%) cases, systemic diseases, in 15 (2.2%) cases, vascular and in 7 (1%) cases, hereditary kidney diseases.
The reasons for starting PD were in 498 (74.7%) patients, due to CKD progression, in 57 (8.5%), due to loss of renal graft, in 67 (10%), due to transfer from HD and in 45 (6.7%) patients, non-recovery from an episode of ARF.
Solutions used in peritoneal dialysis
A total of 146 patients (21.59%) used icodextrin and from 2004, we used the biocompatible PD solutions in 138 (21%) patients. We did not find any differences in the survival between patients who were treated with or without icodextrin (P=.5) and those treated or not with biocompatible PD solutions.
Comparative data according to decades
The data are displayed in Table 1. We observed a progressive increase in the number of incident patients in the three periods. No differences were observed in age, sex, Charlson index, follow-up time or cause of CKD on comparing the three periods, with the most common causes of CKD being tubulointerstitial nephritis (19.6%) and DM (19.6%). In the last period, we observed a higher incidence of diabetic patients (P=.03), patients on automated PD (APD) (P=.000) and patients whose origin was a kidney transplant (P=.000).
Reasons for discontinuing peritoneal dialysis
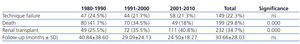
At the end of the study, 199 (29.8%) patients died, 232 (34.8%) received a kidney transplant, 149 (22.3%) were transferred to HD, 38 (5.7%) were transferred to another centre, 14 (2.1%) recovered renal function and 35 (5.2%) continued on PD.
We observed a significant increase in PD discontinuation due to renal transplantation (P=.000) over the three decades, with a decrease in the mortality rate (P=.0001), without observing differences in the transfer to HD. The patients who received a transplant were significantly younger, had a lower Charlson index score and lower prevalence of DM (Table 2).
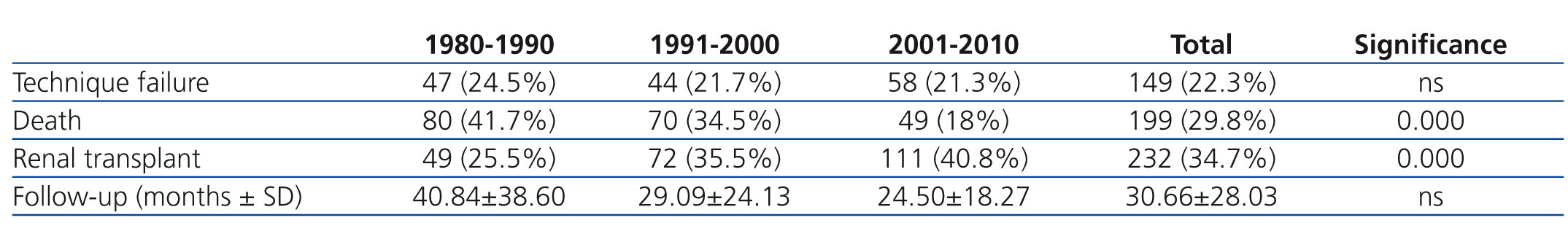
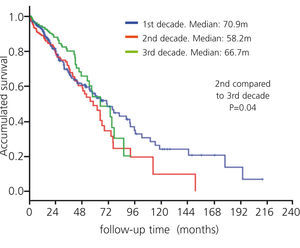
Analysis of patient survival
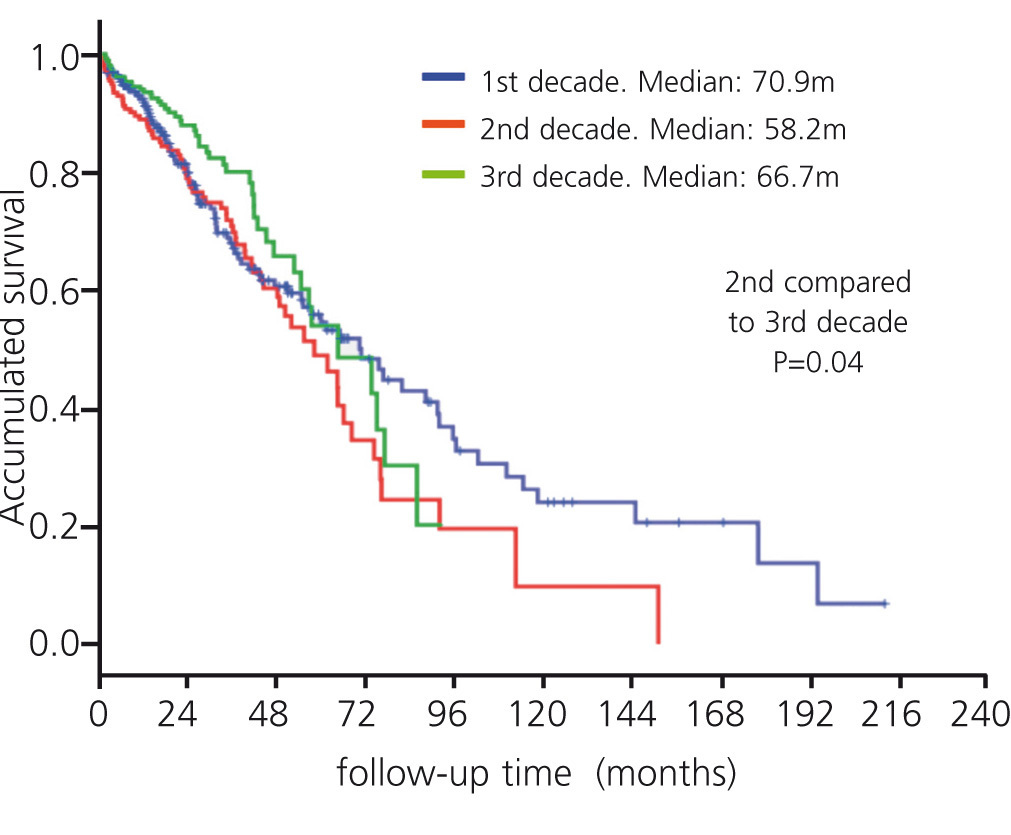
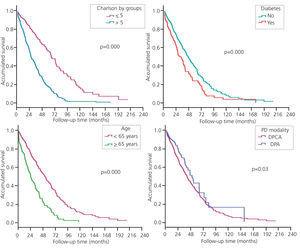
The main cause of death was cardiovascular, followed by infection, without significant differences being observed over the three periods. The median survival was 64.66 months. The overall survival of the patients was 92, 73, 54, 36 and 19.6% at 1, 3, 5, 7 and 10 years. A significant decrease in mortality was observed between the second and third decades (P=.04) (Figure 1). The main risk factors that influenced patient survival were age greater than 65 years (P=.000), male sex (P=.037), a Charlson index score >5 (P=.000), DM (P=.000), type 2 DM in particular (P=.000), and chronic ambulatory PD (CAPD) (P=.03).
In the Cox multivariate model, the Charlson index, age and HD origin were related to patient survival.
Analysis of technique survival
The survival of the technique was 93.4, 78.5, 64.2, 47.1 and 39.6% at 1, 3, 5, 7 and 10 years. Median survival was 82 months. The reasons for transfer to HD were: membrane failure in 38 (25.5%) patients, peritonitis in 33 (22.14%), wall problems in 16 (10.73%), patient decision in 44 (29.5%), insufficient dialysis in 2 (1.34%), catheter malfunction in 2 (1.34%) and various causes in 14 (9.39%). The main risk factors for technique survival were age >65 years (P=.000), Charlson index scores >5 (P=.000), DM (P=.000), type 2 DM (P=.000) and CAPD modality (P=.034). No differences were observed over the three decades (Figure 2). In the Cox multivariate model, the Charlson index, age, DM, type 2 DM and ADP are independently related to the survival of the technique.
DISCUSSION
In the present study, we assessed patient and technique survival in our PD unit after 30 years of experience, comparing the results in the different decades.
According to the 2011 Spanish Renal Disease Registry, the prevalence of CKD in Spain is 1078 pmp and over the years, we have observed an increase in the use of PD as an initial treatment option, although it continues to be the least employed treatment modality (5.27%).1
The demographic characteristics of the patients in this study are similar to the characteristics of those starting dialysis in Spain. The proportion of diabetic patients in our cohort was 23.3% and the main causes of kidney disease were DM and tubulointerstitial nephritis, which is similar to data reported in other cohorts in Spain, such as that of the registry of Andalusia.13,14
Overall patient survival at five years in our cohort was 54%, which is similar to rates reported in other studies,7-10 with a significant decrease in mortality between the second and third decades. The improvement in the prognosis of PD patients has been evident in recent decades, as is demonstrated by data in the Renal Registry of Renal Diseases and also in the 2009 ERA-EDTA European population registries.15 In Spain, Quiros-Ganga reported the experience of PD in Andalusia after 12 years, comparing the results before and after the introduction of biocompatible PD solutions, and improvements in survival could be observed in the last period.13
In line with other studies, age and DM were independent predictors of patient survival.10,16,17 Improved survival was observed in APD, similar to the results shown by Mujais et al. in the United States;10 this may be due to variables not taken into account in the study that define the profile of patients starting on APD, such as increased compliance with treatment and possibly higher ultrafiltration, which has an influence on survival.
The comorbidity of patients in our study was measured by the Charlson index, and in PD it has proven to be a good predictor and more useful than age, DM or cardiovascular disease separately.12 In this study, comorbidity was associated with reduced survival of the technique and the patient.
Other factors not analysed in this study were shown to influence survival in PD patients, such as serum albumin, serum creatinine, high blood pressure, residual renal function, the peritonitis rate, the creatinine dialysate/plasma ratio and Kt/v urea,7,9 but most studies agree that PD patient survival is influenced to a much greater extent by the conditions at the beginning of the technique (age, comorbidity and DM) and that these other factors play a marginal role after statistical adjustments are made, including multiple variables.6
In our unit, the survival rate for the technique at five years was 64.2%. In general, the rates reported in other series are variable, with rates at five years from 20% to 68.2%, the latter being described by Nakamoto et al.18 in the Japanese population in 2006, which is similar to that described in our series. It is important to highlight that the psychosocial factors that primarily include the voluntary decision to withdraw the technique, usually due to the inability to care for oneself, are the main cause of failure (29.5%) in our series and constitute a factor on which technological advances and improved dialysis practices have less influence.
Failure rates for the technique show much variability between the different centres, as has been demonstrated in multiple studies.10,19-21 Huismans et al. analysed several Dutch registration centres and found that this variation is related to the absolute number and proportion of PD patients, with low survival being displayed for the technique in centres with less than 20 patients.
Data from our centre represent the longest accumulated experience (30 years) reported to date in the literature. We have seen an increased incidence of PD patients over the three decades, with a significant decrease in mortality between the second and third decade. It is possible that over time certain factors, such as better patient selection, the centre’s own experience in the technique (collective learning curve), knowledge of the most appropriate dialysis doses, the use of biocompatible PD solutions, the increased use of APD and continuity of medical and nursing care have contributed to better outcomes in our centre.
In terms of its limitations, the design is a single-centre, retrospective study, and as such, we cannot rule out the effect of the centre on survival. Moreover, other factors related to the quality of dialysis, the characteristics of the peritoneal membrane and the peritonitis rate, among others, that may influence patient or technique survival, were not taken into account in this study, although they were analysed in other specific studies.
We conclude that in our PD unit, after 30 years of experience, we have seen an increase in the incidence of patients, greater use of APD and an improvement in survival. The maturity of the technique is demonstrated with these indicators, but each patient continues to require high quality care.
Acknowledgements
The authors wish to express their gratitude to the Instituto Reina Sofía de Investigación Nefrológica (IRSIN) and REDinREN (RETICS 06/0016 of ISC III).
Conflicts of interest
The authors declare that they have no conflicts of interest related to the contents of this article.
Table 1. Baseline characteristics of peritoneal dialysis patients according to decade
Table 2. Reasons for discontinuing the technique
Figure 1. Survival curves by decade (1980-2010)
Figure 2. Risk factors that influence patient survival. Univariate analysis by: Charlson Index (A), diabetes mellitus (B), age (C) and peritoneal dialysis modality (D).