Introducción: Los eventos cardiovasculares (CV) son la primera causa de mortalidad en pacientes con enfermedad renal crónica (ERC). El objetivo de nuestro estudio fue determinar los factores predictores de eventos CV y mortalidad en pacientes con ERC (estadios 1-4). Material y métodos: Realizamos un estudio prospectivo con 218 pacientes (62 % varones), con una mediana de edad de 69 años (rango intercuartílico 56-78). Basalmente se recogieron variables demográficas, antecedentes CV y parámetros analíticos. Se recogieron los eventos CV y la mortalidad (variable final). Resultados: Durante el seguimiento (38 [37-39] meses), 50 pacientes tuvieron un evento: 37 pacientes (17 %) tuvieron un evento CV y 13 (6 %) fallecieron de causa no CV. Se asoció con la variable final ser varón, ser fumador activo, diabetes mellitus, antecedentes CV, presión arterial diastólica baja, menor filtrado glomerular, un índice albúmina/creatinina en orina superior a 1000 mg/g, niveles de troponina T elevados, niveles de péptido natriurético cerebral elevados, niveles de proteína C reactiva elevados y niveles de hemoglobina bajos. En el análisis multivariante, mantuvieron su poder predictivo independiente para el evento final ser varón, diabetes mellitus, antecedentes CV y menor filtrado glomerular. Conclusión: El sexo varón, la diabetes mellitus, tener menor filtrado glomerular y tener antecedentes de evento CV son predictores independientes de tener evento CV y de mortalidad en pacientes con ERC. No hemos podido demostrar la superioridad de los marcadores emergentes de riesgo CV frente a los clásicos.
Introduction: Cardiovascular events (CV) are the major cause of mortality in chronic kidney disease patients (CKD). The aim of the present study was to determine the independent predictors of CV and mortality in CKD patients (stages 1-4). Methods: A prospective study was conducted with 218 patients (62% male), with a median age of 69 years (interquartile range 56-78). Basally, demographic variables, CV risk factors and biochemical values were collected. During follow-up, new CV events and deaths were collected (final variable). Results: During follow-up (38 [37-39] months), 50 patients suffered a final event: 37 patients (17%) had a CV and 13 (6%) died due to a non-CV death. Having a final event was associated to male sex, smoker, diabetes mellitus, history of CV event, low diastolic blood pressure values, low glomerular filtration, urine albumin/creatinine higher than 1000 mg/g, higher troponin T levels, higher BNP levels, higher CRP levels and lower haemoglobin levels. Multivariate analysis, showed that only male sex, diabetes mellitus, previous CV event and lower glomerular filtration independently predicted having the final event. Conclusion: Male sex, diabetes mellitus, previous CV event and lower glomerular filtration independently predicted having a CV event or death in CKD patients. We could not demonstrate the superiority of emerging CV risk markers compared to the classic ones.
INTRODUCTION
Patients with chronic kidney disease (CKD) are at an increased risk for cardiovascular events and mortality and this increases with severity of the kidney disease.1 This situation is due to different circumstances such as inflammation, uraemia, malnutrition or coexistence of other cardiovascular risk factors such as hypertension, dyslipidaemia, peripheral vascular disease or a history of associated cardiovascular disease.2,3. In fact, international nephrology (National Kidney Foundation) and cardiology (American Heart Association) societies recommend considering CKD as an independent risk factor.4,5 In addition, the cardiovascular risk factors mentioned above are also CKD progression factors.6
There is currently growing interest in identifying markers that will allow us to distinguish between CKD patients who are at increased cardiovascular risk.
Different cardiac biomarkers, such as troponin or natriuretic peptide, have been proposed for identifying those CKD patients with an increased cardiovascular risk.7 It is known that an asymptomatic increase in these markers leads to a poor cardiovascular and overall prognosis in CKD patients. This is due to silent myocardial damage and not to deterioration in renal function itself.8
Other emerging markers have appeared in recent years that have also been associated with increased cardiovascular risk. These include uric acid, cytokines, interleukins or adiponectins.9,10 These emerging markers have demonstrated their predictive value in several studies. However, they are still not included in routine clinical practice. For this reason, the classic factors continue to form the foundation for stratifying cardiovascular risk in CKD patients.11-13 In addition, different intrinsic factors of kidney disease itself are associated with a greater number of events. These include proteinuria, calcium-phosphorus metabolism alterations, anaemia or water-electrolyte disorders.14,15
The focus of this study is to determine which risk factors are associated with suffering a cardiovascular event and death in the CKD population. These include some emerging factors in order to corroborate their utility in stratifying cardiovascular risk in these patients.
MATERIAL AND METHOD
We performed a prospective study over 6 months with 218 consecutive patients with stable CKD (stages I-IV) in outpatient nephrology follow-up, of which 135 (62%) were men and the median age was 69 (56-78) years. The data were collected and evaluated by four observers. Demographic variables (age and sex), personal medical history (cardiovascular risk factors [presence of diabetes, dyslipidaemia, smoking, blood pressure levels and monitoring, abdominal circumference] and cardiovascular history prior to the study) were collected at baseline and laboratory studies were ordered for cardiac markers (troponin T, brain natriuretic peptide [BNP]), kidney disease (creatinine, albuminuria), inflammation-nutritional markers (ferritin, fibrinogen, C-reactive protein [CRP], albumin), calcium-phosphorus metabolism markers (parathyroid hormone [PTH], calcium, phosphorus, vitamin D) as well as other variables that were considered relevant such as insulin, homocystein and haemoglobin. None of these measurements required more blood draws or office visits on the part of the patient. Patients also provided verbal informed consent for inclusion in the study.
We define dyslipidaemia according to the ATP III guidelines (LDL greater than 160mg/dl in patients with 0-1 risk factor; greater than 130mg/dl in patients with more than 1 risk factor; greater than 100mg/dl in patients with coronary artery disease or equivalent; or those in treatment with lipid-lowering agents).16 We define hypertension according to the criteria of the seventh report of the Joint National Committee (blood pressure above 140/90mmHg or in treatment with at least one antihypertensive agent).17 We define progression according to the recently published “Consensus Document on Chronic Kidney Disease"6 as loss of more than 5ml/min/1.73m2/year of glomerular filtration rate (GFR), GFR deterioration greater than 25% or greater than 50% increase in the urine albumin/creatinine ratio.
Routine methods were used to measure creatinine, albumin, haemoglobin, uric acid, fibrinogen, PTH, calcium, phosphorus and vitamin D. Ultrasensitive CRP was measured using turbidimetric immunoassay in the HITACHI automatic analyzer (Sigma Chemical Co., St. Louis, MO, USA). Albuminuria was measured as the albumin/creatinine ratio with an immunonephelometric method. Cardiac troponin T and BNP were measured using a third-generation electrochemiluminescence (ECLIA) immunoassay (Roche Diagnostics, Basel, Switzerland). Based on the estimated GFR by CKD-EPI, we divided the patients into stages according to the K/DOQI Guideline classification.18
The first cardiovascular events (fatal and non-fatal) were recorded during follow-up (median 38 [37-39] months):
- Heart failure.
- Arrhythmia.
- Peripheral artery disease (diagnosed as stenosis of the main arteries or arteries of the lower extremities confirmed by arteriogram; or the need for amputation).
- Stroke.
- Coronary event.
In addition to deaths by other causes, we defined a combined variable for all endpoint events (composed of cardiovascular events and death due to any cause).
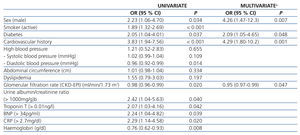
A univariate analysis was done in order to corroborate the factors associated with an endpoint event. Afterwards, those factors that were independent predictors were analyzed using multivariate analysis.
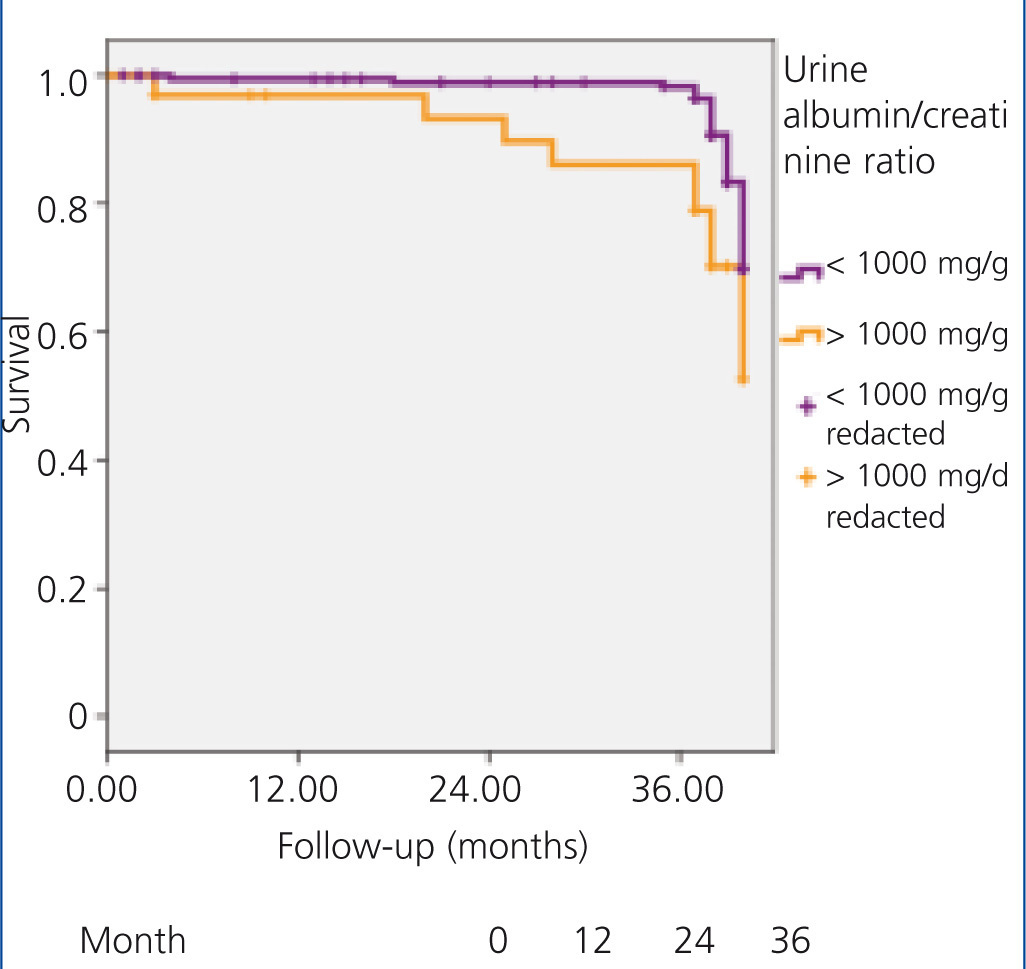
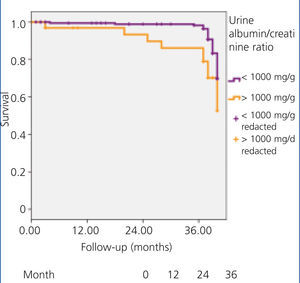
The variables are expressed as the mean (standard deviation) if they follow a normal distribution (according the Kolmogorov-Smirnov test). When the variables do not follow a normal distribution, they are expressed as the median (interquartile range). Student’s t test or the χ2 test was used for variables with a normal distribution, otherwise the Mann-Whitney U test was used. Logistical regression analysis was performed to analyze what variables were predictive of endpoint events. A survival analysis was performed using the Kaplan-Meier curves in order to confirm the link between albuminuria (urine albumin/creatinine ratio above or below 1000mg/g) and the events. In addition, linear regression was used to calculate the progression of CKD. This cut-off point was chosen as it was sufficient data in the univariate analysis. A value of P<.05 was considered to be statistically significant. SPSS version 16® (Chicago, IL, USA) was used for the statistical analysis.
RESULTS
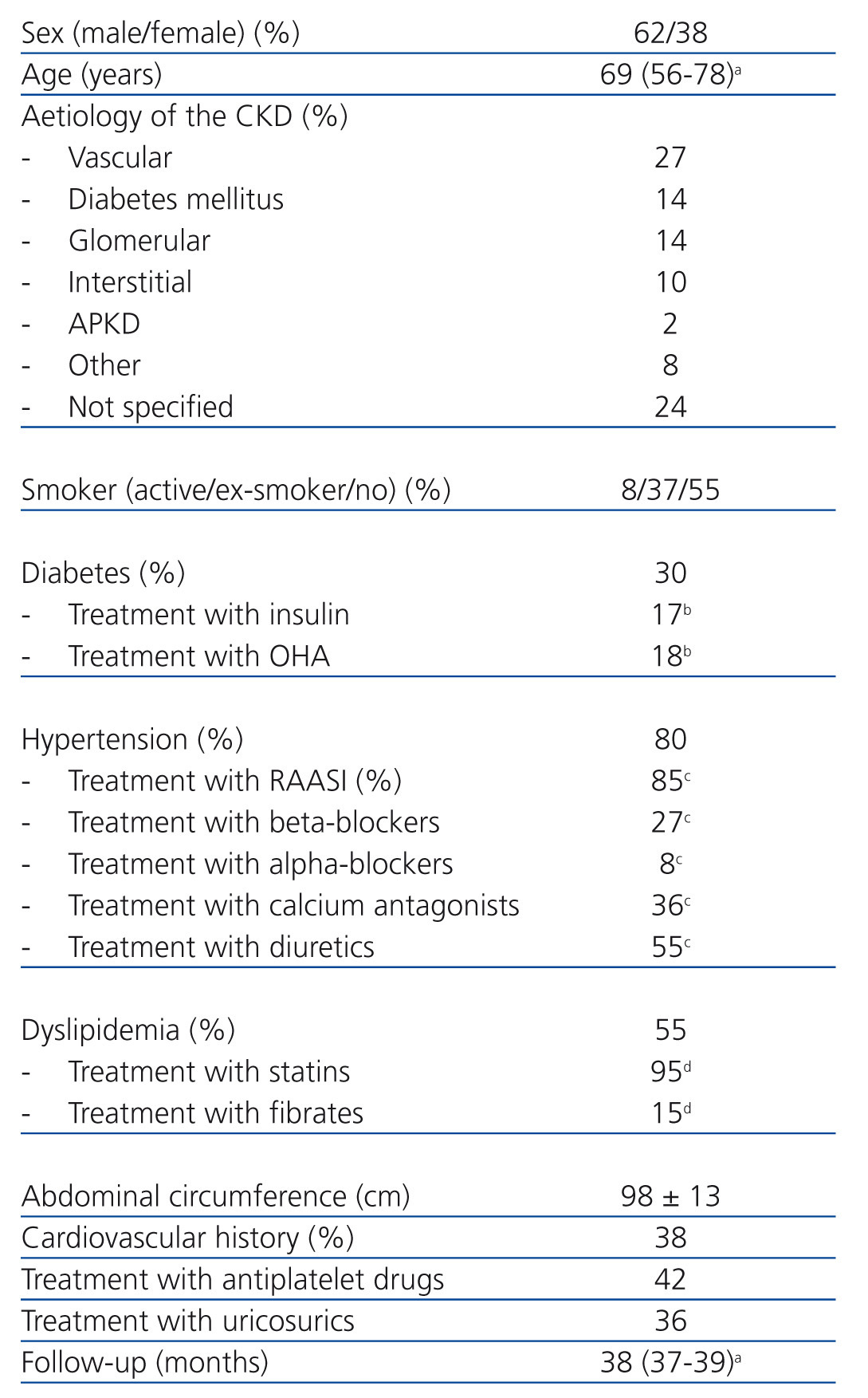
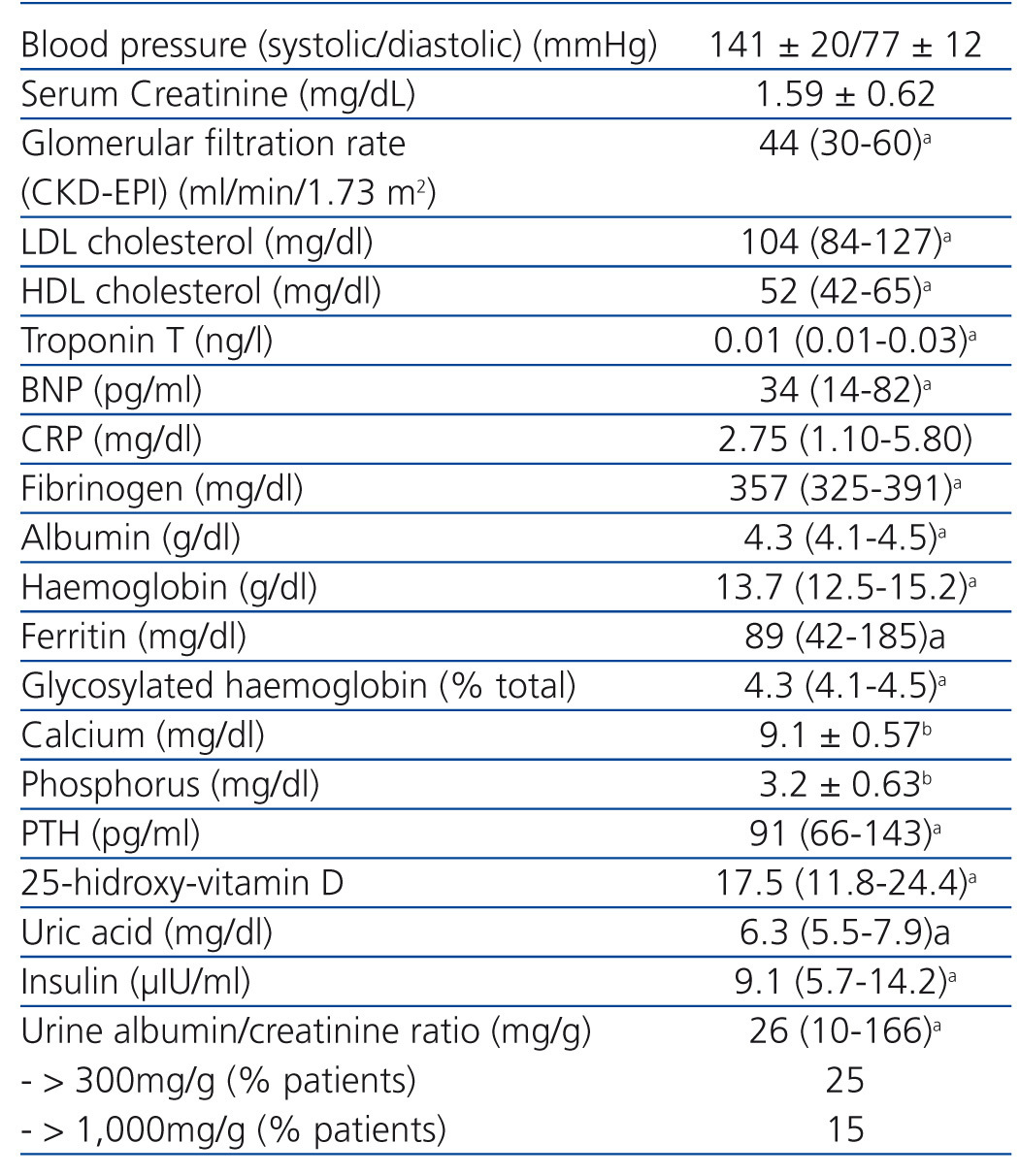
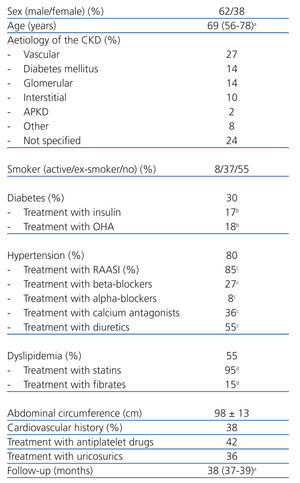
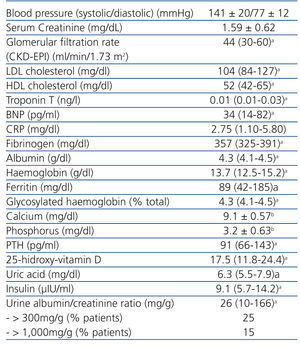
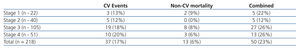
The baseline characteristics of the population (n=218) are shown in Table 1. The baseline laboratory values are shown in Table 2. Patients with CKD, stages 1 to 4, were included and distributed as follows: stage 1, 10%; stage 2, 18%; stage 3, 48%; stage 4, 23%.
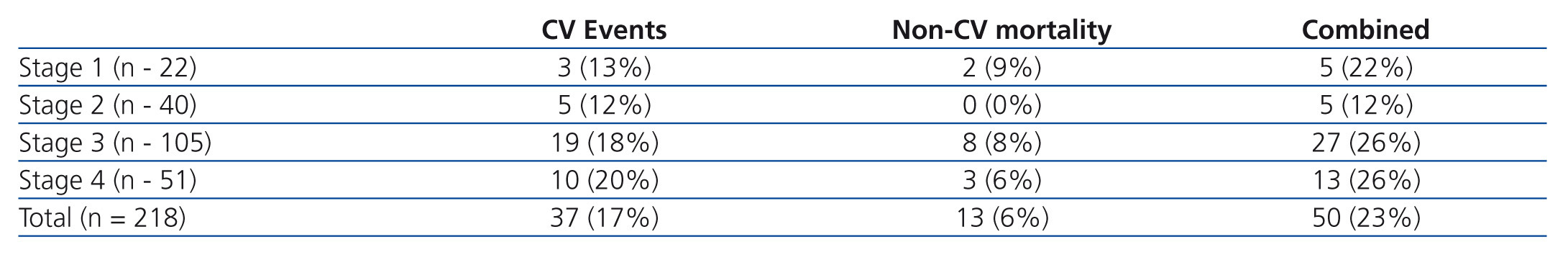
During follow-up (38 [37-39] months), 50 patients had an event: 37 patients (17%) had a cardiovascular event and 13 (6%) died due to a non-cardiovascular cause. The distribution of the events was the following: 33% coronary event, 29% died, 17% first episode of heart failure, 8% some type of arrhythmia, 8% stroke and 2% peripheral artery disease. 10% of patients (21) were lost in follow-up because they stopped coming in to the outpatient clinic. Among the lost patients and those who completed follow-up, statistically significant differences were only found for sex (more men lost, P=.022).
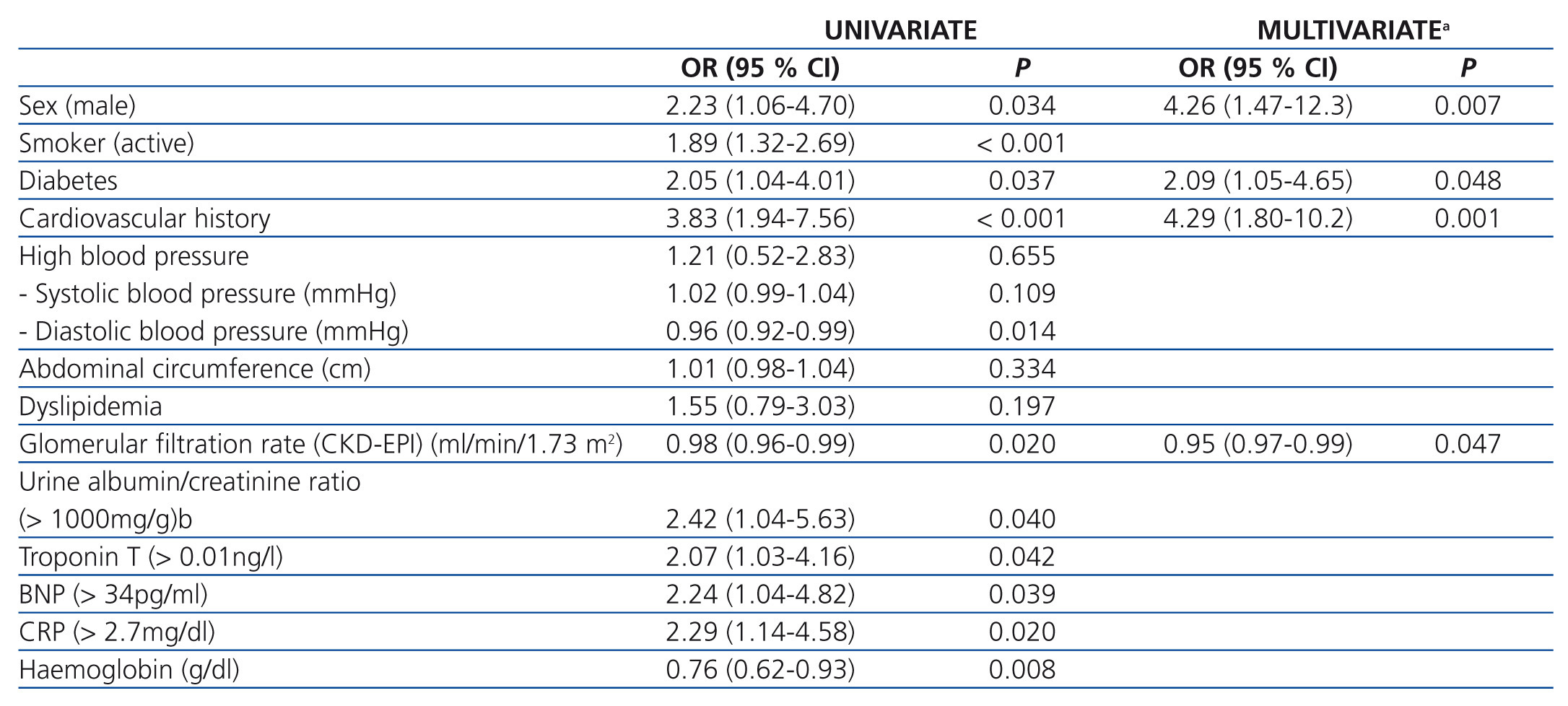
The univariate analysis revealed that factors that were associated with having an endpoint event (cardiovascular event or death due to non-cardiovascular cause) were male sex, active smoking, diabetes mellitus, low diastolic blood pressure, cardiovascular history, lower GFR, an urine albumin/creatinine ratio greater than 1000mg/g (when we found 300mg/g, we obtained a value of P=.14), troponin T levels greater than 0.01ng/l, BNP levels greater than 34pg/ml, CRP levels greater than 2.7mg/dl and low haemoglobin levels (Table 4). A survival analysis was performed for the endpoint event with Kaplan-Meier curves in order to evaluate their associated with albuminuria levels (Figure 1). We found no significant differences between patients with and without progression of their CKD (P=.566).
Male sex, diabetes mellitus, cardiovascular history and reduced GFR maintained their independent predictive value on multivariate analysis by logical regression.
DISCUSSION
Classic cardiovascular risk factors such as being male, diabetic, having a higher stage of kidney disease or having a cardiovascular history are independent predictors of cardiovascular events and mortality in patients with CKD.
The incidence of events in our population is around 5% annually, findings that are slightly lower than previously published series.19,20 This is probably due to a different distribution of patients by stages in our series (with a greater number in stage 3), the younger age of our patients and the lesser history of cardiovascular risk factors. In addition, the distribution of cardiovascular events increases with kidney disease stage. However, this progression disappears when mortality is combined in the endpoint event. The reason is probably the same since an event in stages 1 and 2 leads to a significant increase in the total percentage.
As in our case, male sex has been shown to be an independent factor for cardiovascular events and mortality in populations with and without kidney disease.21,22 However, age does not achieve a significant value between both groups. This is probably because of the very narrow age range in our patients. Conversely, tobacco use, which is associated with having an event, loses its predictive value. This is because the majority of smokers have a cardiovascular history. In addition, the percentage of smokers in our outpatient clinic is low compared to the general population.23
The association between kidney disease and cardiovascular events is known and has been studied broadly.4,5 The element that contributes most to an increase in these events is probably endothelial dysfunction given that this is considered to be the first step in the development of atheromas. This endothelial damage is not only explained by classic cardiovascular risk factors but also by the microinflammation environment in patients with CKD, uraemia, malnutrition, volume overload or calcium-phosphorus metabolism alterations.24-26 These data support the assertion that kidney disease itself is a cardiovascular risk factor and leads to the determination that, despite carrying out exhaustive monitoring of these factors, the population with CKD continues to be at an increased risk for an event.27 The classic RENAAL and LIFE studies on cardiovascular risk, which include diabetic and/or hypertensive patients, demonstrate that baseline creatinine is the most significant independent predictor for the development of cardiovascular events.28-30
The association between elevated cardiac markers and cardiovascular events indicates the presence of these subclinical asymptomatic lesions in patients with CKD.6 Several studies have demonstrated that both troponin and natriuretic peptide levels are elevated in patients with CKD; however, this situation does not seem to be related to the deterioration in GFR but instead is due to silent myocardial damage or volume overload.7,31,32 Therefore, it is not surprising that after adjusting the multivariate model for cardiovascular risk factors, these variables lose their independent predictive ability. This is because they are not effectors but simply cardiovascular risk markers and their baseline value should therefore be obtained in the nephrology department.33
Diabetes mellitus is a cardiovascular risk factor on its own. It causes an increase in cardiovascular events, as is seen in our data.34,35 However, although proteinuria shows an association with cardiovascular events, we have not been able to demonstrate that it is an independent predictive factor. This is probably due to the fact that diabetics make up the highest percentage of patients with a urine albumin/creatinine ratio greater than 1000mg/g, which causes it to lose its significance in multivariate analysis that includes diabetic patients. Conversely, the presence of hypertension was not associated with the presence of events, though low diastolic blood pressure was associated with having an event. Both high and low systolic and diastolic blood pressure has been associated with the presence of cardiovascular events and mortality, meaning that excessive control of hypertensive patients carries an increased risk that is similar to that seen in patients with high levels (J-curve effect).37,38 As can be seen in the distribution of CKD aetiology in Table 1, more than 40% of patients have vascular disease or diabetes. This confirms the high prevalence of these pathologies in patients with deteriorated kidney function. This distribution coincides with the data in the Spanish Nephrology Society registry.
We were not able to demonstrate an association between increased cardiovascular risk and the emerging factors mentioned previously. In our cohort, neither the presence of increased uric acid nor inflammation markers demonstrated an association with the combined endpoint event. This is probably due to low baseline levels of these variables. Therefore, it would seem that monitoring these variables is less relevant in the prognosis of these patients when compared to the classic factors. These data lead us to think that indiscriminate measurement of these variables in nephrology department is, for the moment, not justified when compared to the classic cardiovascular risk parameters.
Our study has some limitations such as being a single-site study and it lacks the echocardiographic parameters necessary to perform a more exhaustive study of heart disease. As these are consecutive patients, the distribution of patients by stage is not homogeneous and above all the results are valid for the population studied (patients in an outpatient nephrology clinic). In addition, the number of patients and the follow-up time are also limitations of the study.
In conclusion, male sex, diabetes mellitus, having a reduced GFR (CKD-EPI) and a history of cardiovascular risk are independent predictors of cardiovascular risk factors and mortality in patients with CKD (stages 1-4). In addition, the presence of an albumin/creatinine ratio greater than 1000mg/g is associated with a greater number of events.
Conflicts of interest
The authors declare that they have no conflicts of interest related to the contents of this article.
Table 1. Baseline characteristics of the study population
Table 2. Variables measured at baseline in the study population
Table 3. Cardiovascular events and mortality distributed by stages.
Table 4. Univariate and multivariate analysis for combined event
Figure 1. Kaplan-Meier survival analysis between patients with a urine albumin/creatinine ratio above or below 1 g/g (log-rank 5.99, p &