Dear Editor,
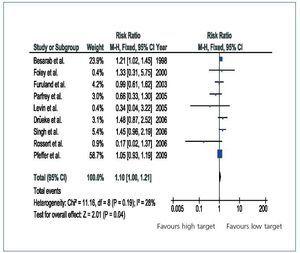
Although the results from the TREAT1 study only apply to diabetics, strictly speaking,2 the comparison between high and low haemoglobin targets affects all types of patients. The metaanalysis by Phrommintikul et al. is currently the most complete overview of the effect of high haemoglobin targets on mortality in chronic kidney disease.3With a percentage of diabetics near 40%, the mortality risk ratio with a high haemoglobin target compared with a low target was 1.17 with a 95% confidence interval (CI) between 1.01 and 1.35. When we add the results from the TREAT study, which has a higher overall percentage of diabetics (near 66%) the mortality risk ratio decreases slightly to 1.10 with a 95% CI between 1.00 and 1.21 (Figure 1). These results contradict the hypothesis that the increase in mortality with high targets is limited to diabetic patients. The only indication for exploring this hypothesis in later studies would have been if the mortality risk ratios for diabetics had been higher than for nondiabetics in the preliminary clinical trials.3 But nothing in these studies suggests that this is the case. We must not forget the significance of the meta-analysis results from all of the published controlled randomised studies: the search for high haemoglobins may increase the risk of mortality by a small but important amount (up to 21%), while the probability of high haemoglobins decreasing mortality is practically non-existent. In contrast, the improvement in quality of life generated by high haemoglobin levels is clinically insignificant.4 Since differences between diabetics and non-diabetics have not been shown, this interpretation should apply to all patients. In absolute terms, diabetic patients will be more vulnerable to the harmful effects of high haemoglobin targets, since they have a higher absolute risk of death, but we must not ignore that non-diabetic patients also have an added risk of mortality. In the case of stroke, the situation is quite similar: of the three data-bearing studies published prior to TREAT, the stroke risk ratio for a high target was 1.53, with a 95% CI of 0.89 to 2.64. When the TREAT is added, the combined risk ratio becomes 1.81, with a 95% CI of 1.37 to 2.39, without statistical heterogeneity among the studies, that is, without any indication that the TREAT results would be different from the rest (our own calculation). The relative risk of stroke where targets are high is higher than risk of death. These data do not correspond with the practice of setting higher haemoglobin targets in non-diabetics than in diabetics, as De Francisco et al.2 propose.
Figure 1. Meta-analyses of the effect of high haemoglobin targets on mortality in chronic kidney disease.