Dear Editor: We read with great interest the letter by Calle et al.1 describing the case of a patient who underwent a kidney transplant and developed a pneumonitis caused by sirolimus. They related that there are, until now, only seven cases reported of recovery from pneumonitis caused by sirolimus.
We would like to describe the case of a 27-year-old woman with a two-year history of haemodialysis for endstage renal disease underwent a haplo-identical, living kidney, donor transplantation. Following the procedure, she began immunosuppressive therapy with tacrolymus, mycophenolate mofetil, and steroid. Her renal function was stable and she was discharged with normal serum creatinine levels.
Two months after beginning immunosuppressive therapy she presented with diarrhoea of unknown aetiology. After recovery from the diarrhea, the patient was discharged while using mycophenolate sodium and metronidasol. Six months later, she was admitted with another episode of diarrhea and the tacrolymus was switched to sirolimus.
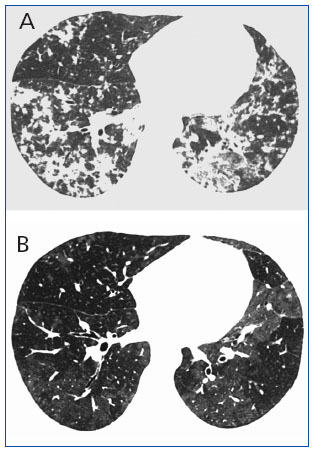
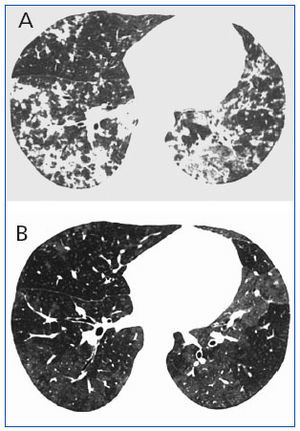
Ten months after initiation of the sirolimus treatment, the patient was admitted with fever, shortness of breath, and dehydration. Chest X-rays and high-resolution CT of the chest demonstrated bilateral areas of nonhomogeneous air space consolidation, mainly in the left upper lobe and lower lobes (figure 1A). Bronchoalveolar lavage revealed hypercellularity with lymphocytosis, and the microbiological evaluation was negative for bacteria, fungi, and viruses. Serological tests for cytomegalovirus were negative. The patient began an empirical, antiinfection treatment with intravenous azithromycin and ciprofloxacin, with no response. The fever persisted with antibiotic treatment and sirolimus was thought to be the cause of the symptoms. When sirolimus was switched to azathioprime symptoms improved within 10 days, and were resolved in 30 days. On the follow-up chest X-ray and high-resolution CT, 30 days after sirolimus discontinuation, the parenchymal abnormalities had improved, with accentuated reduction of the air-space consolidation pattern. There were persisting residual areas of bilateral ground-glass opacities on the high-resolution CT (figure 1B).
Sirolimus (rapamycin) is a potent immunosuppressive drug that has been successfully used in solid organ transplant recipients as an alternative to calcineurin inhibitor therapy2-4. The most common side effects associated with this drug are dose-dependent hyperlipidemia, and thrombocytopenia. Unlike calcineurin inhibitors, sirolimus does not induce acute or chronic nephrotoxicity. However, in very rare cases, patients treated with sirolimus may exhibit severe pulmonary toxicity2,3.
The symptoms of pulmonary toxicity related to sirolimus are generally nonspecific, and may include a dry cough, dyspnea, fatigue, and fever, frequently leading to the initial diagnosis of pulmonary infection5. Some reports have described histopathological patterns as a result of sirolimus pulmonary toxicity, but these findings are usually nonspecific, consisting of bronchiolitis obliterans with organizing pneumonia, interstitial pneumonitis, and nonnecrotizing granulomas2,4. For this reason, a lung biopsy is not essential, and the diagnosis of this condition must fulfil the following criteria: presence of lung disease on imaging tests, exclusion of pulmonary infection or other lung disease, and clinical improvement after drug withdrawal, independent of the pulmonary biopsy4,5. All these criteria were fulfilled in the patient presented here, who showed significant imaging and clinical improvement after withdrawal of sirolimus.
Due to the increased use of sirolimus, radiologists interpreting imaging studies of transplant patients using this drug should be aware of the imaging features associated with this potentially treatable complication. Although some previous authors reported the use of CT2,3,5, to our knowledge, there are no reports illustrating and discussing the highresolution CT findings of pulmonary toxicity due to sirolimus.
Figure 1. High-resolution CT at the level of the lower lobes (A) (obtained at the time of clinical presentation when respiratory symptoms were evident) demonstrates areas of non-homogeneous air space consolidation in the lower lobes, and mild ground-glass opacities