In 2009, the Framework Document on Managing Chronic Kidney Disease Care in Aragon was drafted by a multidisciplinary working group that comprised healthcare professionals, healthcare management professionals and members of kidney patient associations (ALCER Aragon). A structured, decentralised clinical management model was established based on grouping patients by diseases, identifying opportunities for improvement and describing activities through their processes.1–3 The patient and family were placed at the centre of the process map, and a continuous improvement cycle was introduced. Moreover, a series of indicators—both technical and perceived—were monitored to periodically assess the patient's evolution. This systematic and planned measurement of quality indicators, together with feedback and benchmarking,4,5 enabled us to achieve the objectives. Moreover, activities that are unrelated to the final process were also taken into account. These are information to patients and healthcare personnel, collection of management and indicator data, training of personnel and inspection of facilities.6,7 In this document, we evaluate the response to this intervention by means of monitoring the main indicators.
Improvement programmes centred on the following strategic plans were established at all nephrology units:
- -
Recovery of the patient's role in decision-making.
- -
Improvement of information systems.
- -
Designing a registry of patients undergoing renal replacement therapy in the autonomous community.
- -
Resolution of structural limitations: installing water treatment units to obtain ultrapure water in hospitals lacking the same and renewing equipment at dialysis centres.
- -
Increasing the percentage of patients on special techniques.
- -
Improving the critical points of the care process:
- •
Optimisation of management of patients with ACKD: equity, reduction in variability.
- •
Promoting kidney transplants from living donors.
- •
Promoting home dialysis techniques.
- •
Promoting conservative kidney management.
- •
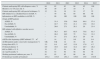
Analysing the main indicators after the development and implementation of the management process has allowed us to observe a significant improvement. The various clinical, nutritional, analytical and evolution-related parameters in the different RRT techniques have reached similar ranges to routine nephrology practice and are even higher than the national averages in some aspects.8 A brief selection of the changes among the other indicators is reflected in Table 1.
Evolution of the main technical quality indicators.
| 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | |
|---|---|---|---|---|---|---|
| Patients undergoing HD with ultrapure water, % | 64 | 62 | 63 | 68 | 62 | 100 |
| Monitors over 10 years old, % | 36 | 30 | 25 | 10 | 5 | 2 |
| Patients undergoing HD with special techniques, % | 12 | 16 | 19 | 18 | 17 | 22 |
| HD initiated on a scheduled basis in ACKD, % | – | 70 | 82 | 84 | 86 | 88 |
| Information on RRT modalities in ACKD, % | – | 90 | 100 | 100 | 100 | 100 |
| Origin of RRT patients | ||||||
| ACKD, % | – | 31.4 | 35.6 | 50.8 | 64.4 | 57.4 |
| Not ACKD, % | – | 42.7 | 37.3 | 21.1 | 15.6 | 19.2 |
| Unscheduled, % | – | 26.6 | 27.1 | 28.1 | 20 | 23.4 |
| HD initiated with definitive vascular access | ||||||
| ACKD, % | – | 76.3 | 85.7 | 65.5 | 75.8 | 81.5 |
| Not ACKD, % | – | 26.2 | 36.5 | 75 | 71.4 | 33.3 |
| Unscheduled, % | – | 14 | 27.1 | 28.1 | 20 | 16 |
| eGFR at the beginning of RRT ml/min/1.73m2 | – | 14 | 12 | 9.6 | 10 | 9.4 |
| ACKD patients under conservative management, % | UK | UK | 12 | 16 | 22 | 20 |
| Living donor KTx, % | 5.3 | 9.4 | 14.7 | 12.9 | 17.9 | 4.7 |
| Peritoneal dialysis, % | 8.9 | 18.9 | 22.4 | 32.2 | 28.7 | 28.2 |
| Kt/V in PHD >1.3, % | 32 | 37 | 34 | 36 | 46 | 53 |
| At 3 and 6 months, % | 52 | 53 | 50 | 58 | 64 | 78 |
| Working peritoneal catheters per year, % | 91 | 93 | 92 | 88 | 94 | 93 |
| Peritonitis per months of treatment | 1/31.2 | 1/34.3 | 1/41.2 | 1/38.4 | 1/43 | 1/43.6 |
UK: unknown.
We feel that the involvement of healthcare personnel and patients in management and the collaboration of the healthcare authorities facilitates the implementation of programmes that may improve healthcare.9,10 The implementation of the above-mentioned processes was especially difficult due to being performed at the time of the economic crisis, with significant financial limitations. The fact that the processes performed are effective (they truly improve the patients’ situations) and efficient (they improve them with a reasonable investment and in many cases actually save money) has facilitated the creation of these units and treatment techniques.
Please cite this article as: Lou Arnal LM, Berni Wennekers A, Gracia García O, Logroño González JM, Gascón Mariño A, García Mena M, et al. Utilidad de un programa de calidad asistencial para la gestión clínica de las enfermedades nefrológicas en Aragón. Nefrología. 2017;37:345–347.