Henoch-Schönlein purpura (HSP) is a leukocytoclastic vasculitis affecting small-vessels that is rarely seen in adults. Lung involvement is extremely rare, with an unpredictable clinical evolution and high rates of mortality.1,2
We report the case of a 69-year-old male patient with IgA nephropathy and a bilateral alveolar haemorrhage in the context of HSP. As for his personal history, he suffered from hypertension and atrial fibrillation, wore a mechanical prosthesis and was undergoing treatment with oral anticoagulants. The patient was admitted due to fever, dyspnoea, oedemas, coughing and expectoration. On admission, a deterioration of kidney function was observed (Cr 1.67mg/dl; GFR 41ml/min) as well as leukocytosis with a left shift. Following diuretic and antibiotic treatment, an improvement in kidney function occurred (Cr 0.9mg/dl, GFR 82ml/min) and the leukocytosis decreased. A few days later, the patient presented again deterioration of kidney function (Cr 2.1mg/dl), anaemia (Hb 7.5g/dl) along with purpuric lesions of the lower limbs. The tests performed showed: normal albumin, cholesterol and lactate dehydrogenase; an ESR of 52mm, urine element and sediment with +++proteins, ++++Hb, >100 red blood cells/field, 24-hour urine protein of 1870mg; IgA 437.00mg/dl, normal remaining immunoglobulins and complement, antinuclear antibodies, anti-neutrophil cytoplasmic antibodies, anti-glomerular basement membrane antibodies and negative viral serology testing. Haptoglobins < 25, blood smear without schistocytes, positive direct Coombs test. Urological ultrasound with no pathological findings.
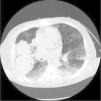
In light of suspected vasculitis, treatment was initiated with three boli of methylprednisolone 500mg on consecutive days, followed by prednisone at 1mg/kg every 24 hours. 72 hours later, symptoms of haemoptysis and anaemia appeared; a chest X-ray and chest CT scan were performed, showing findings suggestive of a bilateral alveolar haemorrhage and the presence of intraparenchymal pulmonary haematoma (Figs. 1 and 2). Treatment was initiated with a bolus of 500mg/m2 cyclophosphamide and immunoglobulins at 2g/kg, spread across five doses. Five days later, frank haemoptysis, anaemia and significant respiratory effort occurred, prompting a transfer to ICU, where orotracheal intubation and mechanical ventilation were performed. The patient also required aspiration due to massive bleeding.
During the patient's stay in the ICU, six sessions of plasmapheresis were performed on alternate days, and treatment with corticosteroids was maintained. A clinical and analytical improvement was seen over the subsequent days and extubation was performed 13 days later, with normalised kidney function and no new bleeding episodes. Finally, a kidney biopsy was performed in which 15 glomeruli were observed, four of which were sclerosed while the others showed the presence of diffuse segmental lesions in the form of endocapillary and mesangial proliferation and glomerular necrotic lesions. Interstitium with mild fibrosis and patchy inflammatory infiltrate. Positive immunofluorescence in the face of granular mesangial IgA (++), IgM (++) and C3 (++). After three months in hospital, the patient was discharged on a monthly immunoglobulin treatment and a decreasing corticosteroid regimen. Due to the risk of superinfection, combined treatment with other immunosuppressants was postponed until the pulmonary haematoma had resolved.
At the last hospital visit, from a clinical point of view the patient presented without dyspnoea, and clear improvements were seen in his lung X-ray and laboratory tests: creatinine 1.2mg/dl, GFR 61ml/min, urine with minimal microscopic haematuria (15–20 red blood cells/field) with a urine protein:creatinine ratio of 238.6mg/g, and no anaemia or leukocytosis.
HSP is a form of leukocytoclastic vasculitis that affects the small vessels and, on rare occasions, the medium vessels. Its symptoms are characterised by non-thrombocytopenic palpable purpura (100% of cases), arthralgia in the lower limbs (82%), gastrointestinal involvement (50–75%) and renal involvement (20–50%). Musculoskeletal, neurological, pulmonary, cardiac and ocular conditions have been described less frequently.1,2 The incidence in adults is around 1.3 cases per 100,000.3
The EULAR/PRINTO/PRES diagnostic criteria (2008) for HSP include, as a mandatory criterion, the existence of non-thrombocytopenic palpable purpura, predominantly in the lower limbs and, in case of atypical distribution, proven IgA deposition in the biopsy. In addition, at least one of the following characteristics is required: diffuse abdominal pain, biopsy with IgA deposition, arthritis or arthralgia and renal involvement (haematuria or proteinuria).4
Renal involvement usually manifests in the form of mild glomerulonephritis, with microscopic haematuria and proteinuria, and a biopsy showing IgA nephropathy.5,6
Lung involvement in HSP is extremely rare and includes, above all, haemorrhage or interstitial disease. Diffuse alveolar haemorrhage, which may present immediately following the HSP diagnosis, or even several years later, has an unpredictable clinical evolution and is associated with high rates of mortality.7,8
Chest X-rays are usually non-specific and computed tomography is required to confirm the findings. The severity of the situation warrants the use of intensive immunosuppressive therapy9; treatment combined with glucocorticoids and cyclophosphamide, azathioprine, methotrexate or rituximab is common. Plasmapheresis has also been noted as a therapeutic option.
The most common aetiologies that coexist with alveolar haemorrhage and glomerulonephritis are anti-neutrophil cytoplasmic antibody-associated vasculitis and anti-glomerular basement membrane antibody disease. Although uncommon, HSP should be considered among the differential diagnoses in a patient with pulmonary haemorrhage and renal involvement.
Please cite this article as: Belmar Vega L, Fernández-Díaz C, Palmou Fontana N, Rodrigo Calabia E, Martin Penagos L, Arias Rodríguez M, et al. Hemorragia pulmonar en paciente con nefropatía IgA. Nefrologia. 2017;37:347–349.