En junio de 2009, la OMS declaró la pandemia por virus de la influenza A de origen porcino (H1N1). Desde entonces, los nefrólogos fuimos afectados en varias de nuestras actividades. Disminuyó la asistencia al trabajo del personal de salud al cuidado de pacientes renales crónicos. Aparecieron nuevos casos de fallo renal agudo asociados a la infección viral, la mayoría en adultos jóvenes, con alta tasa de mortalidad. Hubo contagios en pacientes trasplantados renales y se retrajo transitoriamente la procuración de órganos en la semanas de mayor contagio. Entidades científicas se movilizaron para consensuar protocolos de evaluación y tratamiento con el fin de disminuir el impacto de la pandemia en pacientes renales.
INTRODUCTION
In early April this year, a new influenza A virus was identified, hemagglutinin 1 and neuraminidase 1 (H1N1), with significant changes in both proteins, 27.2% and 18.2% of the amino acid sequence, respectively, when compared with the previous H1N1 strain isolated in 2008. This implies a lack of immunity in the population, except for some people older than 60,1 and high human to human transmission.2,3 It has spread widely and rapidly in both hemispheres, prompting the World Health Organisation (WHO) to declare a Pandemic alert Phase 6 on 10 June. Given the historical context, it could infect 30% of the world population.4 This new virus of swine origin (S-OIV, swine-origin influenza virus) appears clinically as a febrile respiratory influenza, ranging from mild to severe which can affect all ages, although 80% has occurred in people under 30 years of age. Both fever and cough occur in more than 90% of cases, and a third of them are associated with gastrointestinal symptoms (vomiting and diarrhoea). It occurs equally in both sexes,5,6 and has an adequate therapeutic response to neuraminidase inhibitors, oseltamivir and zanamivir.7
The nephrologist has an important role in the pandemic, since we are part of the health team treating patients with kidney problems such as acute renal failure associated with infection by S-OIV (H1N1), and we are also involved in the care of patients with chronic kidney problems (undergoing transplant, dialysis or treated with peritoneal dialysis, PD) and in organ donation in areas with infected patients.
INVOLVEMENT OF THE HEALTH TEAM SPECIALISING IN RENAL PATIENTS
Although there is significant asymmetry between the countries of the region, generally the number of nurses trained in renal replacement treatment and physicians specialising in nephrology is reduced in Latin America, and this contrasts with the increased incidence of chronic kidney disease (CKD) in need for replacement therapies.8,9 The care provided by personnel during a pandemic is a priority. Frequent hand washing, use of equipment and specific strategies for treating infected patients reduce the risk of personnel passing on the disease. According to the Pan American Health Organisation (PAHO), the overall impact is still moderate in countries such as Uruguay, and mild in the USA. In Argentina, this information has not been provided to the PAHO, but it is clear that in some dialysis units the level of absenteeism has reached a third of staff. This is due to several factors: the first is the risk of spreading the disease by health workers (nurses, doctors, administrators, etc.), who stay at home for a week to prevent contact with patients and the rest of the team. The second reason is government regulation. Personnel at high risk if they catch the disease (e.g. pregnant women, patients with chronic bronchial or immunosuppressant problems) make use of compulsory permits until the end of the pandemic. Finally, as a precautionary measure, the Argentinean Ministry of Education ordered the closure of schools, based on nonpharmacological strategies which have proven effective in alleviating the pandemic.11 This has resulted in many children being left at home in metropolitan areas, forcing staff, especially mothers of young children, to seek special permission to stay at home to care for their children. For all these reasons, the Argentinian Nephrology Society together with companies and organisations in nuclear dialysis centres have prepared recommendations to protect health personnel, and to prevent and adequately treat patients on dialysis.
ACUTE RENAL FAILURE ASSOCIATED WITH INFLUENZA A (H1N1)
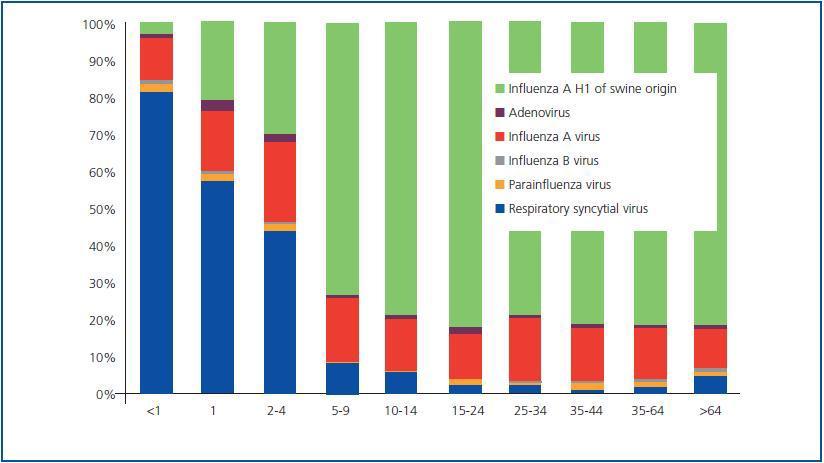
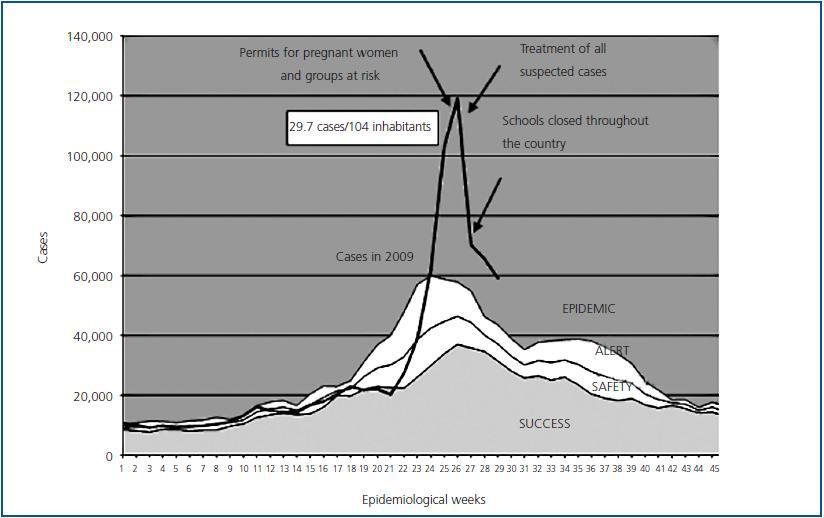
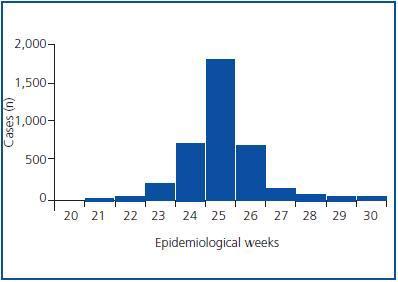
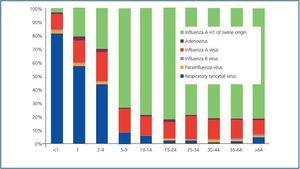
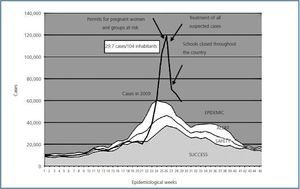
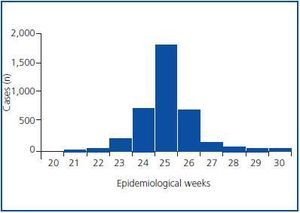
Since the first cases in Mexico, USA and Canada, it was reported that infected patients may develop serious respiratory symptoms12,13 and some of these with acute renal injury (ARI). The typical case we see in Argentina is the young adult patient, with or without comorbidities, who rapidly develops acute respiratory failure (ARF) 2-3 days after the onset of the symptoms, requiring mechanical ventilation, due to severe persistent hypoxaemia, usually with PAO2/FIO2 ratio values < 150. During the first week of, oliguric ARI may occur, requiring renal replacement therapy. The ARI is no different to that in seasonal influenza cases, particularly in children.14 It occurs in the context of systemic inflammatory response syndrome typical of viral infection that some experts call ¿viral sepsis¿, with multiorgan dysfunction, in this case respiratory, haemodynamic, hepatic, renal and haematological. The renal involvement of the sepsis is by hypoperfusion mediated by cytokines and other endocrine systems, and occasionally is accompanied by disseminated intravascular coagulation.15 The organ of greatest impact on influenza infection is the lung, so another mechanism of renal lesion is probably induced ischemia due to severe persistent hypoxaemia. The association of the latter with acute renal involvement is clearly established.16-18 Finally, rhabdomyolysis is a process directly related to renal injury in seasonal influenza.19-27 Rhabdomyolysis induces an aggression by vasoconstriction, formation of tubular casts and direct cytotoxicity due to heme.28 During the pandemic in Argentina, there were different levels of creatine kinase reported, up to 30,000U/ml.29 Although to date there is no documented direct cytopathic injury in kidneys of patients with influenza, some authors have suggested it as cause of ARF.30 Viremia is transient and extrapulmonary tissue injury limited, therefore, this mechanism is unlikely.31 In one reported case of ARI associated with seasonal influenza A, the histopathological changes observed were due to toxicity and myoglobin deposition, without any injury directly attributable to the virus observed.32 Of the cases reported as influenza-like illness (ILI) in adults and studied with virological techniques in the current pandemic in Argentina, the majority was influenza A (Figure 1). 1% of these patients required admittance to the hospital. One fifth of those hospitalised were referred to the ICU and the majority required mechanical ventilation.33 Although the possibility that an infected patient displays a shift towards respiratory failure with ARI is less than 0.5%, experience shows that these patients have a mortality exceeding 90%. A feature of the pandemic is that the cases steadily appear until reaching a peak, and in Argentina during epidemiological week 26, there were 29.7 suspected cases of ILI per 10,000 population (Figure 2). In this period of increased case mix in the metropolitan area, it was common to see an increase in critically ill patients requiring mechanical ventilation, especially in referral centres (Figure 3). Simultaneously, more nephrological services were demanded, which put the public health system on a state of alert.
CHRONIC RENAL PATIENTS
The patient with chronic kidney disease is considered an infection risk, and specifically with the influenza virus, so different organisations recommend preseasonal prophylaxis by vaccination.34-36 Pharmaceutical companies are already developing a new vaccine against H1N1, which will probably be offered in a triple formulation (H1N1, H3N2 and influenza B). After the epidemic of H5N1 (bird flu) vaccine production was improved.37 Today, the WHO estimates that in an optimal setting production could reach 4.9 billion doses annually. The possibility of vaccinating patients in Argentina will then depend on world production, the cost, the amount purchased by industrialised countries and the reserve ratio for emerging countries with little or no access to new vaccines.38
The patient undergoing chronic haemodialysis is in a particular situation: he is ambulatory but spends several hours with other patients in an enclosed area. Thus, there is a strong possibility of infection in the haemodialysis room. In the above recommendations, the Argentinian Nephrology Society stresses the importance of treating suspected cases inside and outside the dialysis room, and how to prevent such patients from spreading the disease. In addition, it highlights the need to adjust the dose of oseltamivir to renal function.39 Work is currently proceeding in the reporting of patients undergoing chronic dialysis with suspected cases and their evolution, to show how the pandemic affected this population.
ORGAN DONATION AND SOLID ORGAN TRANSPLANTS
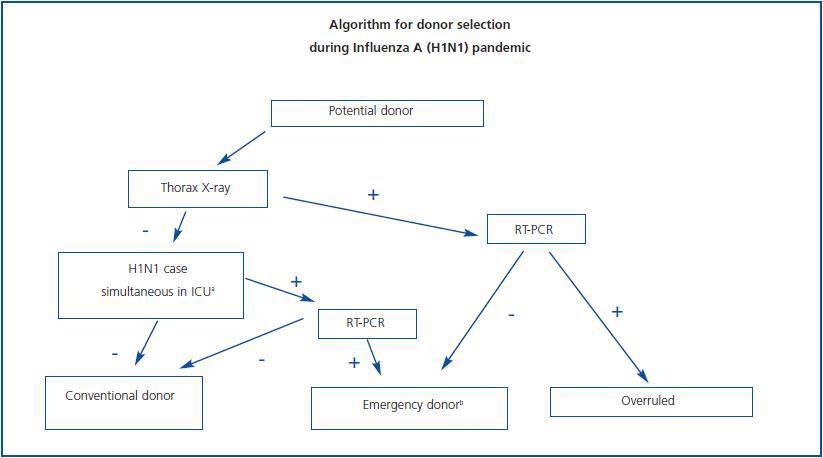
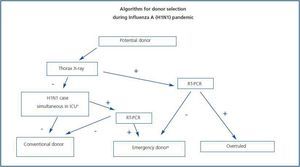
In 2008, Argentina reached a rate of 13.1 cadaver donors per million inhabitants. There are seasonal and geographical variations (e.g., in the City of Buenos Aires, the equivalent rate was 24.9 pmp). During the month of June, which is winter in this hemisphere, the number of areas was reduced by approximately 50% in the metropolitan area.40 This coincided with the progression of patients with acute lung injury in the ICU of referral and donor hospitals, displacing the more prevalent pathologies that lead to brain death. Literally, the ICUs were filled to capacity with patients requiring mechanical ventilation. Then came questions about whether donors could be sought from those in contact with patients diagnosed with H1N1, if there was a possibility of horizontal, intranosocomial, transmission in the ICU, etc. So much so that experts from procurement agencies along with transplant organisations, infectious diseases and intensive care departments met and agreed on a donor selection algorithm during the pandemic, based on the history and clinic, as well as viral detection by RT-PCR (Fig. 4). Some kidney transplant patients developed unfavourably, as with the general population. Transplant centres in the metropolitan area chose to avoid scheduled periodic inspections and erformed triage of patients with febrile syndrome and, at the above meeting, developed recommendations for treatment.41
These stated that antiviral therapy in suspected cases should continue for 10 days (antiviral treatment in the general population is 5 days). This is supported by some work that identified a prolonged respiratory viral excretion in inmunocompromised patients.42,43 In addition, the SAT Committee on Infectious Diseases is implementing a register of transplant patients infected with influenza A.
CONCLUSIONS
The first reported pandemic in the twentieth century, the ¿Spanish flu¿ (1918), coincidentally influenza A H1N1, caused the death of 20 to 40 million people. At the dawn of this new century, we find ourselves in the same situation but with knowledge of the viral biology and genetics that give us therapeutic and technological tools to deal with it. Nephrologists carry out a major role in the influenza pandemic. The high mortality of, mostly young, patients with ARI presents a challenge. Adequate and timely use of antivirals may improve the development, and it is hoped that the specific vaccine to immunise staff and uninfected patients will arrive soon. Education and protection of persons under renal replacement treatment and the care staff working with us are a priority. The recommendations of experts may help to reduce infection rates and mortality.
Thus, with adequate health measures, medical management of high risk potential infection scenarios and the use of new technologies, we may improve the results of previous pandemic experiences.
Figure 1.
Figure 2.
Figure 3.
Figure 4.