To the Editor:
Posterior reversible encephalopathy syndrome (PRES) can occur in recipients of solid organ transplants associated with calcineurin inhibitors. The incidence of this syndrome in kidney transplant recipients is low, approximately 0.34%,1,2 and should be suspected when neurological symptoms arise in association with characteristic lesions found in cerebral magnetic resonance (CMR) images, which revert after reducing or suspending the dose of tacrolimus. In order to resolve this condition and avoid neurological sequelae, an early diagnosis and suspension of the causal calcineurin inhibitor is needed.3
Here we present the case of a kidney transplant recipient who developed atypical PRES associated with tacrolimus.
Ours was a 32-year old male patient with a personal history of arterial hypertension and stage 5 chronic kidney disease, who had received a kidney transplant 2 years earlier with the prescription of sirolimus, but who was switched to tacrolimus due to gastrointestinal intolerance to the first drug, and had been taking tacrolimus for the past 5 months.
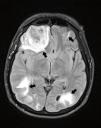
The patient sought treatment at our hospital of IV level of complexity due to a first-onset generalised tonic-clonic seizure of 60 seconds in duration. A physical examination showed that the patient was without fever, had a blood pressure of 187/133mm Hg, and was sleepy in a postictal state, with no other relevant findings. A laboratory analysis revealed mild leukocytosis, hyperlactaemic metabolic acidosis, creatinine: 5.43mg/dl (baseline: 3.0mg/dl), and normal electrolyte levels. We performed a simple cerebral computed axial tomography (CAT), which revealed several hyperdense lesions, the largest of which was in the right frontal lobe; we then administered a CMR (Figure 1), which revealed several lesions: frontal lobe with mass effect and cortical/subcortical without restrictions in the ADC sequence. We performed several analyses to determine the extent of the lesions, including: cerebrospinal fluid analysis, haemocultures and urine cultures (negative), and a stereotactic biopsy of the right frontal lobe lesion that revealed reactive gliosis and small foci of interstitial bleeding. Given these findings, we were able to rule out other possible diagnoses and settled on the probable diagnosis of neurotoxicity from tacrolimus. We decided to suspend the medication and observe the patient’s evolution, which was very favourable from a neurological standpoint. The patient was discharged under a renal replacement therapy regimen, since basal GFR were not recovered, and no immunosuppressant medications were prescribed. Three months later, a follow-up simple cerebral tomography (Figure 2) showed that the supratentorial lesions had healed, with only a small encephalomalacic area in the right frontal lobe at the site of the haematoma.
DISCUSSION
Calcineurin inhibitors have been described as potent immunosuppressants that are considered to be quite effective in the prevention of acute transplant rejection. However, these drugs are associated with several adverse side effects; in the specific case of tacrolimus (also known as FK-506 or Fujimycin), reports have described increased incidence rates of diabetes and nephrotoxicity, among others, but nephrotoxicity in particular, with even greater incidence rates than those produced by cyclosporine.4 The symptoms include headache, trembling, paraesthesia, visual impairments, convulsions, and coma.5 One form of presentation of this neurotoxicity is PRES, a clinical/radiological entity that is uncommon and was first described only recently (1996).6 A CMR has been considered as the gold standard7 for diagnosing this condition; we typically see an increase in signal intensity for T2-weighted images in both posterior regions, with compromised cortical tissue due to the lack of regulation of posterior circulation.6 However, these signals were then described in the frontal region due to vasogenic oedema of the subcortical white matter.6,8 The FLAIR sequence (fluid-attenuated inversion recover) increases the capacity for detecting minute lesions. Diffusion weighted imaging sequences (DWI) and the apparent diffusion coefficient (ADC) are useful for differentiating vasogenic oedema with mild restriction from oedema with no restriction, which indicates reversibility.
Follow-up imaging controls are indispensable for supporting the diagnosis.1,6 There is no specific timeline established for these controls; some authors recommend 4 weeks after resolution of clinical signs. These controls can take place in the form of CMR or cerebral CAT scans.6
In our patient, we observed characteristics that can be considered atypical for this syndrome, such as increased involvement of the right frontal lobe, with cortical lesions and intra-lesion bleeding that surpassed the PRES lesions, making these typically reversible lesions progress towards irreversible damage and encephalomalacia, as observed in the follow-up cerebral imaging tests from this patient (Figure 2).
Conflicts of interest
The authors state that they have no potential conflicts of interest related to the content of this article.
Figure 1. Cerebral magnetic resonance, FLAIR sequence
Figure 2. Simple cerebral computed axial tomography, control