El síndrome de Sjögren primario es una enfermedad inflamatoria multisistémica que suele cursar con lesiones de las glándulas exocrinas originando síntomas de sequedad oral y ocular. La expresión clínica también incluye manifestaciones generales, afección extraglandular y desarrollo de linfoma. La asociación de enfermedad renal es frecuente. Habitualmente, la lesión observada corresponde a nefritis túbulo-intersticial. En cambio, es rara la afectación glomerular, así como los casos de fracaso renal agudo severo. Presentamos el caso de una mujer con síndrome de Sjögren primario que desarrolla un cuadro de insuficiencia renal aguda grave por glomerulonefritis crioglobulinémica con respuesta favorable a la terapia con esteroides, ciclofosfamida, plasmaféresis y rituximab.
Primary Sjögren´s syndrome is a multisystemic inflammatory disorder that mainly affects the exocrine glands and usually presents as dryness of the mouth and eyes. The wide clinical spectrum of the disease also includes general symptoms, extraglandular manifestations and lymphoma. It is frequently associated with renal diseases. Interstitial nephritis is the most common renal manifestation, but glomerular involvement and acute renal failure may also (rarely) occur. We describe a case of a female patient with primary Sjögren´s syndrome complicated by severe acute renal failure due to cryoglobulinemic glomerulonephritis. Treatment with steroids, cyclophosphamide, plasma exchange and rituximab successfully led to recovery from acute renal failure.
INTRODUCTION
Sjögren’s syndrome (SS) is a chronic autoimmune disease characterized by lymphoplasmacytic infiltration of the exocrine glands. It primarily affects lachrymal and salivary glands, giving it the name of dry eye syndrome. In the absence of other associated autoimmune diseases, it is known as primary Sjögren’s syndrome (pSS).
Half of pSS patients present extraglandular manifestations, most commonly arthritis and pulmonary disease. Renal damage by interstitial tubular nephritis is also a known complication of pSS. However, glomerulopathies and episodes of acute renal failure are only seen in exceptional cases.
Here, we describe the case of a patient affected with SS who develops cryoglobulinemic glomerulopathy with severe acute renal failure, requiring dialysis and with a strong response to immunosuppressor treatment.
PRESENTATION OF THE CASE
56 year-old female diagnosed with pSS 13 years before. Presented with dry syndrome, asthenia, and frequent episodes of polyarthritis. During this time, she received a prolonged treatment with non-steroid anti-inflammatory drugs (NSAI) and steroids. Additionally, methotrexate had been applied in recent months with slight improvement of the symptoms.
Three months after starting odontological treatment with dental implants, the patient was admitted with facial oedema, fever, and reduced urine output.
The physical examination revealed a general deterioration in physical state, blood pressure (BP) at 160/90 mmHg, fever, and submandibular oedema with evidence of an active infection in the lower dental arch. She did not present any distal oedema or skin lesions.
The chemical analysis detected Hb 9.2 g/dl, creatinine 2.9 mg/dl, urea 110 mg/dl, and normal liver profile, lipid profile, ANCA and immunoglobulins. ANA positive, anti-DNA negative. Low C3 and C4 levels, 46 and 1.6 mg/dl, respectively. Serology for HBV, HCV, and HIV negative. Haemocultures negative. ANA, anti-LA, anti-Ro antibodies, and rheumatoid factor (RF) were positive from the moment the patient was diagnosed with pSS. Hypocomplementemia was also occasionally presented. The urine sample showed proteinuria (2 g/l) and microhaematuria. The kidney ultrasound came back normal. The patient evolved into a low grade fever that evening, in spite of antibiotic therapy, and oliguria, requiring dialysis treatment.
Suspecting acute glomerulonephritis (GN), probably post-infectious given the mandibular infection and hypocomplementemia, a kidney biopsy was performed with the following results:
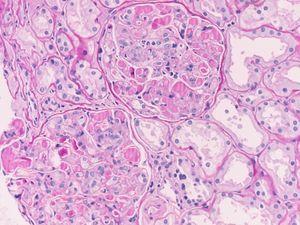
The cylinder for light microscopy contained 8 glomeruli that presented diffuse capillary occlusion due to thrombi of a PAS-positive proteinaceous material (figure 1). In some glomeruli, these were accompanied by segmented infiltration of inflammatory cells. Isolated centres of interstitial lymphoplasmacytic inflammation were present, with no alterations in the arteries.
In the direct immunofluorescence study (dIF), we observed intense positivity in the thrombi of IgG, IgM, kappa, and lambda, and to a lesser degree, C3 and IgA (figure 2). C1q and fibrinogen were negative. The ultrastructural study was performed afterwards.
Anatomopathological diagnosis
Glomeruli with massive intracapillary immunoglobulin thrombi indicating cryoglobulinemic glomerulopathy associated with SS.
Evolution
The analysis confirmed the existence of cryoglobulinemia (cryocrit 50%) and an IgM kappa monoclonal band, requiring 3 pulses of methylprednisolone and one pulse of 750 mg of i.v. cyclophosphamide. Given the severity of the situation, we decided to continue treatment with three sessions of plasmapheresis and four weekly doses of 375mg/m2 of rituximab.
The patient also presented complications in the form of a Candida infection from the dialysis catheter, which was resolved with antifungals and removal of the catheter. An infection by cytomegalovirus (CMV) was also detected and proceeded without symptoms, and it was controlled following a cycle of treatment with valganciclovir.
The patient showed a slow improvement in kidney function. After 9 weeks, the dialysis treatment was suspended. At 5 months, creatinine was at 1 mg/dl, GFR 42 ml/min/1.73 m2, the complement and RF were normal, and cryoglobulins negative. Proteinuria and sediments also normalized. The CD19 lymphocyte count in peripheral blood went from 21% pre-treatment to 0% post-treatment. The steroid dose was progressively reduced until stabilizing with 5 mg/48 h of prednisone.
Eight months after the episode, the patient was re-admitted with asthenia, polyarthritis, and epigastralgia. Purpura was observed in the lower limbs. The analytical study detected elevated RF and hypocomplementemia, with stable renal function and negative cryoglobulins. After a brief improvement, the patient was stricken with severe gastroenteritis with fever, severe vomiting and diarrhoea, followed by a reduction in diuresis. She continued to present oliguria, in spite of adequate hydration, such that the chemical analysis and renal biopsy were repeated. A cryocrit of 50% was observed as well as a recuperation of the CD19 lymphocytes in peripheral blood (23%).
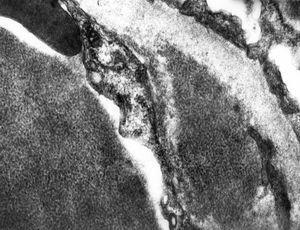
The renal biopsy showed a recurrence of the cryoglobulinemic glomerulopathy, containing 22 glomeruli, one of which was sclerosed; the rest also presented abundant hyaline thrombi (PAS+) with capillary occlusion and varying levels of monocytic infiltration (at times severe) in the capillary spaces (figure 3 and figure 4). Few areas of interstitial fibrosis were present. In dIF, the stain was preferentially intraluminal for the same antisera of the previous biopsy. The electron microscope analysis showed that the deposits had microtubular organization (figure 5).
With these findings, and taking into account the favourable evolution observed in the first episode, we applied the same therapeutic regimen. After applying haemodialysis for 3 weeks, the patient started to recover kidney function. At 3 weeks her creatinine levels reached 0.9 mg/dl, GRF 52 ml/min/1.73 m2, with normalized complements and negative cryoglobulins. We also observed in this episode an asymptomatic reactivation of the CMV infection with a good response to valganciclovir and an episode of a urinary infection that was resolved with outpatient treatment. No new complications have arisen in the 5 months since the last episode.
DISCUSSION
Although SS normally presents as xerostomia and dry keratoconjunctivitis, extraglandular manifestations are very common, and are responsible for the wide variability in the symptoms of this disease, as it can affect practically any organ. The most severe complication is the development of B cell lymphomas, observed in 5 – 7% of cases.
An estimated 25% of patients with pSS present with renal alterations. These tend to be cases of tubulointerstitial nephritis (TIN), which is primarily manifested by proteinuria and tubular dysfunction with evidence of lymphoplasmacytic infiltrates.1 It is rarely associated with renal failure, and when it is, this condition tends to be mild. The association of SS with glomerulopathies has been rarely described.
In a study of 60 patients with pSS and evidence of tubular and/or glomerular dysfunction, nine were biopsied, six presented TIN, and three glomerular disease, one of which was a cryoglobulinemic membranoproliferative glomerulonephritis (MPGN).2
In the recently published study by Maripuri et al., only 24 patients with pSS (0.3% of the 7,276 patients) were evaluated with renal biopsies, 17 had TIN, and seven presented glomerular lesions that included MPGN with cryoglobulinemia.1
Mixed cryoglobulinemia is associated with lymphoproliferative, autoimmune, and infectious diseases. In our field, the principal causal agent is HCV, while SS is the most frequent cause of mixed cryoglobulinemia in the absence of HCV infection.3 In the study by Ramos-Casals et al., cryoglobulins were detected in as much as 16% of pSS patients. However, only half of these were infected with HCV.4
The polyclonal activation of lymphocyte B (LB) characterized by pSS can in some cases evolve into an oligoclonal or monoclonal LB expansion with production of IgM kappa, which constitutes the principal monoclonal component of cryoglobulinemia. Finally, this monoclonal activation can arise in malignant lymphoproliferative diseases. In this sense, the detection of cryoglobulins indicates an increased risk of lymphoma progression.
It still remains to be verified if the intercurrent infectious processes precipitate the stimulation of LB and cryoglobulin synthesis in patients with SS. In the case we have presented, the initial breakout and recurrence of cryoglobulinemic glomerulonephritis were preceded by a submandibular infection and acute gastroenteritis, respectively.
The renal disease associated with cryoglobulinemia is heterogeneous, with type I MPGN being the most frequent histological pattern (80%). Other renal lesion patterns include proliferative diffuse or focal GN, and more rarely, membranous glomerulopathy. Monocyte infiltration is common, although some areas of glomerular segments can also include polymorphonuclears. Intracapillary thrombi are identified in approximately half of these cases and tend to be focal. Massive cryoglobulinic intracapillary thrombi, such as those found in our patient, are infrequent and usually present with a rapid deterioration of renal function.5
Three distinctive patterns have been described in dIF, one of which consists of a strong stain of intraluminal thrombi and peripheral mottling, the most characteristic pattern, and must indicate a diagnosis of cryoglobulinemia; however, only a small portion of patients with cryoglobulinemia exhibit this type of appearance.6
Regarding treatment, steroids and various immunosuppressors, cyclophosphamide or azathioprine, as well as plasmapheresis in the most severe cases, are traditionally used with poor results. Only 14% of patients remain in remission for long periods of time, with an elevated incidence of severe complications.7
Rituximab is a monoclonal antibody with anti-CD20 activity capable of producing a strong depletion in B-lymphocytes. Although it was initially indicated in the treatment of B lymphomas, its use in recent years has been extended given the positive results obtained.
It has been used in mixed essential cryoglobulinemia and cryoglobulinemia associated with HVC resistant to conventional immunosuppressor treatment, producing a clinical improvement in arthralgia and skin lesions, as well as decreased cryocrit and increase in complement. From the renal point of view, improved kidney function and a decrease in proteinuria have been observed. Cacoub et al. have reviewed 57 cases published on mixed cryoglobulinemia treated with rituximab. They observed a favourable clinical response in 15 out of 18 patients (83%) with compromised renal function. The response was complete in 75% of these cases, although 39% experienced recurrence, which tends to respond to new treatment cycles. In general, the treatment was well tolerated with few side effects.8 The use of rituximab creates a new expectation for the clinical management of these cases. Even so, very little data is available and new studies are needed to evaluate the costs/benefits of this treatment on a long-term basis.
Questions
Dr. Julia Blanco (Madrid). How do you explain the presence of kappa and lambda immunoglobulins in the biopsy?
Anwer. In cryoglobulinemia, the glomerular deposits detected by direct immunofluorescence in the renal biopsy reflect the composition of the serum precipitate. In type II mixed cryoglobulinemia, which would be the type corresponding to our case, monoclonal (usually IgM kappa) and polyclonal (IgG) immunoglobulins are present. The intracapillary thrombi in these cases usually stain with antisera for both immunoglobulins IgG and IgM, as well as for both kappa and lambda light chains. The monoclonal kappa component of the IgM would be hidden and overlapped by the positivity of both kappa and lambda light chains corresponding to the polyclonal IgG.
Dr. Antonio Barat (Madrid). Do you think that an acute tubular necrosis in the second biopsy could have contributed to the rapid deterioration in renal function?
A: In the second biopsy, focal alterations in the tubular epithelium are effectively evidenced, indicating an acute lesion that could simulate ischemic renal failure. In our opinion, as has occurred in other cases of severe glomerulonephritis, we interpret these changes to be secondary to the florid glomerular process that is presented by the patient rather than an acute tubular necrosis.
Dr. Miguel Ángel Frutos (Málaga). The objective after these two episodes of rapid deterioration in renal function is to avoid similar recurrences. What strategy will you use with this patient?
A: In our case, the patient presented two episodes of rapidly establishing and severe acute renal failure. In both the initial breakout and the recurrence, the patient was oliguric in a few hours and required prolonged haemodialysis treatment. On the other hand, just 2 weeks before the second episode, renal function was stable, cryoglobulins were negative, and CD19 LB were low (3%). Given the severity and magnitude of the episodes of renal failure and the absence of serum markers that could allow us to anticipate recurrence with a certain margin, we consider it necessary to apply immunosuppressive treatment as a preventative measure. Some cases from the bibliography have used various levels of rituximab treatments with success,9 although the proper dosage and duration of treatment remain to be determined. In our patient, the use of rituximab for maintenance could be useful in preventing new outbreaks.
Dr. Miguel Perdiguero (Alicante). In this case, could serial measurements of C3 and C4 aid in predicting outbreaks?
A: In our patient, each episode of renal failure was accompanied by hypocomplentemia. However, only 14 days passed between the onset of hypocomplementemia and the development of oliguria. This constitutes a short period of time that does not allow for proper planning of the treatment to be administered before the outbreak.
Dr. Simona Alexandrini (Madrid). Has any effort been put into finding some clone responsible for the production of cryoglobulins?
A: The chemical analysis showed the presence of a monoclonal IgM kappa spike, which reflects a monoclonal expansion of LB. Until now we have not been able to directly identify the presence of a cryoglobulin-producing LB clone in peripheral blood, since we do not have the necessary material for such an analysis at our centre.
Dr. Jesús Egido (Madrid). I was wondering if maintaining such a low dose of prednisone in the treatment following recuperation from the first episode might have facilitated the abrupt outbreak of the second.
A: The protocol for dosage and duration of maintenance treatment with steroids in cases of cryoglobulinemic glomerulonephritis is as yet unestablished. The majority of published cases tend not to describe the dose used, and as such, it is difficult to evaluate the influence of the use of low dosage or even the absence of steroids in the appearance of recurrences.
Dr. Manuel Praga (Madrid). Do you have any opinion on the use of bortezomib in similar cases?
A: Bortezomib is a selective proteasome inhibitor that has been demonstrated to be effective in the treatment of malignant gammapathies (multiple myeloma, plasmacytoma, leukaemia). Recently, 3 cases have been communicated on patients with type I cryoglobulinemia and skin vasculitis that were resistant to intensive steroid immunosuppressor treatment, alkylating agents, and even rituximab. Additionally, a significant decrease in cryocrit was observed, as well as a complete resolution of the skin vasculitis.
None of the patients presented data on renal damage, which is quite infrequent in cases of type I cryoglobulinemia.10,11
Acknowledgements
We would like to thank Novartis Pharma for the facilities for the presentation and discussion of this case at the meeting of the Nephropathology Club and GLOSEN.
Figure 1. PAS. Massive glomerular intracapillary thrombi
Figure 2. Intense positivity in intracapillary thrombi for anti IgC, IgM, Kappa and Lambda (In the direct IF image for IgG)
Figure 3. Recurrence of cryoglobulinaemic GN. PAS positive intracapillary thrombi and glomerular hypercellularity
Figure 4. Monocyte/macrophage cell line cells with CD68 immunostaining
Figure 5. Cryoglobulinaemic glomerulonephritis. Electron microscope. Intraluminal and subendothelial deposits with microtubular sub-structure.