The application of antiseptic solution for handling tunnelled catheters is recommended in patients undergoing haemodialysis. These routine antiseptic procedures in handling catheters are crucial to avoid complications. We report an outbreak of Serratia marcescens (S. marcescens) bacteraemia in numerous haemodialysis units of the Community of Madrid.
Material and methodsThe first cases of bacteraemia due to S. marcescens were isolated in December 2014. The Preventive Medicine Services were informed of the detection of an atypical pathogen in several patients, suspecting a probable nosocomial outbreak. Information from 4 centres with similar S. marcescens bacteraemia was analysed.
ResultsTwenty-one cases of bacteraemia related to S. marcescens were identified. The mean age of affected patients was 72±10 years. The mean time on haemodialysis of affected patients was 33±13 months (range: 3–83 months), the median time of tunnelled catheter was 22±13 months. In 11 cases the clinical picture was similar, with hypotension and general malaise during the haemodialysis session. Fever was present in a further 7 cases. In 3 cases the presentation was asymptomatic and was detected by blood cultures. All patients had tunnelled catheters (12 patients with catheter in the right jugular vein, 5 in the left jugular, 2 in the right femoral artery and 2 in the left subclavian artery). Gentamicin intravenous doses (1mg/kg) with catheter lock solution with ciprofloxacin post-dialysis were administered for 3 weeks in 6 patients. In 12 patients the treatment was ceftazidime (2g IV) plus catheter lock solution with the same antibiotic, for 2 weeks. Four patients received oral ciprofloxacin for 2 weeks, in one case together with IV vancomycin. The patients were asymptomatic and without new episodes 48h after the treatment. No major complications were observed. The teams informed the health authorities of the situation, which then reported the presence of batches of antiseptic (chlorhexidine 0.05 and 2%) colonised by S. marcescens. Given the routine application of this antiseptic in handling catheters at these units, this was considered the source of contagion and new cases were not observed after the removal of the batches.
ConclusionsThe presence of bacteraemia due to unconventional germs should alert us to a potential outbreak. The application of a solution contaminated by S. marcescens in haemodialysis catheters was the source of bacteraemia. The intravenous antibiotic treatment and the catheter lock solution allowed an excellent survival of patients and catheters.
La aplicación de una solución antiséptica previa al uso de los catéteres tunelizados es una práctica recomendada. Estas medidas habituales en la manipulación de los catéteres para hemodiálisis son cruciales para evitar complicaciones. Presentamos un brote de infección por Serratia marcescens (S. marcescens) en varias unidades de hemodiálisis de la Comunidad Autónoma de Madrid.
Material y métodosLos primeros casos de bacteriemia por S. marcescens fueron aislados en diciembre de 2014. La detección de un germen infrecuente en varios pacientes se puso en conocimiento de los Servicios de Medicina Preventiva por sospecha de probable brote nosocomial. Se recogieron datos de 4 centros donde se detectaron episodios de bacteriemias similares por S. marcescens.
ResultadosFueron detectados un total de 21 casos de bacteriemia por S. marcescens. La edad media de los pacientes era de 72±10 años. El tiempo medio en hemodiálisis de los pacientes afectados era de 33±13 meses (rango: 3–83), el tiempo medio del catéter tunelizado era de 22±13 meses. En 11 casos el cuadro clínico fue semejante, caracterizado por hipotensión y malestar general durante la sesión de hemodiálisis. En otros 7 pacientes se asoció fiebre. En 3 casos la forma de presentación fue asintomática y se detectó por hemocultivos. Todos eran portadores de catéteres tunelizados (12 pacientes con catéter en la vena yugular derecha, 5 en la yugular izquierda, 2en la femoral derecha y 2 en la subclavia izquierda). El tratamiento que se aplicó en 6 casos fue gentamicina posdiálisis intravenosa (1mg/kg) más sellado del catéter con solución de ciprofloxacino durante 3 semanas. En 12 pacientes el tratamiento fue ceftazidima 2g iv más sellado de catéter con el mismo antibiótico durante 2semanas. Cuatro pacientes recibieron dosis de ciprofloxacino oral, en un caso se asoció a vancomicina iv, durante 2semanas. A las 48h de iniciar el tratamiento, los pacientes quedaron asintomáticos y no presentaron nuevos episodios. No se observó ninguna complicación mayor. Esta situación fue comunicada por los equipos a las autoridades sanitarias. Posteriormente, se notificó la presencia de lotes de antiséptico de clorhexidina acuosa al 0,05 y 2% colonizados por S. marcescens. Dada la aplicación de forma rutinaria del antiséptico en el manejo de los catéteres en estas unidades, este fue considerado el foco de contagio. Tras la retirada de los lotes no acontecieron nuevos casos.
ConclusionesLas bacteriemias por gérmenes no convencionales deben ponernos sobre aviso para investigar posibles brotes. La aplicación de una solución contaminada por S. marcescens en los catéteres en hemodiálisis fue la vía de bacteriemia. El tratamiento antibiótico intravenoso y el sellado de los catéteres permitió una excelente supervivencia tanto de los pacientes como de los catéteres.
Venous catheters are the alternative for patients who do not have an arteriovenous fistula or functioning prosthesis for renal replacement therapy with haemodialysis. Although the design of the current tunnelled catheters (TCs) has improved, they continue to present higher morbidity and mortality and complication rates than other vascular accesses.1–3 Infections are the main problem, with a high risk of bacteraemia, which determines the life expectancy of patients on renal replacement therapy.4 Prophylaxis measures for handling the catheters are crucial for preventing this type of complication. Applying an aseptic solution for TC handling is a recommended practice for decreasing the risks in patients with this type of catheter.5,6 The most common causative agent for catheter-associated bacteraemia is Staphylococcus aureus, with a high associated comorbidity. While other germs are more unusual, secondary bacteraemia with less conventional germs can also be observed.7–9 We present an unusual outbreak of Serratia marcescens (S. marcescens) bacteraemia in patients with TCs for haemodialysis in 4 hospitals in the Autonomous Community of Madrid.
Material and methodsThe study was conducted at 4 sites where cases of S. marcescens bacteraemia were identified in patients with TCs for haemodialysis. On 17 December 2014, after identifying 2 patients with TCs with positive blood cultures for an uncommon germ (S. marcescens), prevention mechanisms were activated because of the possibility of a nosocomial outbreak. The entire haemodialysis unit, the staff, and the possible sites of infection were investigated, starting with using blood cultures to monitor the at-risk patients, those with catheters, prostheses, those using the button-hole technique. Cultures were taken from the lines, dialysis machines, and the aseptic solutions applied per protocol in the units. A retrospective, multi-centre, descriptive study was conducted of all the cases identified from the first event until the outcome was considered over. The objective was to identified the number affected, the patient characteristics, the treatment received, and the course. A case was considered any patient with S. marcescens identified by blood culture with a TC for haemodialysis, whether or not there were associated symptoms. No patients who were not on renal replacement therapy were included. The 4 sites that conducted a joint analysis along with the measures applied are shown in Table 1. The sites were independent, and the treatment regimens were personalised in each hospital. Each site had its own Nephrology and Preventive Medicine section. To establish whether it was the same strain of S. marcescens, genotyping was performed using pulsed-field gel electrophoresis: the blood cultures and the samples from the contaminated solutions had to coincide.
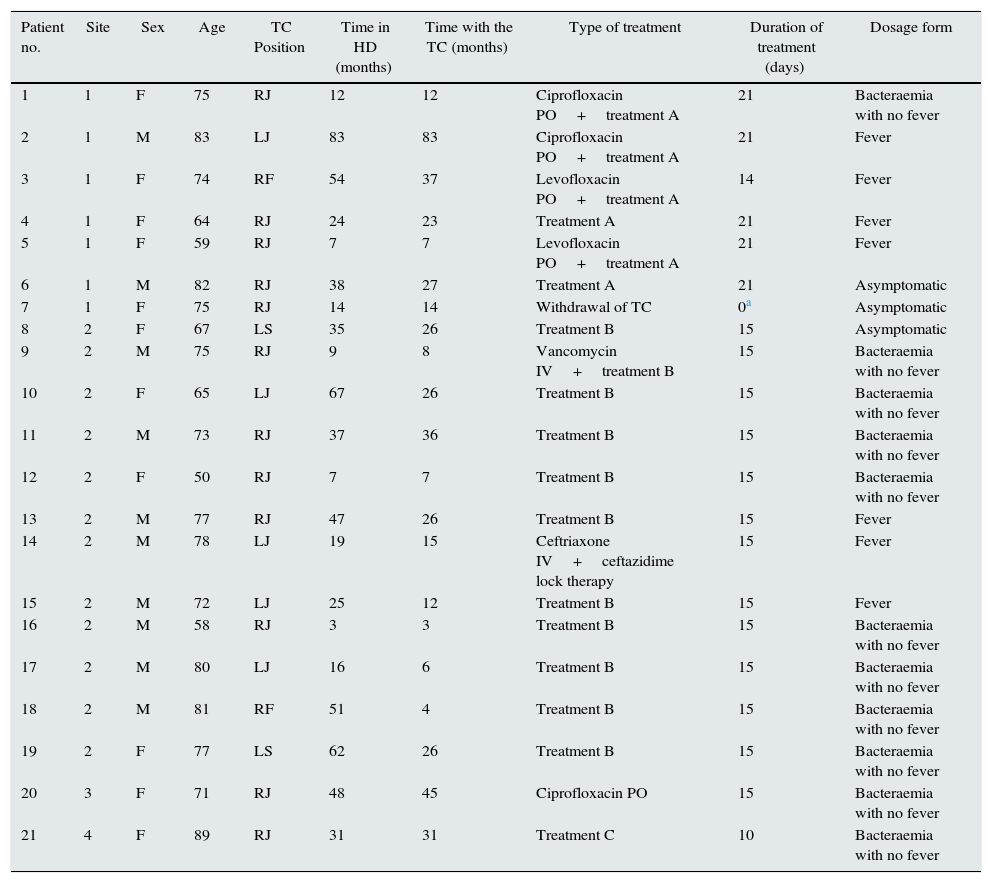
Patient characteristics.
| Patient no. | Site | Sex | Age | TC Position | Time in HD (months) | Time with the TC (months) | Type of treatment | Duration of treatment (days) | Dosage form |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 1 | F | 75 | RJ | 12 | 12 | Ciprofloxacin PO+treatment A | 21 | Bacteraemia with no fever |
| 2 | 1 | M | 83 | LJ | 83 | 83 | Ciprofloxacin PO+treatment A | 21 | Fever |
| 3 | 1 | F | 74 | RF | 54 | 37 | Levofloxacin PO+treatment A | 14 | Fever |
| 4 | 1 | F | 64 | RJ | 24 | 23 | Treatment A | 21 | Fever |
| 5 | 1 | F | 59 | RJ | 7 | 7 | Levofloxacin PO+treatment A | 21 | Fever |
| 6 | 1 | M | 82 | RJ | 38 | 27 | Treatment A | 21 | Asymptomatic |
| 7 | 1 | F | 75 | RJ | 14 | 14 | Withdrawal of TC | 0a | Asymptomatic |
| 8 | 2 | F | 67 | LS | 35 | 26 | Treatment B | 15 | Asymptomatic |
| 9 | 2 | M | 75 | RJ | 9 | 8 | Vancomycin IV+treatment B | 15 | Bacteraemia with no fever |
| 10 | 2 | F | 65 | LJ | 67 | 26 | Treatment B | 15 | Bacteraemia with no fever |
| 11 | 2 | M | 73 | RJ | 37 | 36 | Treatment B | 15 | Bacteraemia with no fever |
| 12 | 2 | F | 50 | RJ | 7 | 7 | Treatment B | 15 | Bacteraemia with no fever |
| 13 | 2 | M | 77 | RJ | 47 | 26 | Treatment B | 15 | Fever |
| 14 | 2 | M | 78 | LJ | 19 | 15 | Ceftriaxone IV+ceftazidime lock therapy | 15 | Fever |
| 15 | 2 | M | 72 | LJ | 25 | 12 | Treatment B | 15 | Fever |
| 16 | 2 | M | 58 | RJ | 3 | 3 | Treatment B | 15 | Bacteraemia with no fever |
| 17 | 2 | M | 80 | LJ | 16 | 6 | Treatment B | 15 | Bacteraemia with no fever |
| 18 | 2 | M | 81 | RF | 51 | 4 | Treatment B | 15 | Bacteraemia with no fever |
| 19 | 2 | F | 77 | LS | 62 | 26 | Treatment B | 15 | Bacteraemia with no fever |
| 20 | 3 | F | 71 | RJ | 48 | 45 | Ciprofloxacin PO | 15 | Bacteraemia with no fever |
| 21 | 4 | F | 89 | RJ | 31 | 31 | Treatment C | 10 | Bacteraemia with no fever |
Site 1: Hospital Univ. del Henares; Site 2: Hospital Univ. Príncipe de Asturias; Site 3: Hospital Univ. Infanta Leonor; Site 4: Hospital Univ. Infanta Sofía; F: Female; HD: haemodialysis; IV: intravenous; LJ: left jugular; LS: left subclavian; M: male; PO: oral; RF: right femoral; RJ: right jugular; TC: tunnelled catheter; Treatment A: Gentamicin IV (1mg/kg/body weight)+ciprofloxacin lock therapy; Treatment B: ceftazidime 2g IV+ceftazidime lock therapy; Treatment C: ciprofloxacin PO+vancomycin IV+gentamicin lock therapy.
Statistical analysis: The results are expressed as the mean and standard deviation. The median and range are included when required by the series.
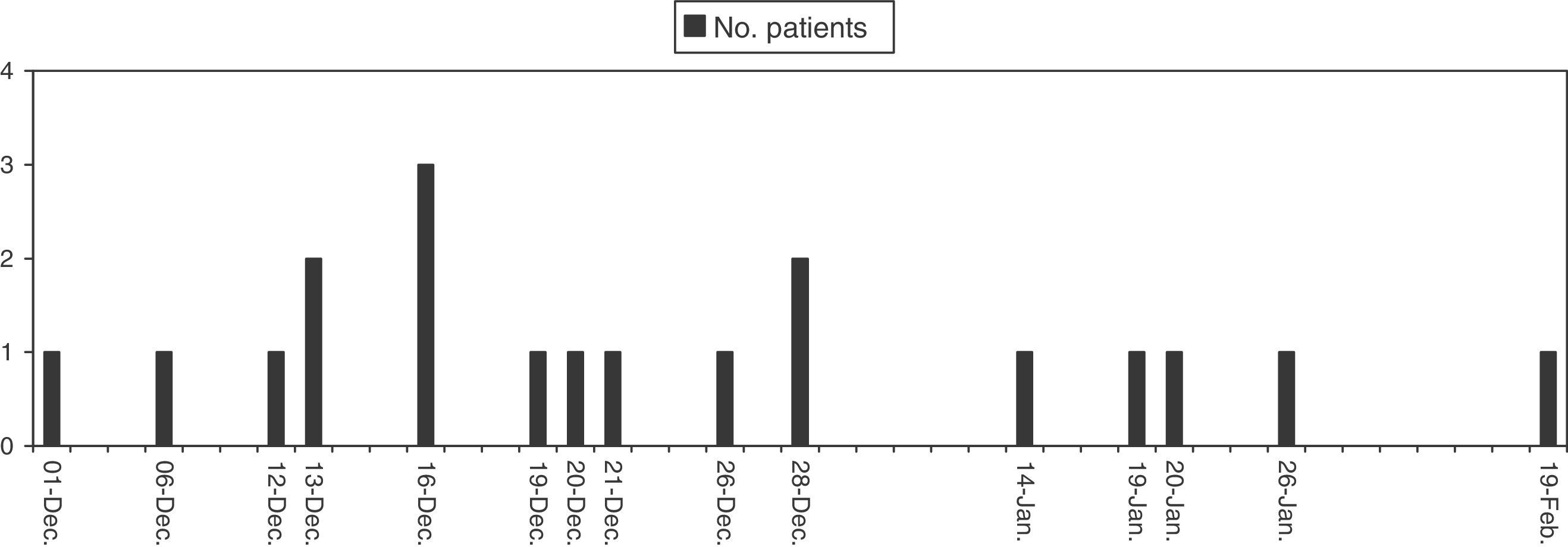
FindingsThe first case confirmed by blood culture was on December 6th 2014. The outbreak was suspected on December 17th given the presence of 2 other patients with positive blood cultures for the same germ. The outbreak ended on 19 February 2015, the date of the last positive case. Once the outbreak was over, 21 total patients were identified, all with positive blood cultures for S. marcescens and using TCs. Once the first cases were confirmed in different haemodialysis units, it was reported to the heads of Preventative Medicine at each site. During this period, an epidemiological study of the potential sources of infection was conducted according to each site's protocol, including the healthcare staff, materials, and machinery. Preventative control measures were also ramped up. Lastly, 11 male and 10 female patients were affected, with a mean age of 72±10 years. The mean time on haemodialysis of the affected patients was 33±13 months (range: 3–83) and the mean time since the catheter implantation was 22±13 months. The patients did not all coincide in the shifts, dialysis site, or the staff who cared for them. The most common presentation was the onset of hypotension, general discomfort, and shivering, with no fever associated with the bacteraemia in 11 cases, during the dialysis session. Temperature over 38°C was recorded in 7 cases. Three (3) cases whose were diagnosed via positive cultures were asymptomatic. The blood cultures were extracted from the lines during the haemodialysis session, in both the symptomatic and asymptomatic patients. The distribution by site and TC location are shown in Table 1. The treatment regimen was different at the 2 sites with the most patients affected. One used a treatment with ceftazidime IV (2g) after dialysis and antibiotic lock therapy with a solution of the same antibiotic (1ml of 500mg ceftazidime in 50 cc of saline solution, with a heparin solution until completing the catheter branches) for 2 weeks (in 11 patients), after confirming sensitivity. Another site used a regimen with gentamicin IV at a dose of 1mg/kg/body weight after dialysis and antibiotic lock therapy using a solution of ciprofloxacin (3ml of antibiotic [vial 200mg/100ml]+3 cc heparin 5%) for 3 weeks, after verifying sensitivity via antibiogram. Three (3) cases were given oral quinolone given the rareness of the infection, 2 cases also received vancomycin IV (1g after dialysis), one patient received oral ciprofloxacin exclusively, and another ceftriaxone IV (2g after dialysis) along with a ceftazidime lock therapy. The attack rate in the sites with the most cases described was 36.8% (7 patients affected out of 19 with TC catheters) and 46.15% (12 S. marcescens infections in 26 patients with TCs). No patients with prostheses or using the button-hole technique presented bacteraemia and their blood culture screens were negative.
Once the risk prevention measures were taken, the potential transmission vectors were reviewed and the healthcare authorities were notified. On December 19th 2014, a report was received regarding the presence of lots of the BohmClorh healthy skin chlorhexidine 2% aqueous solution (250 cc, lots I-33, I-34, and I-35) antiseptic colonised by S. marcescens. A few weeks later, the prohibition on using this solution was expanded to the 0.05% lots. Given that these formulations are routinely applied when handling catheters in these hospitals, this contaminated chlorhexidine was deemed the source of infection. After withdrawing the compromised lots, both the alcoholic and aqueous solution, no new cases were reported. The last recorded case was in February 2015. The timeline of the cases is shown in Fig. 1. Sites 3 and 4 presented one isolated episode. At site 1, after the first notification all chlorhexidine solution lots were withdrawn; at site 2 only the 2% lots were withdrawn after the first recommendation and later the 0.05% lots. To establish whether it was the same strain of S. marcescens, genotyping was performed: the blood cultures and the chlorhexidine sample from of the withdrawn lots coincided. The course was favourable in all cases, with no recurring fever, and none of the TCs needed to be removed because of the infection. The only TC removed was scheduled, since the patient recovered residual kidney function. The positive blood culture was detected a posteriori in this case, during the general unit screening. Given the absence of symptoms and that the focal point was removed, no associated antibiotic treatment was started. No patients died due to a complication secondary to the infection.
DiscussionS. marcescens is a gram-negative bacilli included in the same Enterobacteriaceae family as Klebsiella, Proteus or Escherichia. It is a significant cause of nosocomial infections such as bacteraemia, pneumonia, and urinary tract infections. It commonly affects patients admitted to the ICU and in neonatal units.10–12 Nosocomial outbreaks in adults are commonly related to colonisation of the respiratory and urinary tracts. It has the ability to colonise the gastrointestinal tract, skin, and inorganic treatment vehicles, as well as to survive in disinfecting substances. Its presence in intensive care units has been described, and although there are descriptions of outbreaks more than 20 years ago in haemodialysis, finding it in dialysis units is rare.13,14 In a paper published in 1991, the colonisation of the dialysers used at that time was considered the source of the outbreak.15 Presently this possibility is very low with the current control and sterilisation methods.
Bacteraemia-associated morbidity and mortality secondary to catheter infection is high, and therefore the care measures for TCs are extreme in haemodialysis units.2,4 It is well known that the contamination rates were reduced in the equipment involved, with good training and periodic retraining; with special attention to hand washing, as different papers have made it clear.16,17 Nevertheless, despite these measures, bacteraemia occurs and accounts for one of the main causes of death in haemodialysis patients. Applying antiseptic solutions prior to handling the TCs is an accepted practice for decreasing the risks of infection.5,18 The high attack rate and the onset of cases in a short period of time at several sites at the same time suggested the presence of a common vehicle. Although all sites applied conventional prevention measures, the fact that the source of contamination was the antiseptic solution used resulted in a high infection rate. Initially, the withdrawal notice was only associated with a chlorhexidine concentration, although it was later extended to all concentrations, given the common origin. This fact is likely the one that led to the outbreak being prolonged. Although all concentrations in the haemodialysis unit were removed at site 1, at site 2 other formulations were kept, according to the recommendations from the healthcare authorities, until the definitive indication to completely withdraw all the dosage forms from the same brand.
In turn, only the patients with TCs were affected, with no bacteraemia being detected in other patients who were also potentially at risk, such as the patients with PTFE prostheses or using the button-hole technique. This makes it clear that the TC patients had a higher exposure to the contaminated solutions.
The most commonly implicated germ in TC-associated bacteraemia is Staphylococcus aureus, although bacteraemia can also be secondary to other gram-positive or gram-negative bacteria, and even of fungal origin.7 In general, for any secondary bacteraemia in catheters, its removal is indicated as the main measure.19,20 Nevertheless, in haemodialysis patients with TCs, pharmacological treatment is acceptable if no severity criteria are met in order to avoid removing the TC, given its vital condition as a vascular access.21 A situation of severe sepsis, haemodynamic instability, presence of infection elsewhere, evidence of complicated tunnel-associated infection, persistent fever for 48–72h after starting antibiotic therapy or finding infection by Pseudomonas, Candida, or other fungal infections, as well as detecting multi-resistant pathogens or resistant Staphylococcus aureus are criteria for removing a colonised TC.22 In our series, the patients did not meet the severity criteria and pharmacological treatment was used. TC maintenance is a reasonable treatment option if the bacteraemia is not accompanied by severity criteria, as proposed by some guidelines. In these conditions, attempting IV antibiotic therapy for at least 2 weeks is acceptable.23 This treatment should include, as some studies have previously demonstrated, along with systemic antibiotics (oral or IV), TC antibiotic lock therapy.21,24
It is known that the presence of a biofilm in the catheter can act as a reservoir; therefore, the treatment should include this antibiotic lock therapy.25 In our series, the treatment was established with an IV regimen and catheter lock therapy based on the antibiogram, applying two different formulations that showed similar results. Both the ceftazidime and the gentamicin were effective with gram-negative bacteria, and although there is more experience with gentamicin in dialysis, it can cause more side effects.26,27 Although the antibiotic therapy regimens are usually advised for 2 weeks of treatment, site 1 opted to lengthen it to 3 weeks given the uncertainty of the course with an atypical germ.22,24 In our series, the course was favourable, without requiring the TC to be removed and with no significant associated complications. The early treatment and practice of using lock therapy probably enabled this outcome, once the source of contamination was removed from the haemodialysis units.
ConclusionsThe appearance of bacteraemia caused by an unconventional germ like S. marcescens should put us on alert in haemodialysis units. Colonisation in aseptic solutions is rare, but it can occur. Therefore it should be a vector to be analysed in these situations. Treatment should be as early as possible and it should include TC antibiotic lock therapy. Removing the catheter may not be necessary if no severity criteria are present. Fast action, collaboration of all the facilities, and applying screening measures are key for interrupting the spread of the outbreak and achieving a favourable course for the infections. In this situation the main risk factor was using a TC. Therefore, as long as it is possible, it would be advisable to insist on reducing the number of TCs in the dialysis units.
Conflicts of interestNone.
Please cite this article as: Merino JL, Bouarich H, Pita S, Martínez P, Bueno B, Caldés S, et al. Brote de bacteriemia por Serratia marcescens en pacientes portadores de catéteres tunelizados en hemodiálisis secundario a colonización de la solución antiséptica. Experiencia en 4 centros. Nefrología. 2016;36:667–673.