Due to the growing number of patients with a renal transplant, their increased life expectancy, and the associated comorbidity, the medical care of such patients in the hospital emergency department continues to increase. There is a large variety of conditions that cause such patients to seek medical attention at the emergency department.1–3 The aim of this study was to determine the factors associated with transplant patients’ attendance at the emergency department in the province of Granada, Spain, to evaluate repeat attendance, and determine the most common reasons for consultation.
Patients and methodsThis was a retrospective observational cohort study of stable renal transplant patients based in the province of Granada over one year, including events in the first 6 months (No.=421, SICATA).
The clinical data included were age, sex, aetiology of CKD, period of time on renal replacement therapy (RRT) and transplant, type of dialysis, number of transplants received, immunosuppressive treatment, clinical cardiovascular disease (CVD), diabetes mellitus, HCV, neoplasia, death, and commencement of RRT in the year studied.
The data for analysis were taken from routine reviews at the transplant outpatient clinic, and comprised urea, creatinine, MDRD, haemoglobin, calcium, phosphorus, cystatin C, homocysteine, CRP, PTH, and albuminuria.
We reviewed the emergency department records in the hospitals of the regional area (province). Information was collected on attendance at emergency department, number of consultations, ethnic origin, reason for attendance, and patient destination after consultation, from two tertiary hospitals (Central-west and Central-east transplant areas), two district hospitals (Southern Management area and North-eastern area) and one “High-Resolution” Hospital (HAR-Guadix).
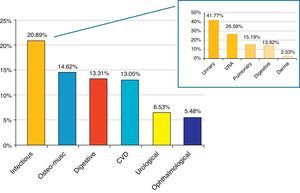
The most common reasons for attendance were grouped as follows: infectious, musculoskeletal, gastrointestinal, cardiovascular, urological, ophthalmological, and accidents.
Statistical analysis was performed with SPSS® v.19, and comprised descriptive analysis, analysis of contingency tables, Pearson's chi-square test and/or Fisher exact test, measures of association, and a logistic regression model.
ResultsOur results show that in transplant patients, 46.56% presented to the emergency department at least once, vs 53.44% who did not use emergency services. Comparing the two groups (Table 1), there were differences according to the presence of diagnosed CVD: 60.26% of patients with CVD attended the emergency department vs 39.74% with CVD who did not attend, P=.004; OR=2.079 (CI, 1.218–3.442).
Comparison of attendance vs no attendance at hospital emergency department.
| Attendance at emergency department | ||
|---|---|---|
| Percentage No (n) | Percentage Yes (n) | |
| Gender of recipient | ||
| Male/female | 59.6/40.4 (134/91) | 58.2/41.8 (114/82) |
| Aetiology of CKD | ||
| Glomerular | 35.4 (79) | 31.3 (61) |
| Interstitial | 15.2 (34) | 12.3 (24) |
| ADPKD | 14.3 (32) | 18.5 (36) |
| Unknown | 11.2 (25) | 11.3 (22) |
| Vascular | 9 (20) | 6.7 (13) |
| Inherited | 4 (9) | 3.6 (7) |
| HTN | 3.1 (7) | 2.6 (5) |
| Diabetes | 0.4 (1) | 5.1 (10) |
| Systemic | 2.7 (6) | 3.1 (6) |
| Other | 4.5 (10) | 5.6 (11) |
| Pretransplant RRT | ||
| Prophylactic | 4.2 (9) | 3.2 (6) |
| HD | 86.6 (187) | 85.5 (159) |
| PD | 9.3 (20) | 11.3 (21) |
| Type of transplant | ||
| Cadaveric | 89.7 (200) | 91.8 (178) |
| Living related | 6.3 (14) | 4.1 (8) |
| Living non-related | 2.7 (6) | 1.5 (3) |
| Asystolic | 1.3 (3) | 2.6 (5) |
| Acute rejection | ||
| Yes/No | 8.4/91.6 (17/186) | 12.8/87.2 (22/150) |
| Relapse of underlying disease | ||
| Yes/No | 1.4/97.8 (3/210) | 2.2/98.6 (4/176) |
| Cardiovascular disease | ||
| Yes/No | 14.6/85.4 (31/181) | 26.3/73.7 (47/132) |
| Diabetes mellitus | ||
| Yes/No | 19.8/80.2 (42/170) | 24/76 (44/139) |
| Death | ||
| Yes/No | 0/100 (0/224) | 2.6/97.4 (5/190) |
| Dialysis started | ||
| Yes/No | 0/100 (0/219) | 1/99 (2/192) |
The estimated glomerular filtration rate using MDRD was significantly lower in the group of patients who attended the emergency department than in those who did not attend, 52.39±22.33mL/min vs 60.69±20.49mL/min. There was no significant interaction between CVD and MDRD.
In the repeat attendance study (more than one consultation), the only associated factor was age; P=.006, OR=1.031 (CI, 1.009–1.054).
The most common reasons for consultation were infectious, musculoskeletal, gastrointestinal, cardiovascular, urological, ophthalmological, and accidents. Within the infectious causes, the most common site was urinary, followed by upper respiratory tract, pulmonary, gastrointestinal, and dermatological (Fig. 1).
Fifty one percent of patients in the first post-transplant year generated 28 consultations with a different distribution: infectious, 32.14%; urological, 21.42%; and cardiovascular, 14.28%.
Regarding location, 71.02% of consultations occurred in the transplant centre. Patients came directly from home in 89.03% of cases. Patient destination was discharge to home in 77.02% of cases.
Patients referred to the transplant centre from non-transplant hospitals came from: Central-eastern area, 5.88%; Southern Management area, 21.21%; North-eastern area, 6.25%; HAR (Guadix), 25.92%. Of these referrals, 35.29% were discharged, 41.18% were admitted to the renal department, and 23.53% were admitted to other departments. The main reason for referral was infection (41.17%).
DiscussionThis study shows that less than half of the transplant population attended a hospital emergency department in the Granada province in one year. For the same year, in the general population, the percentage attendance at the emergency department of provincial tertiary hospitals was 51%, suggesting no increased demand on services from our study population. Emergency department attendance was associated with diagnosed CVD as a risk factor and renal function as a protective factor. Repeated emergency department attendance was associated with increased age of recipient patients.
There was a wide variety of reasons for consultation and diagnoses, the most common reason for consultation being infection,4 followed by musculoskeletal causes.5 In the first post-transplant year, infection remained the main reason for consultation, followed by urological causes. This difference could be attributed to the effect of immunosuppression in the first year, thereafter urological complications in post-transplant patients being more significant.1,6
In the comparison between percentage of transplant patients and percentage of the general population referred from hospitals without a renal unit to a hospital with a transplant unit, there was a larger number of referrals from the transplant population to the reference hospital compared with the general population: HAR (25.92% vs 4.6%) and North-eastern area (6.25% vs 0.84%).
Unterman et al.7 performed a retrospective descriptive analysis of visits to the emergency department of 1251 patients with solid organ transplants from 2000 to 2004 in Illinois; 378 were renal transplant recipients. The percentage attending the emergency department was higher than in our population (70.1% vs 46.56%), as was the percentage of hospital admissions (56% vs 21.67%). This difference could be related to our more frequent scheduled outpatient review system, which may result in a lower demand on hospital emergency departments from these patients and less need for admission from this unit. In such study the most common diagnosis was infection/fever, which was consistent with our results. The second most common diagnosis, depending on how recent was the transplantation, was, dehydration and non-infectious gastrointestinal/genitourinary disease (early post-transplant) and cardiopulmonary and musculoskeletal disease (late post-transplant). In the present study, there was a wide range of period elapsed since transplantation (mean 109 months), which could explain why musculoskeletal causes were the second most common reason for consultation. Tokalak et al.8 described a wide variety of reasons for consultation in the emergency department in 78 patients with recent renal transplant; fever was the most common reason, and the rate of hospital admission was higher than that of our study.
In conclusion, in the renal transplant population of the Granada province, there was a high emergency department attendance rate, similar to or even somewhat lower than that of the general population. The factors associated with attendance were CVD (risk factor) and renal function deterioration (protective factor). Information on the most common reasons for emergency department attendance and the care protocol in a determined geographical area could lead to improved coordination between emergency departments and renal units. Likewise, it may help to optimize the referral route between hospitals in regional areas and the transplant hospital.
FundingThis study was cofinanced by REDinREN (Renal Research Network).
Please cite this article as: Ruiz-Fuentes MC, Vargas-Rivas J, de Gracia-Guindo C, Ruiz-Fuentes N, de Teresa-Alguacil J, Osorio-Moratalla JM, et al. El paciente trasplantado renal en urgencias. Nefrologia. 2015;35:591–593.