A 52-year-old female patient with a history of high blood pressure, left nephrectomy in 1990 due to hydronephrosis secondary to lithiasis, and chronic kidney disease, who started haemodialysis in 2008 non compliant with the treatment. The patient had severe secondary hyperparathyroidism refractory to medical treatment. She developed brown bone tumour while waiting for a parathyroidectomy. Total parathyroidectomy was performed in July 2013.
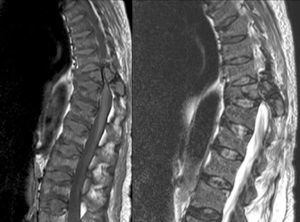
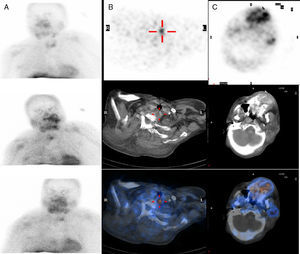
In January 2014, she was hospitalised for thoracolumbar pain and lower limb paresis. MRI findings were consistent with a 3.7cm brown tumour in vertebral posterior elements in D10 and a smaller tumour in L2. She also had widespread bone disease with chronic fractures and “rugger jersey” sclerosis (Figs. 1 and 2). Persistent severe hyperparathyroidism was observed in lab tests, and so a new imaging study (ECHO and parathyroid scintigraphy) was requested which confirmed the existence of a fifth retrotracheal left paratiroidea gland (Fig. 3).
Thoracolumbar MRI: sagittal plane of MRI in T1 and T2 of the thoracolumbar spine showing a focal lesion in the left posterior elements of the D10 vertebra involving the pedicle, pars, and lamina. The lesion has an expansive character and is surrounded by a thin, newly-formed shell of periosteal bone with a maximum diameter of 3.7cm, presenting soft tissue components and invading the spinal canal, resulting in clear cord compression with narrowing. An intermediate signal is observed in all pulse sequences and we believe it is consistent with a brown tumour (osteoclastoma).1,2
Parathyroid scintigraphy: (A) Planar imaging of head and chest in the anterior projection following administration of 20mCi of 99mTc-MIBI (methoxy isobutyl isonitrile) at 20, 60, and 180min, showing increased uptake of the radiotracer next to the lower half of the left thyroid lobe, which was sustained during the long period of examination. (B) Selected axial section of the SPECT/CT image at 60min, SPECT/CT fusion showing a focus of increased uptake of retrotracheal location somewhat to the left, up to D1. Findings are consistent with parathyroid adenoma or hyperplasia. (C) Selected axial section of the SPECT-CT image, based on skull and jaw region. The SPECT, CT, and fusion images show a large area of irregular increased uptake of radiotracer in left maxilla, appearing as expansive osteolytic lesion in the CT scan and consistent with a brown tumour.3
Surgery included complete hemivertebrectomy, tumour dissection and bilateral transpedicular instrumentation of T8-11, with implants of titanium prosthesis. After surgery spinal cord was not longer compressed resulting in an immediate clinical and electrophysiological improvement.
Excision of the left retrotracheal parathyroid gland was conducted following recovery from surgery. The patient developed hungry bone syndrome and the size of the maxillary brown tumour was significantly reduced.
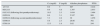
The outcome of biochemical parameters related to severe secondary hyperparathyroidism is summarised in Table 1.
Evolution of biochemical parameters of bone and mineral metabolism.
| Ca (mg/dl) | P (mg/dl) | Alkaline phosphatase | PTHi | |
|---|---|---|---|---|
| 1/17/13 | 9.9 | 5 | 907 | 3.418 |
| 06/12/13 | 9.9 | 4.8 | 1.397 | 2.933 |
| 01/13/13 (following first parathyroidectomy) | 10.3 | 2.3 | 1.610 | 1.464 |
| 03/03/14 | 8.6 | 3.1 | 2.547 | 908 |
| 03/26/14 (following second parathyroidectomy) | 7.3 | 2.8 | 39 | 1.078 |
| 05/06/14 | 5.9 | 2.3 | 26.06 | 392 |
| 07/01/14 | 13.3 | 1.9 | 3.62 | 244 |
A differential diagnosis should be made between brown tumour and giant cell lesions, fibrous dysplasia, and bone tumours (sarcoma or metastatic carcinoma). Treatment should include the management of hyperparathyroidism in order to reverse skeletal abnormalities. Surgery is indicated for patients with symptoms requiring emergency decompression due to the involvement of adjacent anatomical structures, like in our patient.
Please cite this article as: Rodríguez-Gómez EM, Ruiz-Escolano FJ, Ramos-Font C, Calurano-Casero R, Cruz-Muñoz S, Bernáldez-Domínguez MP. Compresión medular por tumor óseo pardo en paciente en hemodiálisis. Nefrología. 2015;35:594–596.