The SARS-CoV-2 (Covid-19) coronavirus pandemic is evolving very quickly and means a special risk for both immunosuppressed and comorbid patients. Knowledge about this growing infection is also increasing although many uncertainties remain, especially in the kidney transplant population. This manuscript presents a proposal for action with general and specific recommendations to protect and prevent infection in this vulnerable population such as kidney transplant recipients.
La pandemia por coronavirus SARS-CoV-2 (Covid-19) está evolucionando de manera muy rápida y representa un riesgo especial en pacientes inmunodeprimidos y con comorbilidades añadidas. El conocimiento sobre esta infección emergente va también en aumento, si bien, aún sigue habiendo muchas incógnitas, sobre todo en la población con trasplante renal. Este manuscrito presenta una propuesta de actuación con recomendaciones generales y específicas para proteger y prevenir de la infección a esta población tan vulnerable como son los receptores de un trasplante renal.
On December 31, 2019, the Wuhan Health Commission reported about groups of people with pneumonia who were epidemiologically linked to a seafood and live animal market in Wuhan, China.1 The etiology was identified as a new coronavirus, with a supposed zoonotic origin. The virus has been recently named the coronavirus of severe acute respiratory syndrome type 2 (SARS-CoV-2) and the disease has been called Coronavirus Disease 2019 (COVID-19).2
So far, there is uncertainty regarding the transmission capacity of the virus. Recent studies show the presence of a high viral load in the oropharynx at early stages of the disease, which increases the concern about the high risk of infectivity during incubation periods or with only mild symptoms.3 The average incubation period has been estimated to be 5–6 days, with a range of 1–14 days. In over 80% of cases the symptoms of the disease are mild (fever, cough, expectoration, general malaise), while approximately 20% may have serious clinical manifestations (pneumonia and other clinical complications) that require hospital admission. Pregnant women, newborns, the elderly, immunocompromised and patients with comorbidities such as diabetes mellitus, hypertension and cardiovascular disease, are more to be infected by COVID-19, and they are more likely to suffer severe illness that often requires to be admitted to ICU. The impact of COVID-19 on chronic kidney disease has been scantily reported.4 Current mortality rate in China is 3.9% of the cases confirmed by the lab, which is very similar to that of Spain 3.7% (data as of March 16, 2020).5 However, it is still premature to establish the true mortality rate in our country.
General considerations in kidney transplant patientsIn kidney transplant recipients, due to their status of immunosuppression, the clinical manifestations, treatment, and prognosis of COVID-19 pneumonia may differ from the general population, hence the importance of early diagnosis by SARS-CoV-2 screening, in those cases where the infection is suspected. In the general population, lymphopenia has been observed in up to 63% of patients,6 but many kidney transplant recipients have drug-induced lymphopenia, therefore, this finding does not help the diagnosis. Therefore, special attention should be paid to this type of immunosuppressed patients, evaluating the early detection of this infection by appropriate diagnostic test and the admission to the hospital in case of infection.
The first case of COVID-19 pneumonia in a kidney transplant recipient has been published recently.7 The clinical features (symptoms, laboratory tests and chest CT scan) were similar to non-transplanted patients with COVID-19.
There have not been published relevant reports on the progress of this disease in the renal transplant population. Most of the transplant centers in Spain already have cases of kidney transplant patients affected by COVID-19 that have not been published. Therefore, it is essential the collaboration between countries in the preparation of national and European registries to learn with detail the epidemiological characteristics of this infection in patients with solid organ transplants, including kidney transplantation.
To our knowledge, COVID-19 has not been described in donor-recipient transmission of solid organ transplants. However, related viruses such as the severe acute respiratory syndrome coronavirus (SARS-CoV) and the Middle East respiratory syndrome coronavirus (MERS-CoV) were reported in transplant recipients during previous outbreaks of these viruses.8,9
Based on experiences with previous coronaviruses, it is known that an transplant recipient exposed to the virus would become infected in a high percentage of cases; however, less is known about the risk of donor-recipient transmission. The possibility of a donor-derived infection may be influenced by exposure of the donor, the infectivity of individuals during the incubation period and by asymptomatic people. The extent and duration of viremia and the viability of the virus within specific blood or organ compartments would also affect the risk of donor transmission. Therefore, despite the possible negative consequences, temporary interruption of kidney transplantation may be necessary in areas where the virus is being exposed intensively.10
The current epidemic of COVID-19 in Europe is still in its early stages, and although the acquisition knowledge is increasing rapidly, there are many unknowns for the community in general and particularly for the transplant patients. However, it is imperative to anticipate the potential impact on the transplant population to avoid serious consequences. The recommendations may change as we learn more about the infection.
In order to acquire the maximum knowledge to protect the population of kidney transplant recipients, the transplant centers have to develop connections with their local infectious disease specialists and infection prevention professionals. At the same time, it is important to be aware of local and national public health policies to report suspected cases of COVID-19. The Ministry of Health of the Government of Spain periodically publishes a implementation technical report,11 which at this time does not include any special consideration for kidney transplant patients.
The Spanish Nephrology Society (www.senefro.org) and the Spanish Transplant Society (www.setrasplante.org) are conveying the recommendations of measures for prevention and contingency against COVID-19 in kidney patients, including kidney transplant patients.
Specific considerations regarding donation and transplantationThe National Transplant Organization (ONT) in collaboration with the Transplant Coordination in the Autonomies (Regions) with the advice of the Study Group of Infection in the Transplanted patient and in the Immunocompromised Host (GESITRA-IC), recommends preserving the donation and transplant activity for as long as to pandemic allows (http://www.ont.es/) carrying out universal screening of donors and potential organ recipients.
Any transplant program in the affected areas should make a case-by-case assessment when evaluating the convenience of performing a transplant based on:
- 1.
Availability of resources in the ICU/resuscitation areas.
- 2.
Assessment of the risk/benefit of exposing an immunosuppressed patient to the risk of SARS-CoV-2 infection (based on the number of cases and the possibility of admission under ideal isolation conditions) versus the need for transplantation (patient's clinical situation).
- 1.
Maintain adequate hygiene. Wash your hands frequently with soap and water for at least 20s, or with an alcohol-based hand sanitizer (at least 60% alcohol), especially: after using the bathroom, before eating, after blowing, coughing or sneezing and after direct contact with sick people or their surroundings. Avoid touching your eyes, nose and mouth before washing your hands.
- 2.
Cleaning of house surfaces should be done regularly. Clean and disinfect frequently touched objects and surfaces.
- 3.
Avoid contact or maintain a distance of at the least two meters with people with respiratory infection symptoms (fever, cough, generalized sore muscle, sore throat or respiratory difficulty) and do not share personal belongings.
- 4.
During the state of alarm, you must remain at home except for the stipulated exceptions, according to the rules established by the political and health authorities. Phone the kidney transplant clinic at your referral center or the phone numbers authorized by the health authorities.
- 5.
Try to follow a correct diet. Avoid smoking and alcohol. In addition to being harmful to health, these substances weaken the immune system, making the body more vulnerable to infectious diseases.
- 6.
Avoid sharing food and utensils (cutlery, glasses, napkins, handkerchiefs, etc.) and other objects without cleaning them properly.
- 7.
The Centers for Disease Control and Prevention and (CDC): does not recommend to the general population that people who are well to wear a face mask to protect himself from respiratory diseases, including COVID-19. Today, the kidney transplant population must comply with the recommended measures of protection in the general population, especially if they are asymptomatic at home. However, the responsible physicians will recommend the use of a mask on an individual basis, mainly in cases where the patient goes to a health center or other place with agglomeration. People who show symptoms of being infected with SARS-CoV-2 should wear masks to prevent the spread of the disease to others.
- 8.
It would advisable to authorize a sick leave in patients whose profession entails a high risk for infection.
- 9.
To monitoring your kidney transplant through teleconsultation is recommended to reduce the time spent in health centers and minimize the risk of infection.
According to the latest document from the Ministry of Health (COVID-19 Clinical Management Technical Document: Medical Treatment of March 19, 2020), kidney transplant recipient patients with suspected SARS-CoV-2 infection have indication of diagnostic test and assessment of admission if the result is positive, and the initiation of a specific treatment.
All kidney transplant patients with symptoms compatible with COVID-19 are recommended to contact their transplant specialist or primary care physician (preferably by telephone), indicating clearly their chronic diseases and the type of treatment they take regularly. Depending on the symptoms presented, it is recommended:
- •
Mild symptoms (without dyspnea/tachypnea) and temperature <38°C in a kidney receptor with adequate functional reserves: the patient will be asked to contact by phone with phone number that has been designed by the Health Authorities in each Autonomic Community to have the diagnostic test performed and remain at home monitoring symptoms and alarm signs with telephone monitoring by the transplant team every 24–48h.
- •
Moderate/severe symptoms, temperature >38°C or fragile receptor: the patient will be instructed to go to the Hospital Emergency Department to be clinically evaluated.
Currently there is no evidence from controlled clinical trials to recommend a specific treatment for the SARS-CoV-2 coronavirus in the general population in patients with suspected or confirmed COVID-19.12
In the absence of conclusive data on the treatment of this infection in kidney transplant patients, the drugs used to date for the control of this disease in the general population are the following:
Hydroxychloroquine: Usually used for the treatment of malaria and amebiasis. Antiviral activity has been documented in vitro and no data is available in humans but favorable results have been observed. It interferes with the ECA2 receptor and with the intercellular traffic of the virus.
Dose: 400mg every 12h the first 24h, then 200mg every 12h for a total of 10 days. Requires adjustment in dialysis and liver failure.
Chloroquine: alternative to hydroxychloroquine. Lower in vitro activity than hydroxychloroquine.
Dose 500mg every 12h.
Lopinavir/Ritonavir: Combination of protease inhibiting antiretroviral agents. Both are inhibitor is of CYP3A, so should be reduced dosages of calcineurin inhibitors and mTOR inhibitors. Concomitant use with tacrolimus causes a severe increase in immunosuppressant levels far greater than that produced when a single protease inhibitor is used, with a high risk of toxicity.13 It is advisable to suspend the administration of anticalcineurin and to start monitoring levels after 48h.
There is little evidence to support its possible effect on COVID-19 infection.14,15 An ongoing clinical trial (MIRACLE) is looking at the association between Lopinavir and IFN-β for 14 days for the treatment of MERS. Compared to Remdesivir, Lopinavir/Ritonavir has the advantage of being widely available with and acceptably tolerated toxicity profile. It has been suggested to use a triple therapy with Lopinavir/Ritonavir/Ribavirin.16
Dose: 200mg/50mg 2 comp p.o. each 12h up to a maximum of 14 days.
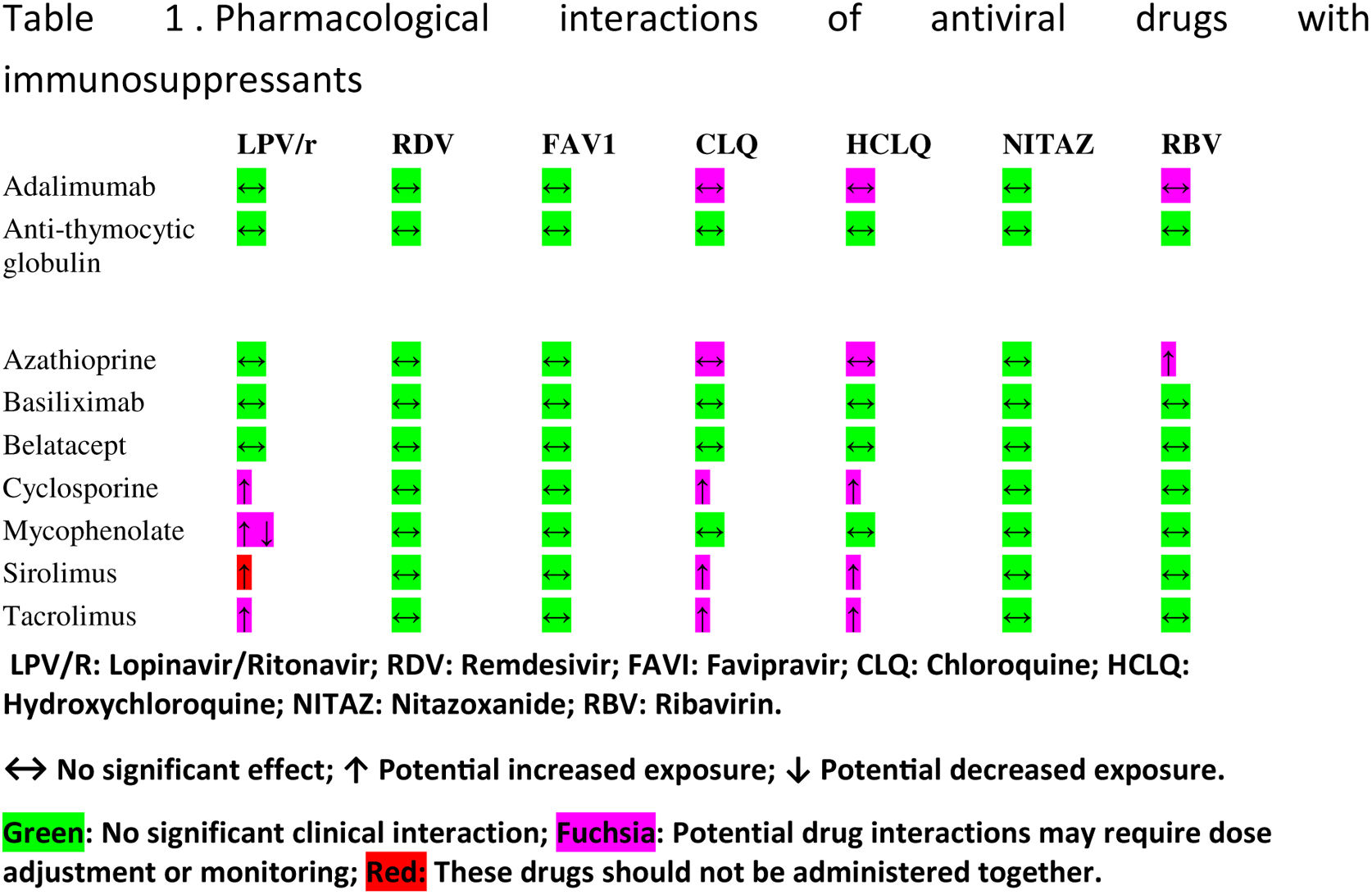
Table 1 describes the interactions of drugs for COVID-19 infection with different immunosuppressants.
Systemic corticosteroids: Not widely recommended. No benefit has been demonstrated in SARS or MERS epidemics. They can increase the spread of the virus. Consider and weight it use in cases of adult respiratory distress syndrome (ARDS), septic shock, encephalitis, hemophagocytic syndrome and in case of bronchospasm with wheezing.
Interferon-β1b (INF-β1b): Dose: 0.25mg sc. every 48h for 14 days (total 7 doses). Risk of acute rejection due to induction of alloreactivity, therefore its use should be individualized, strictly evaluating the risk-benefit in kidney transplant patients.
Remdesivir: Thus is the prodrug of a nucleotide analog with potent activity in vitro against a broad spectrum of virus RNA, as the virus Marburg, Ebola, MERS-CoV, respiratory syncytial virus, Nipah virus and Hendra virus. Its mode of action is based on the premature termination of viral RNA transcription.17 It is suggested that it helps to reduce viral load and improves respiratory parameters in animals and in vitro models.18 Several clinical trials with this drug are currently underway. It is for compassionate use.
Dose: loading dose in the first day of 200mg/iv followed by a maintenance dose of 100mg/iv per day from day 2 to day 10.
Tocilizumab: it is a humanized monoclonal anti interleukin-6 receptor. It is used in severe cases taking into account the role of IL-6 together with other proinflammatory cytokines in the development of ARDS.
Dose: 8mg/kg (maximum dose 800mg) iv single dose; consider to repeat dose according to clinical response at intervals of at least 8–12h up to a maximum of 3 doses.19
Ascorbic acid: The CITRIS-ALI multicenter trial suggests an improvement in mortality in ARDS.20 However, there is no further evidence supporting this effect.
Intravenous immunoglobulins: They have been used in severe cases but their indication and efficacy must be evaluated. The recommended doses are: 1g/kg/day, 2 days, or 400mg/kg/day, 5 days. Treatment highly questioned, there is no evidence for its use.
Antibiotic treatment: It is used in case of bacterial superinfection. A study has recently been published demonstrating a synergistic effect of the combination of hydroxychloroquine with azithromizine (500mg on the first day, followed by 250mg/d for 4 days).21
Given the possibility of drug interactions, it is recommended to carefully review the therapeutic combinations well before starting any treatment.
Kidney transplant patients frequently receive drugs that block the renin-angiotensin-aldosterone system. It is currently unclear what is the role that these drugs may play in patients with COVID-19 disease. The American Society of Cardiology recommends not stopping these drugs in patients who are taking it.22
Immunosuppressive treatment in patients with SARS-CoV-2 diseaseKidney transplant patients, due to immunosuppression, the immune response have been altered and particularly the T-cell immune response. There is little evidence regarding the minimization or management pattern of immunosuppression, especially in the kidney transplant population infected by COVID-19. There has been a very short period of time since the appearance of COVID-19 with very limited accumulated experience and the insufficient published scientific evidence. To date, only one case of a patient with COVID-19 pneumonia in a kidney transplant recipient has been published, whose clinical manifestations were similar to those of the population not carrying a kidney transplant.7 In this case, the triple immunosuppressive therapy that he had received so far was discontinued (prednisone, mycophenolate mofetil (MMF) and tacrolimus and starting methylprednisolone at a dose of 40mg/day plus nonspecific immunoglobulin). In this patient, fever remitted the fifth day after discontinuation of the treatment. Then, at that moment, tacrolimus was restarted at half the dose, although the radiological signs of pneumonia still persisted. Resolution of the clinical and radiological symptoms with a negative microbiological sample for COVID-19 occurred two weeks after the onset of the clinical symptoms, and the previous dose of tacrolimus and MMF were reintroduced.7
Therefore, given the limited experience accumulated and the high probability of torpid evolution in a short period of time, with the development of multi-organ failure and the need for respiratory support, the immunosuppressive strategy recommended a priori, at least in the most severe cases of kidney transplant patients with COVID-19 pneumonia, should involve the temporary interruption of immunosuppressants and the start of methylprednisolone at low doses between 20 and 40mg/day, to confer the rapid acquisition of the necessary cellular immunity to control the infection and thus prevent vital complications. Low-dose systemic corticosteroids have several beneficial effect due to their immunomodulatory, anti-inflammatory and vascular properties, which confer immunological protection of the renal allograft23; Corticoids produce inhibition of proinflammatory cytokines, reduction of white blood cell traffic and maintenance of integrity and permeability of the endothelium, thus maintaining homeostasis and controlling dysregulation of the immune system.23
In less severe cases, an alternative could be the withdrawal of MMF and the reduction of the dose of calcineurin inhibitors, but so far there are no studies that support this strategy. Given the trophism of the virus by the lung tissue, it seems undesirable to use anti-mTOR drugs, at least in patients with pathology of the lower respiratory tract.
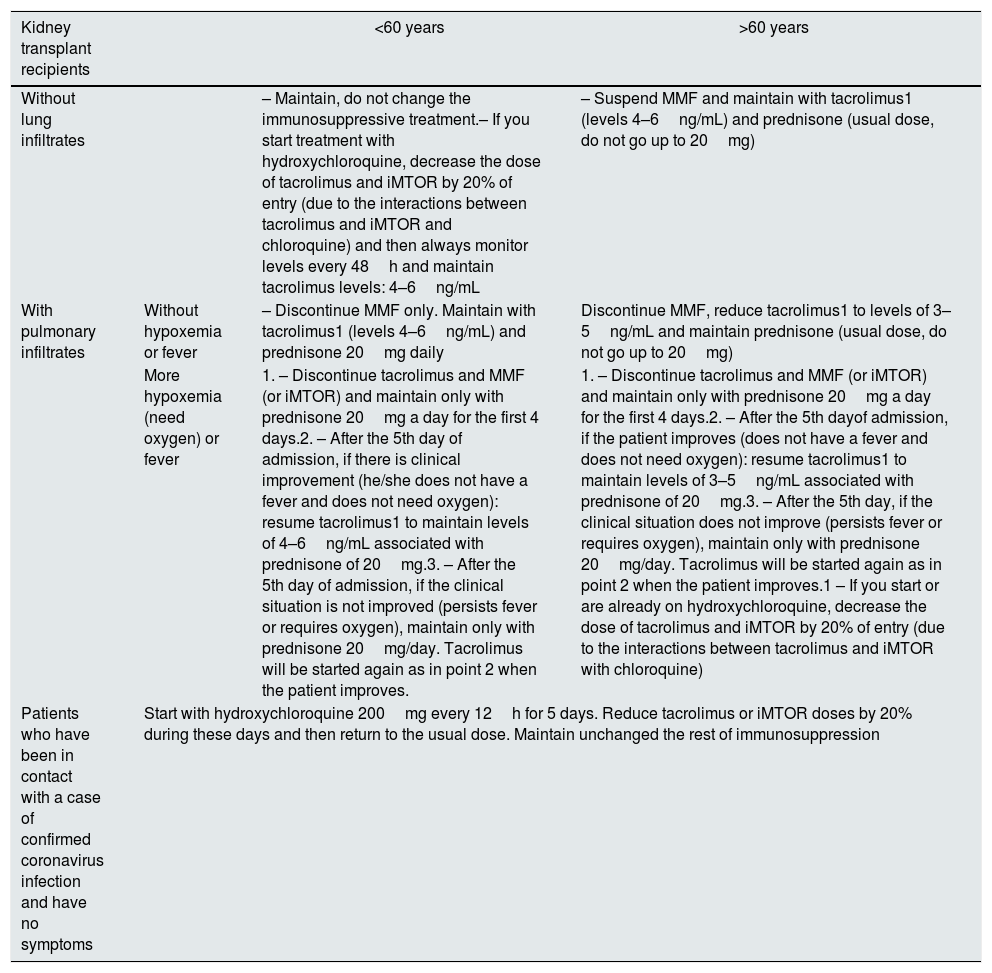
The Spanish group at the Hospital de la Paz has recently communicated its protocol for managing immunosuppressive treatment in patients with Covid-19 infection24 (Table 2).
Immunosuppressive protocol in kidney transplant patients with COVID-19 infection at Hospital La Paz in Madrid.
| Kidney transplant recipients | <60 years | >60 years | |
|---|---|---|---|
| Without lung infiltrates | – Maintain, do not change the immunosuppressive treatment.– If you start treatment with hydroxychloroquine, decrease the dose of tacrolimus and iMTOR by 20% of entry (due to the interactions between tacrolimus and iMTOR and chloroquine) and then always monitor levels every 48h and maintain tacrolimus levels: 4–6ng/mL | – Suspend MMF and maintain with tacrolimus1 (levels 4–6ng/mL) and prednisone (usual dose, do not go up to 20mg) | |
| With pulmonary infiltrates | Without hypoxemia or fever | – Discontinue MMF only. Maintain with tacrolimus1 (levels 4–6ng/mL) and prednisone 20mg daily | Discontinue MMF, reduce tacrolimus1 to levels of 3–5ng/mL and maintain prednisone (usual dose, do not go up to 20mg) |
| More hypoxemia (need oxygen) or fever | 1. – Discontinue tacrolimus and MMF (or iMTOR) and maintain only with prednisone 20mg a day for the first 4 days.2. – After the 5th day of admission, if there is clinical improvement (he/she does not have a fever and does not need oxygen): resume tacrolimus1 to maintain levels of 4–6ng/mL associated with prednisone of 20mg.3. – After the 5th day of admission, if the clinical situation is not improved (persists fever or requires oxygen), maintain only with prednisone 20mg/day. Tacrolimus will be started again as in point 2 when the patient improves. | 1. – Discontinue tacrolimus and MMF (or iMTOR) and maintain only with prednisone 20mg a day for the first 4 days.2. – After the 5th dayof admission, if the patient improves (does not have a fever and does not need oxygen): resume tacrolimus1 to maintain levels of 3–5ng/mL associated with prednisone of 20mg.3. – After the 5th day, if the clinical situation does not improve (persists fever or requires oxygen), maintain only with prednisone 20mg/day. Tacrolimus will be started again as in point 2 when the patient improves.1 – If you start or are already on hydroxychloroquine, decrease the dose of tacrolimus and iMTOR by 20% of entry (due to the interactions between tacrolimus and iMTOR with chloroquine) | |
| Patients who have been in contact with a case of confirmed coronavirus infection and have no symptoms | Start with hydroxychloroquine 200mg every 12h for 5 days. Reduce tacrolimus or iMTOR doses by 20% during these days and then return to the usual dose. Maintain unchanged the rest of immunosuppression | ||
As far as resuming immunosuppressive therapy, it is not clear either when to restart and at what dose, and each case should be evaluated individually. In general, it is reasonable to recommend resuming the calcineurin inhibitor at half dose after obtaining the first microbiological culture negative for COVID-19 or a negative PCR, and if the patient remains asymptomatic, add progressively MMF during the following days.
We need more time and experience to be able to optimize the treatment protocol and the immunosuppressive strategy to be followed in kidney transplant patients with COVID-19 infection.
Key concepts- •
To prevent the transmission in the renal transplant population is essential to comply with the general recommendations, with particular emphasis on measures of self-hygiene.
- •
To minimize the risk of infection, teleconsultation is recommended for the follow-up of patients with a kidney transplant.
- •
It is recommended to preserve the donation and transplant activity to the extent that the pandemic allows it, individualizing in each case depending on the characteristics and epidemiological situation of each health center.
- •
Due to the high probability of torpid evolution, the immunosuppressant strategy recommended in kidney transplant recipients with COVID-19 pneumonia should consist in the reduction, or ultimately, the temporary interruption of immunosuppressants.
This article was funded in part by the Ministry of Economy, Industry to and Competitiveness of Spain, of the ISCIII (PI17/02043), funded by the European Regional Development Fund-ERDF, RETIC (REDinREN RED16/0009/0006; RD16/0009/0021; RD16/0009/0019; RD16/0009/0027; RD16/0009/0032.
Conflict of interestsThe authors have no conflicts of interest to declare.
Please cite this article as: López V, Vázquez T, Alonso-Titos J, Cabello M, Alonso A, Beneyto I, et al. Recomendaciones en el manejo de la pandemia por coronavirus SARS-CoV-2 (Covid-19) en pacientes con trasplante renal. Nefrologia. 2020;40:265–271.