Currently, kidney transplantation is the treatment of choice for patients with kidney disease who require replacement therapy. Dialysis is a necessary step, but not mandatory prior to transplantation. There is the possibility of pre-emptive transplantation or transplantation in pre-dialysis, that is, without previous dialysis. The aim of the present study is to evaluate the result of our experience with a pre-emptive kidney transplant from a deceased donor.
Materials and methodsRetrospective, observational, matched cohort study. We compared 66 pre-emptive with 66 non pre-emptive recipients, who received a first renal graft performed at our centre, matched by age and gender of donors and recipients, time of transplant, immunological risk, immunosuppression and cold ischaemia time.
Early graft loss, incidence of acute rejection, delayed graft function, renal function at 12 and 36 months and graft and recipient survival were assessed in this period.
ResultsThe percentage of recipients who presented early graft loss, delayed graft function and acute rejection was similar in both groups. No differences were observed in their renal function at 12 and 36 months after transplantation, as well as the actuarial survival of patients (p = 0.801) and grafts (p = 0.693) in the studied period. The total calculated cost of the period on dialysis for the control group was 8,033,893.16 euros.
ConclusionsPre-emptive transplantation can yield comparable outcomes to those for post-dialysis kidney transplantation, and results in better quality of life for patients with end-stage kidney disease, as well as a reduced cost.
Actualmente, el trasplante renal es el tratamiento de elección para pacientes con enfermedad renal que requieren terapia de sustitución. La diálisis es un paso necesario, pero no obligatorio, previo al trasplante. Existe la posibilidad del trasplante renal anticipado o en pre-diálisis, es decir, sin diálisis previa. El objetivo del presente estudio es evaluar el resultado de nuestra experiencia en el trasplante renal anticipado con donante cadáver.
Materiales y métodosEstudio observacional retrospectivo de tipo cohortes emparejadas. Seincluyó a 66 receptores de trasplante renal en situación pre-diálisis, frente a un grupo control de 66 pacientes ya en diálisis que recibieron un primer injerto renal, emparejados por edad y sexo de donante y receptor, momento del trasplante, riesgo inmunológico, inmunosupresión y tiempo de isquemia fría. Se evaluó la pérdida precoz del injerto, incidencia de rechazo agudo, función retrasada del injerto, función renal a los 12 y 36 meses y supervivencia de injerto y receptor en ese periodo.
ResultadosEl porcentaje de receptores que presentaron pérdida precoz del injerto, función retrasada del injerto y rechazo agudo fue similar en ambos grupos. Tampoco se observaron diferencias en la función renal a los 12 ni a los 36 meses después del trasplante, ni en lasupervivencia actuarial de pacientes (p = 0,801) e injertos (p = 0,693).
El coste total del tratamiento renal sustitutivo en el grupo control fue: 8033893.16 euros.
ConclusionesEl trasplante renal de donante cadáver ofrece a los pacientes en situación de prediálisis resultados superponibles a los de receptores en diálisis, además de ser económicamente rentable.
Chronic kidney disease (CKD) causes significant morbidity and mortality, especially cardiovascular.1 Its severity is divided into stages from least to most severe2; stage 5 is the situation in which it becomes necessary to adopt a series of strategies of treatment including the initiating of renal replacement therapy which will not only keep the patients alive, but also, at least in part, will maintain quality of life.
As a general rule, patients are initially included in a dialysis program, either haemodialysis or peritoneal dialysis.3 Both treatments are effective to maintain the patient alive; it requires prior surgical procedures, either the placement of an arteriovenous fistula or insertion of a central venous or peritoneal catheter.4,5 Moreover, these replacement treatments are far from effectively compensating for all of the lost kidney functions, therefore we only achieve partial treated hoping, if there are no contraindications, to apply definitive complete treatment.6
At this time, we have one effective and complete treatment for CKD. Kidney transplant is the treatment of choice in most patients with end-stage CKD.7,8 Achieving adequate graft survival requires administering chronic pharmacological immunosuppression, but this also promotes the occurrence of opportunistic infections9 and the incidence of cancer increases.10,11 Nevertheless, it manages to restore the patient's previous health condition, since the transplanted kidney fully replaces the functions lost by the native kidney, therefore the benefit/risk ratio is positive.
Generally, deceased-donor kidney transplantation is considered when the patient is already on renal replacement therapy. Dialysis is generally a necessary, but not obligatory, step before kidney transplantation in patients who are candidates for this procedure. It is possible to have a kidney transplant without prior dialysis, this is known as a pre-emptive, or pre-dialysis kidney transplant: a reality in recipients from living donors,12 although it remains conditional in the case of deceased donors due to the scarcity of organs.7,8,13 In France, pre-emptive deceased-donor kidney transplants have been incentivized in recent years, with an increase from 5.6% to 15.5% between 2007 and 2014, with good outcomes.14
In 2007, our centre started a pre-emptive deceased-donor kidney transplant programme. It should be noted that patients in a pre-dialysis situation only receive a transplant if there is no candidate for transplant in patient on renal replacement therapy.
The objective of this study is to evaluate the results of our experience in pre-emptive, deceased-donor kidney transplantation via a retrospective observational study with matched cohorts.
Materials and methodsThe design of the study was retrospective, observational study with matched cohorts.
Recipients who received a kidney transplant from a brain dead donor at the Hospital General Universitario de Alicante [Alicante General University Hospital] between 2007 and 2016 were included. Two groups were defined: a pre-dialysis group (pre-dialysis patients who received a pre-emptive, deceased-donor transplant) and a control group (patients in renal replacement therapy who received a first transplant from a deceased donor).
Inclusion criteria: All patients in a pre-dialysis situation (pre-dialysis group) who received a kidney transplant between 2007 and 2016 were included and compared with a control group of transplant patients who were already on renal replacement therapy. In the pre-dialysis group, patients selected had a glomerular filtration rate under 15 ml/min (measured by CKD-EPI), an estimated time to onset of dialysis under 6 months, and a post-transplant time greater than one year. Each case in the pre-dialysis group was matched by age and sex of donor and recipient, as well as by transplant date (to select the case for the control group, the time between the two transplants must be less than 7 days).
The immunological status of the recipients was evaluated via donor-recipient compatibility and the preformed antibody level.
The general immunosuppressant regime at the time of the kidney transplant consisted of tacrolimus (initial dose: Prograf® 0.1 mg/kg every 12 h or Advagraf® 0.2 mg/kg per day; subsequent doses were adjusted to maintain a trough concentration of tacrolimus between 8 and 10 ng/mL during the first month and afterwards between 6 and 8 ng/mL), mycophenolate mofetil (500 mg/12 h orally) or mycophenolic acid (360 mg/12 h orally), basiliximab or timoglobulin in high-risk patients and tapered corticosteroids.
The variables evaluated were incidence of early graft loss (before 48 h), acute rejection (sudden alteration in graft function or presence of delayed graft function, with specific histological changes), delayed graft function (need for dialysis in the first week post-transplant), kidney function at 12 and 36 months (serum creatinine level), and graft and patient survival during the same period.
The period of time in the transplant waiting list in each patient group was evaluated.
Adherence to treatment was evaluated in both groups by determination of the variation in the trough tacrolimus concentration (calculated as the mean of the coefficients of variation [CV] of the trough tacrolimus concentration for the individual patients obtained from month 3 through month 24 post-transplant, expressed as a percentage) along with a personal interview conducted at every visit.
The theoretical cost resulting from the care of the patients on dialysis of the control group patients was quantified using as the data source.the study conducted by Arrieta et al.15 The cost per patient according to the corresponding time on dialysis was calculated (months on dialysis multiplied by monthly cost depending on the technique).
Statistical studyThe continuous variables are expressed as the mean and 95% confidence interval, or median and interquartile range (p25–p75), depending on the distribution type. The categorical variables are described as the number of percentage of patients by response category.
The continuous variables were compared between groups with Student's T-test or Mann-Whitney's U test depending on the type of variable distribution. Categorical variables were analysed using Fischer's test.
A survival analysis (Kaplan–Meier) was performed to analyse the percentage of patients and grafts lost during the follow-up period. Both groups were compared using the statistical test (log-rank). The level of significance was set at 0.05. The statistical analysis was performed with the SPSS software, version 24.
ResultsSixty-six (66) recipients were included in the pre-dialysis group, matched with 66 patients in the control group, 51 of them on haemodialysis and 15 on continuous outpatient peritoneal dialysis. The median follow-up (months) in the pre-dialysis and control groups was 54.0 (p25–p75: 24.0–102.0) and 56 (p25–p75: 28.8–108.3), respectively. The time on the waiting list was similar in both groups (median in months: p25–p75; 4 [2–7] vs. 6 [2–11] months; p = 0.100).
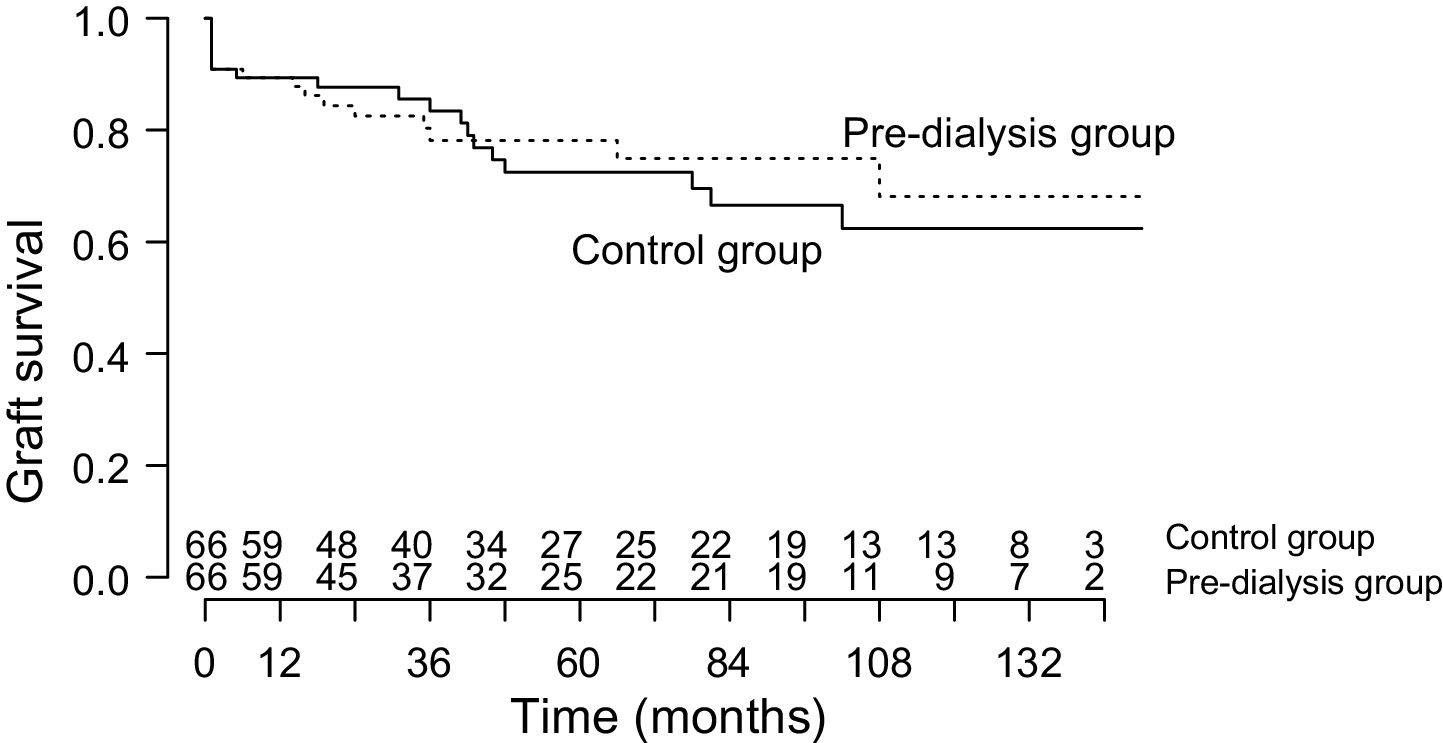
No significant differences were observed between the groups in the age and sex of the donor and recipient, percentage of donors over 60 years, cold ischaemia time, and patients who received induction with thymoglobulin or basiliximab. No significant differences were also observed in the blood group of the recipients or their immunization status. The variability in the trough tacrolimus concentration was similar in both groups, with no lack of adherence detected during the interviews. Table 1 shows the similarity of the variables in both groups.
Demographic data of the patients included in the pre-dialysis group and control group.
| Pre-dialysis group | Control group | p | |
|---|---|---|---|
| Donor age (years), mean (95% CI) | 52.1 (49.1–55.2) | 51.9 (48.4–55.4) | 0.907 |
| Recipient age (years), mean (95% CI) | 51.8 (49.0–54.7) | 51.2 (48.0–54.4) | 0.766 |
| Donor sex (%M/F) | 65.6/36.4 | 56.1/43.9 | 0.375 |
| Recipient sex (%M/F) | 62.1/37.9 | 62.1/37.9 | 0.359 |
| Donor >60 years (%) | 28.8 | 28.8 | 1.000 |
| Cold ischaemia time (hours), mean (95% CI) | 16.7 (15.4–18.0) | 16.9 (15.9–17.9) | 0.826 |
| Thymoglobulin (%) | 43.9 | 34.8 | 0.285 |
| Basiliximab (%) | 24.2 | 18.2 | 0.394 |
| Cp TAC Variability; CV (%), median (p25-p75) | 24.1 (19.5–33.0) | 26.1 (19.1–44.1) | 0.602 |
| Blood group | 0.520 | ||
| A | 56.1 | 50 | |
| B | 9.1 | 9.1 | |
| AB | 10.6 | 6.1 | |
| O | 24.2 | 34.8 | |
| HLA incompatibility | 0.862 | ||
| 4–6 | 54.5 | 51.5 | |
| 0–3 | 45.5 | 48.5 | |
| PRA >50% | 0 | 4.5 | 0.244 |
Cp TAC: trough tacrolimus concentration; CV: coefficient of variation; HLA: histocompatibility antigens; 95% CI: 95% confidence interval; PRA: panel-reactive antibody; M/F: male/female.
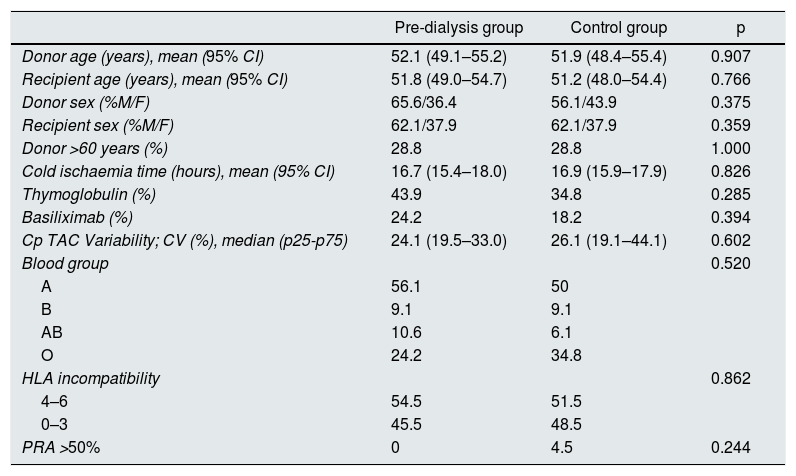
In the pre-dialysis group, the incidence of delayed graft function was similar to the control group (13.6 vs. 15.2%, respectively; p = 0.804). Similarly, no statistically significant differences were found between the two groups for the presence of acute rejection (pre-dialysis group: 12.1% vs. control group: 12.1%; p = 1.000) and early graft loss (pre-dialysis group: 4.5% vs. control group 6%; p = 0.890). Kidney function, evaluated by median serum creatinine, was similar in the pre-dialysis and control groups at one year (1.5 vs. 1.5 mg/dL, respectively; p = 0.568) and 3 years (1.5 vs. 1.4 mg/dL; p = 0.808) (Table 2).
Efficacy and safety variables in the pre-dialysis group and control group (p25–p75: 25th and 75th percentile of the median).
| Pre-dialysis group | Control group | p | |
|---|---|---|---|
| Delayed graft function (%) | 13.6 | 15.2 | 0.804 |
| Acute rejection (%) | 12.1 | 12.1 | 1.000 |
| Early graft loss (%) | 4.5 | 6 | 0.890 |
| Serum creatinine at 12 months, median (p25–p75) mg/dL | 1.5 (1.3–1.7) | 1.5 (1.1–1.8) | 0.568 |
| Serum creatinine at 36 months, median (p25–p75) mg/dL | 1.5 (1.15–1.75) | 1.4 (1.1–2.0) | 0.808 |
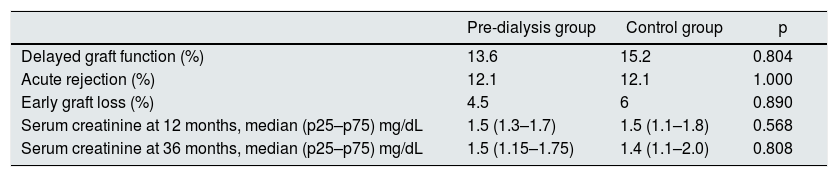
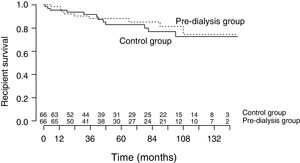
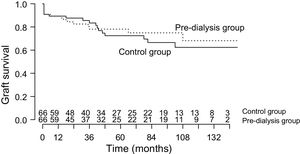
Recipient survival at one and 5 years was 98.5% and 88.3% in the pre-dialysis group and 95.5% and 83.0% in the control group, respectively (Fig. 1). Similarly, graft survival in the pre-dialysis group was 87.8% at one year and 78.2% at 5 years, and in the control group it was 89.4% at one year and 72.5% at 5 years (Fig. 2).
The mean recipient survival time was not different in the pre-dialysis and control groups (126.8 [95% CI: 113.8–139.8] vs. 123.1 [95% CI: 109.7–135.5]) months, respectively; p = 0.730) (Fig. 1). Nor were significant differences in the graft survival time observed between the two groups (pre-dialysis group: 114.6 months [95% CI: 99.1–130.2] vs. control group: 109.3 months [95% CI: 93.7–124.8]; p = 0.693) (Fig. 2).
Taking into account the total time on peritoneal dialysis (334 months) and haemodialysis (1834 months), the total cost of renal replacement therapy in our patients was 8,033,893.16 Euros.
DiscussionThe worldwide experience with pre-emptive, deceased-donor kidney transplant is scarce and under debate.16 Some authors have reported that the time on dialysis before kidney transplantation has a negative impact on its outcome, therefore performing it pre-emptively would be associated with greater graft and recipient survival as compared to patients who remained on dialysis for some time.3,6,8,16–18 Studies by Roake et al.3 and Papalois et al.18 have demonstrated superior survival in pre-dialysis recipients. These results were recently supported by a French multi-centre studied by Prezelin–Reydit in which it was concluded that pre-emptive transplant is associated with a lower risk of graft failure. Nevertheless, this conclusion may be conditional, by having an older dialysis patient group with greater cardiovascular comorbidity and a higher percentage of diabetes mellitus patients than the pre-emptive transplant group, and the fact that the grafts come from older donors.19 Other authors such as Luo et al. recommend this type of transplant, since they improve the patient's quality of life and reduce the economic cost, despite not observing significant differences in terms of recipient or graft survival. However, these authors did show evidence of a decreased rate of acute rejection.20
In our study, like in that by Luo et al.,20 we did not find significant differences in recipient and graft survival rate. Foucher et al. reached the same conclusion in a recent study designed with a control group of more than 500 patients included in the waiting list for at least 6 months before their first dialysis session; in addition, they used an inverse probability score to make the groups mor homogeneous. Nevertheless, the dialysis group had a significantly higher percentage of hyperimmunised patients that were treated with more immunosuppression, which could alter the results.21
The percentage of recipients who experienced acute rejection was similar in both groups, which contrasts with the previously mentioned study by Luo et al. and other studies cited in the literature, which show that a longer time on dialysis increases the risk of rejection.20 The study by Cacciarelli, with 325 kidney transplants, concluded that the incidence of acute rejection was lower in patients who remained on dialysis for a period less than 6 months.17 In contrast, it has been proposed that patients who have not experienced the symptoms of CKD or the morbidity associated with dialysis may be less compliant with the immunosuppressant treatment22, which would lead to a higher incidence of rejection. It is worth to mention that in our group of recipients with pre-emptive transplant, there was no evidence of no compliance in any patient, a similar result was obtained by Papalois, who did not find a higher rate of non-adherence to treatment in patients who received pre-emptive kidney transplant.18
Kidney function 12 and 36 months after the transplant was similar in both groups. However, in other studies, it is made clear that the rate of delayed kidney function is higher in transplant patients who were already on dialysis16; the hypothesis proposed is a higher inflammatory status, as well as an inadequate clearance of certain metabolites in these patients.23
Foucher et al. exhaustively reviewed the ethical justification for transplanting patients in a pre-dialysis situation, which could lead to a longer time on the waiting list for patients on dialysis. In this study, the recipients from the dialysis group were on the waiting list for a mean time of 38 months, significantly longer (p < 0.0001) than the pre-dialysis group, with a mean time of 14 months.21 Our experience is different, since the time on the waiting list in our patients is much shorter and it was not significantly different between the pre-dialysis and dialysis group: 4 and 6 months, respectively; therefore it was consider that, in our case, performing a pre-emptive, deceased-donor transplant does not constitute an ethical dilemma.
The peculiarity of our work is based in the fact that in the analysis of the variables studied, matching were made between pairs of recipients (pre-dialysis situation vs. recipients already on dialysis) who were transplanted with a narrow time margin (under 7 days); whereas in the other referenced series,3,16–18 the group of recipients in a pre-dialysis situation constituted a sub-group of their transplant populations, without matching in terms of transplant time.
Regarding the economicl cost, it is worth to mention that renal replacement therapy (haemodialysis, peritoneal dialysis, and kidney transplant) consume 2.5% of the National Health System's budget and more the 4% of that for Specialised Care. The mean cost of haemodialysis, peritoneal dialysis, and kidney transplant first year is 46,660, 32,432, and 47,136 Euros per patient per year, respectively. However, in subsequent years, the cost of the kidney transplant decreases considerably: 6477 Euros per patient per year; transplant is the technique with the best cost-effectiveness ratio15; therefore we can affirm that it not only prolongs life, but that as far as the economical cost it is also an more advantageous option as compared with long-term dialysis.24 Thus, the time on dialysis for the recipients in the control group entailed a cost which could have been reduced in the case of pre-emptive transplant; this is an objective data point which should be added to the subjective benefit for the patient by avoiding dialysis and, prior to this, inserting the access points.20 However, it is necessary to call attention to the limited availability of deceased-donor kidneys,7,8,16 a fact which would significantly limit the implementation of the proposed strategy.
Deceased-donor kidney transplant offers patients in a pre-dialysis situation outcomes which are at least comparable to those of recipients on dialysis and prevents the morbidity, mortality and psychological impact derived from dialysis, in additional to being economically advantageous.
Conflict of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Franco A, et al. Una aproximación al trasplante renal anticipado de donante cadáver. Estudio de cohortes emparejadas. Nefrologia. 2020;40:32–37.