Background: Chronic Renal Failure (CRF) is a disease that requires determined medications dosages to be adjusted. Objectives: To assess the characteristics of pharmaceutical interventions concerning the dose adjustment of these drugs in patients with CRF who are admitted into hospital. Methods: A 10-month prospective and longitudinal study that calculated the glomerular filtration rate of patients who are brought into the emergency department and had values below 50ml/min/1.73m2. Subsequently, dosage recommendations were provided for the drugs that had not been adapted to the patient’s renal function. Results: The renal functions of 5311 patients were reviewed. One-hundred and eighty-one (3.4%) had a glomerular filtration rate below 50ml/min/1.73m2 and were receiving drugs that needed to be adjusted. 221 interventions were recorded. Reductions in dosages were the more frequent results (65.6%); 65.6% of these recommendations were accepted by the doctor. The antimicrobial group had the highest number of interventions (57.5%). Internal Medicine (50.2%) was the unit with the most interventions. Conclusion: CRF patients that are admitted into the emergency department are a key objective concerning dosages in chronic renal failure. Pharmaceutical recommendations are highly esteemed by doctors, given their high acceptance. Revising antimicrobial drugs offers more opportunities.
Antecedentes: La insuficiencia renal crónica (IRC) es una patología que necesita un ajuste posológico de determinados medicamentos. Objetivos: Evaluar las características de las intervenciones farmacoterapéuticas relacionadas con la adecuación de la posología de los medicamentos en los pacientes con IRC que ingresan en un hospital. Métodos: Estudio longitudinal y prospectivo de 10 meses de duración en el que se calculó el filtrado glomerular de los pacientes ingresados desde Urgencias y se seleccionaron los que tenían valores menores de 50 ml/min/1,73 m2. Posteriormente, se realizaron recomendaciones posológicas de los medicamentos que no estaban adaptados a su función renal. Resultados: Se revisó la función renal de 5311 pacientes. Ciento ochenta y uno (3,4 %) tenían un filtrado glomerular menor de 50 ml/min/1,73 m2 y algún medicamento pautado susceptible de ser ajustado. Se registraron 221 intervenciones, siendo la más frecuente la reducción de dosis (65,6 %); un 65,6 % fueron aceptadas por el médico. El grupo de antiinfecciosos tuvo el mayor número de intervenciones (57,5 %). La unidad donde más se intervino fue Medicina Interna (50,2 %). Conclusiones: Los pacientes con IRC ingresados desde Urgencias suponen un objetivo clave en la adecuación de las dosis a la función renal, siendo las recomendaciones farmacéuticas muy valoradas por los médicos por su alta aceptación. La revisión de los medicamentos antiinfecciosos es la que más oportunidades ofrece.
INTRODUCTION
According to the consensus document by the Spanish Society of Nephrology (S.E.N.) from 20081, renal failure is defined as the reduction of renal function, expressed as a glomerular filtration rate below 60ml/min/1.73m2 or having had kidney damage for at least three months.
The prevalence of chronic renal failure in Spain, according to an Epidemiological study on chronic renal failure in Spain (EPIRCE)2 is 6.83% (confidence interval of 95%: 5.41-8.25), which is similar to data obtained during a systematic revision of 26 epidemiological studies conducted throughout the world (7.2%).
Chronic renal failure is a significant health condition as it increases the risk of cardiovascular morbidity and mortality. This medical condition is becoming a global problem, due to an increase in related diseases such as type 2 diabetes mellitus, obesity, high blood pressure or atherosclerosis2.
Patients who have renal failure are admitted into hospital more frequently than people who do not have it3. In these patients, the pharmacokinetics of drugs is altered, given their inability to excrete a drug, which is normally eliminated through the kidney, thereby increasing the probability of adverse effects. This problem is resolved by adjusting the drug dosage; this adjustment is necessary when the amount of the medication that is excreted unalterably through urine is higher than 50% and when creatinine clearance levels are below 50ml/min. This adjustment maximises the drug therapeutical efficiency and minimises adverse reactions, thereby preventing unnecessary additional expenses caused by treating these adverse effects, longer stays in hospitals or hospital readmissions3,4. In this sense, there have been publications that endeavour to establish a dosage guideline to support the prescription and assessment of treatment in patients with renal failure4,5.
OBJECTIVE
The objective of this study is to assess the characteristics of pharmaceutical interventions concerning dosage adjustments of drugs in patients who have chronic renal failure and are admitted into hospital.
METHOD
Design
Descriptive, longitudinal and prospective study conducted between March and December of 2011 on pharmaceutical interventions in patients who suffer from renal failure and who have been admitted into hospital via the emergency department to a tertiary hospital of 1500 beds.
Patient’s informed consent was not required as the activity of doctors and pharmacists was considered routine practise as members of the hospital medical care team.
Patient inclusion
Adults patients who were admitted to hospital wards, or the Observation Unit from the emergency department with glomerular filtration rates below 50ml/min/1,73m2 (calculated with the Modification of Diet in Renal Disease formula which uses a mass spectrometer through isotope dilution or MDRD-4 IDMS1), and had at least one drug on their electronic prescription card with a dosage that could be modified in accordance with their kidney function were included on the study.
Patients who were admitted through the emergency department and later admitted into surgical wards, patients without electronic prescriptions or in Nephrology, Psychiatric, Oncohematology, Intensive Care Units were not included as they were considered to be special cases. Patients with acute renal failure were excluded too.
Methodology
A pharmacist selected the patients who had been admitted through the emergency department the day before and applied the inclusion criteria every day. Subsequently, the last glomerular filtration rates of the patient were obtained, and in their absence, the Creatinine Plasmatic concentration which is obtained by calculating the glomerular filtration from the MDRD-4 IDMS formula with a calculator on the S.E.N website6. The medical history of each patient who had a glomerular filtration rate below 50ml/min/1,73m2 was reviewed in order to check the patient had chronic kidney disease and the drugs prescribe. The different dosages that corresponded with the dosage recommendations on databases were compared. If they were not correct, recommendations for an adjustment were put in writing (modification of dosage, dosage intervals or both) or the medication in question was suspended in the alerts part of the electronic prescription programme, which would be reviewed by a doctor later. Proposals were considered rejected if the doctor did not change them within 72 hours after the intervention. They were considered not assessable if the patient had been moved to a clinical unit that was excluded from our study, discharged or died after 24 hours of issuing the pharmaceutical recommendation.
The databases that were consulted were the technical specifications7, Medimecum8, Micromedex®9 y Lexicomp®10.
Variables
Demographic data (age and sex) was recorded for each patient, together with their kidney function (serum creatinine concentration and glomerular filtration rate calculated with the MDRD-4 IDMS formula), the clinical unit they were admitted from and other data concerning the intervention (drug that was used, dosage recommended by the doctor and acceptance or non-acceptance of the recommendation).
The electronic software used for the statistic analysis was IBM SPSS Statistics 19®. Results were described with the average, standard deviation, median, range and p25-p75 for the continuous variables. Categorical variables were expressed as frequencies and percentages.
RESULTS
The kidney function of 5311 patients who went to the emergency department during the study was reviewed. 181 (3,4 %) patients had a glomerular filtration rate below 50ml/min/1,73m2 and had at least one drug that could be adjusted in accordance with their kidney function.
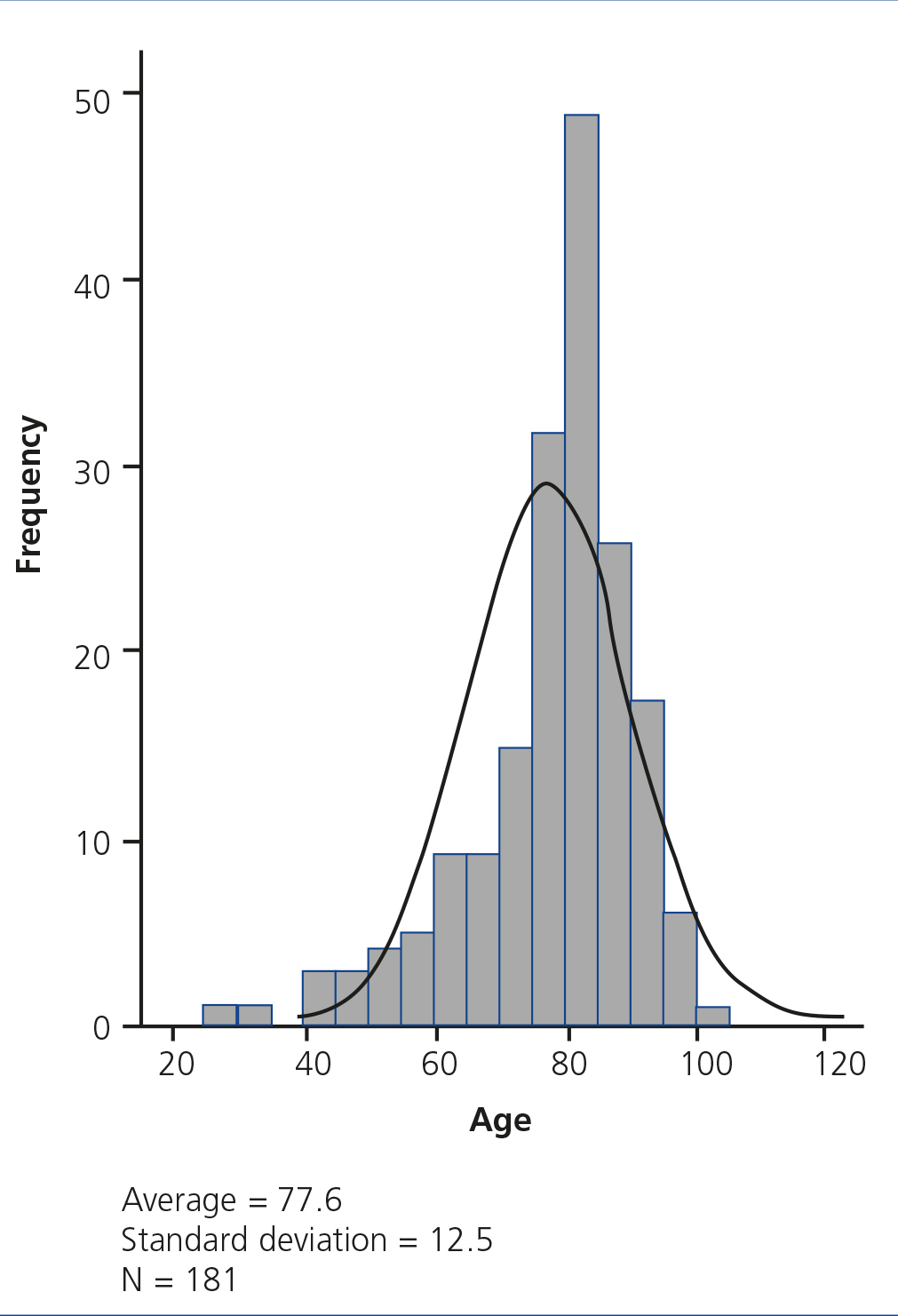
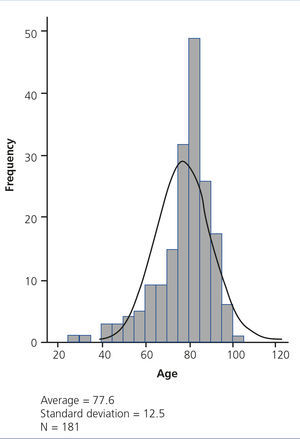
Pharmaceutical interventions were carried out on patients with an average age of 77.6 (Standard deviation [SD]: 12.5) and a median of 80 years of age (range: 29.0-102.0; p25-p75: 73,5-80,0). The distribution of ages is normally curved with a strong deviation to the right and high volume of elderly patients (Figure 1). The average glomerular filtration rate in these patients was 32.3ml/min/1.73m2 (SD: 10.3) and the median was 33.0ml/min/1.73m2 (range: 6-53; p25-p75: 25.4-40.25).
Recommended dosages for chronic renal failure from the literature for 194 drugs were reviewed. 41 different drugs (21.1%) were involved in the intervention, most of them belonging to antimicrobial groups (Group J: 57.5%).
221 interventions in total were recorded. 145 patients (65.6%) were recommended a dosage reduction, 59 patients (26.7%) were given recommendations to expand their daily dosage intervals, 1 patient (0.5%) was given both recommendations and the 16 remaining patients (7.2%) suspended use of the drug.
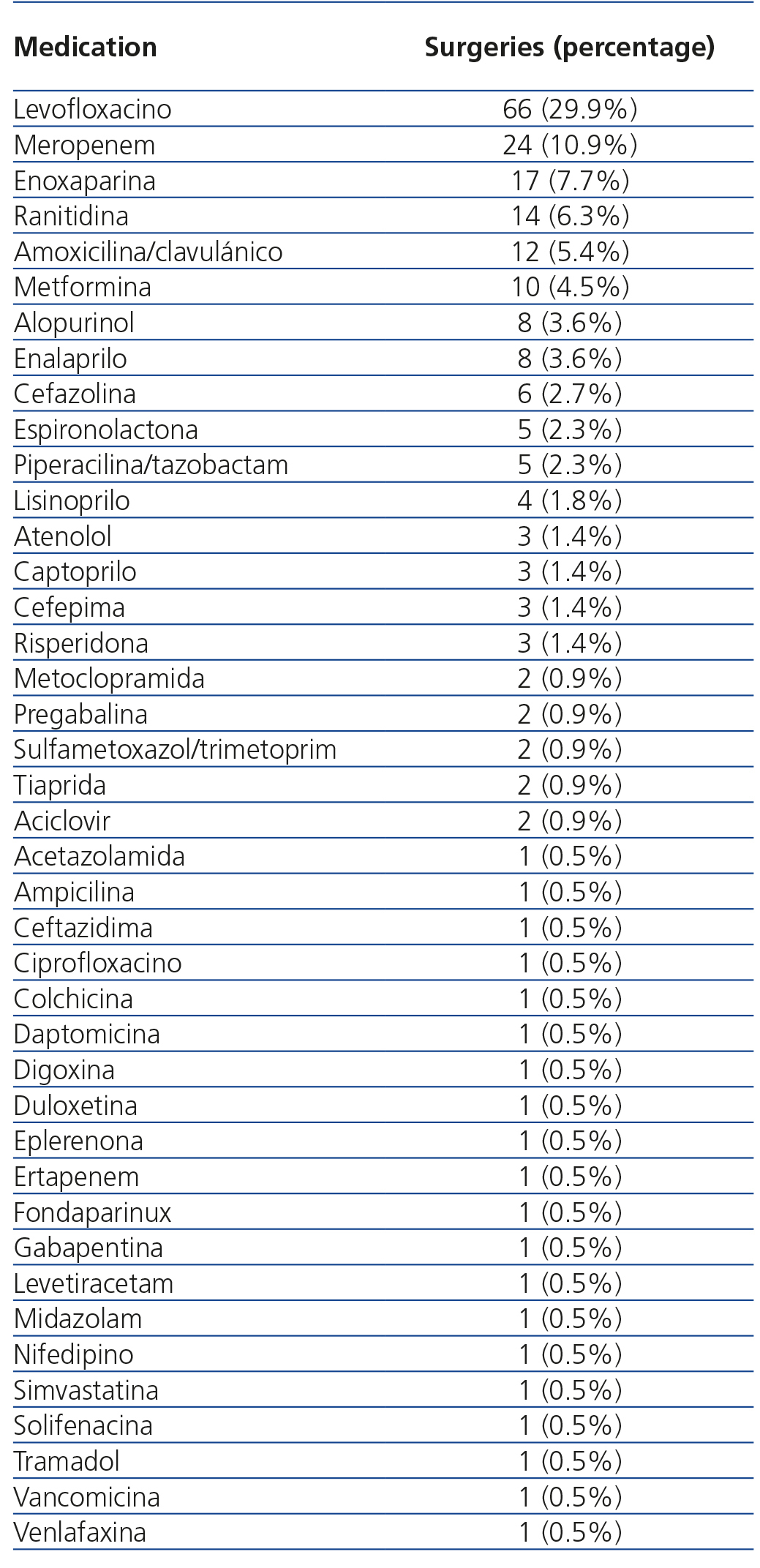
The medication that received the most interventions was levofloxacin (29.9%). A complete list of the medications subject to intervention is shown in Table 1.
The percentage of the global acceptance of the recommendation was 65.6%. Of the interventions, 26.6% were rejected (9.0% due to an improvement of the kidney function, 9.5% due to the medical condition of the patient, which justified the prescribed dosage, and 8.1% without any clear reason). 7.7% of them were not considered assessable.
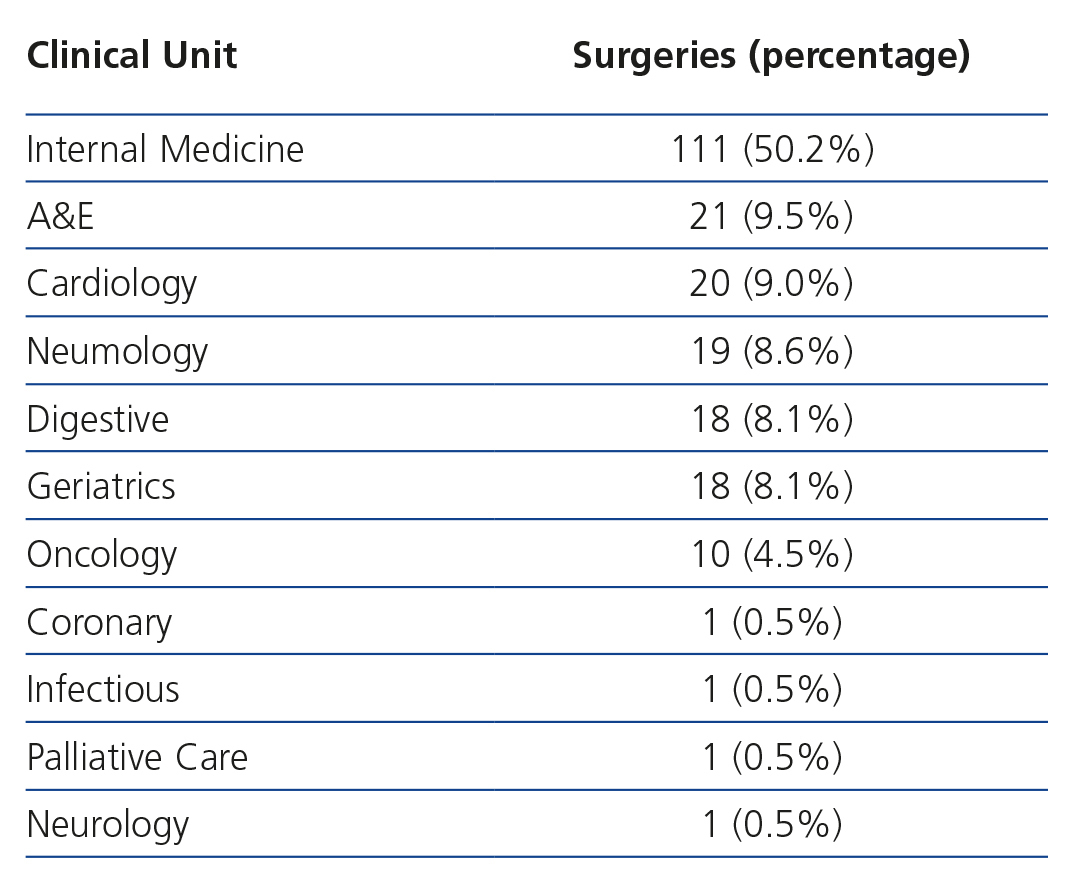
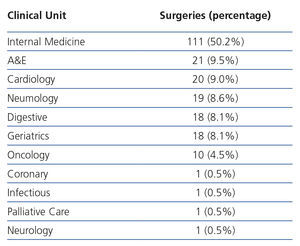
Internal Medicine (50.2%) was the clinical unit that had the most interventions. The distribution of the interventions per unit is included in Table 2.
DISCUSSION
The prevalence of patients with a glomerular filtration rate below 50ml/min/1.73m2 who were taking at least one drug that could be adjusted according to their kidney functions (3.4%) is coherent with the 6.83% of prevalence of kidney failure in Spain, according to EPIRCE2. A limitation found in this study is that not all the patients who had a glomerular filtration rate below 50ml/min/1.73m2 were recorded. In the Falconnier et al. Study in 20014, patients with these characteristics formed 17% of the total of patients who were assessed. One of the main causes of high prevalence of kidney failure in the patients who were admitted was due to old age3.
The population included in this survey was elderly patients, 77.6 years of age being the lower value of the interquartile age range. This element is due to the high prevalence of chronic renal failure in people over the age of 60, which estimated to be about 20%1. The consensus document by S.E.N.1 shows that adjusting drug dosages is recommended in patients with kidney failure, especially in elderly patients as the people who are or are over the age of 60 have an increased risk of suffering from chronic renal failure. This was backed by the EPIRCE study in 20102, in which it was concluded that the most evident predictive factor for chronic kidney failure was age, with an odds ratio of 267.5 patients who were over the age of 64 in comparison to patients who were between 20 and 39 years old. The average glomerular filtration rate of the patients included in the study suffered moderate renal failure, in accordance with clinical guidelines by the National Kidney Foundation in 200211.
The percentage of the drug interventions in comparison with the total number of drugs that were reviewed is high, which highlights the relevance of the process carried out by doctors and pharmacists. The pharmaco-therapeutic group with the highest number of interventions was the antimicrobial drugs, like in other publications3,12-14. Levofloxacin was the most frequent drug. However, the Devesa et al.15 study recorded enoxaparin (71%) in first place, and levofloxacin in second place. Nonetheless, we must bear in mind that aforementioned study included all drugs dosages that could be intervened, and pharmacokinetic monitoring which came from the intervention.
The most frequent intervention was reducing the dosage, just like the results obtained in the Álvarez et al.3study, in which this intervention resulted in 62.9% of the total. We must highlight that a high percentage of interventions recommends the suspension of drug.
In the Devesa et al.15 study, 65.5% of pharmaceutical interventions were obtained, 74 % in the Goldberg et al.16 study, and 54.6% in the pre-intervention phase of the Hassan et al.17 study. The results we obtained in our study are similar. The level of acceptance of the study by Álvarez et al.3 is a little higher (88.6%). Non-acceptance of these recommendations is usually caused by improvements in the kidney function. One-third did not provide a clear reason. Other studies like Álvarez et al.3 or Falconnier et al.4, do not record these types of justifications.
The clinical unit that received the highest number of interventions was the Internal Medicine Unit. It received half of the interventions, followed by the emergency department, which could be due to the high number of polymedicated elderly patients that are included too.
This study recorded patients who were admitted into hospital from the emergency department unit suffering from chronic renal failure. The object of the study was to review the drug’s dosage in accordance with renal function. The objective is to document the implementation value of pharmaceutical attention in this unit. Besides, the American Society of Health-System Pharmacists supports the idea of having hospital pharmacy units within the hospital18. Patients included in the study mainly came from the emergency department, the latter being the first point where the patient is attended.
The renal function of the patient was measured using the glomerular filtration equation MDRD-4 IDMS, which provides the most exact diagnosis for values between 15 and 60ml/min/1.73m2. It is the most used equation in clinical practice, although the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) equation could replace the MDRD-4 IDMS19 equation in the future. The glomerular filtration rate chosen for the study (50ml/min/1.73m2) is lower than 60ml/min/1.73m2 selected as the upper threshold for kidney failure, in accordance with clinical practise guidelines by the National Kidney Foundation11. Álvarez et al. established the thresholds for choosing patients3 at 60ml/min/1.73m2. In this sense, we have a margin of 10ml/min/1.73m2, like the Falconnier et al.4 study, as the high number of drugs that are adjusted to the kidney function of patients recommend adjustments to the normal dosage of drugs from 50ml/min/1.73m2. The Falconnier et al.4 study also used the MDRD-4 IDMS equation to calculate the glomerular filtration rate.
These recommendations were put in writing, by means of the electronic prescription. The Álvarez et al.3 study communicated their recommendation verbally and/or including a report in the patient medical history. The best method was that used in the Falconnier et al.4 study, which consisted of the direct collaboration of the pharmacist who intervenes in the dosage adjustment with the team of doctors who visited the patients.
The main limiting element in putting this study in practise, is the requirement for one person working full time to detect patients who are an objective for pharmaceutical intervention as well as controlling the acceptance and non-acceptance of these interventions, which are not always done instantly. Some of them are put in writing by means of the electronic prescription programme and doctors need time to detect the alert and make their final decision.
Patients who are admitted from the emergency department with chronic renal failure are a key objective for adjusting drug dosages within hospital environments. Medical prescription and pharmaceutical validation are highly important in these processes, as they are filters for any adjustments that can be adapted to the kidney function of these patients. This benefits the safety of the patients as it avoids adverse effects due to overdosing and it saves on expenses.
Reviewing antimicrobial agents and prescriptions from Internal Medicine provide the most opportunities for pharmaceutical interventions. This activity is highly esteemed by prescribing doctors due the high number of acceptance of these interventions and the justification of non-accepted recommendations.
Conflicts of Interest
The authors declare that they have no conflicts of interest related to the contents of this article.
Table 1. Distribution of pharmaceutical interventions by medication
Table 2. Distribution of pharmaceutical interventions by clinical unit
Figure 1. Distribution of pharmaceutical interventions by age