Background: Fluid overload is an important and modifiable cardiovascular risk factor for haemodialysis patients. So far, the diagnosis was based on clinical methods alone. Nowadays, we have new tools to assess more objectively the hydration status of the patients on haemodialysis, as BCM (Body Composition Monitor). A Relative Overhydration (AvROH) higher than 15% (it means, Absolute Overhydration or AWOH higher than 2.5 Litres) is associated to greater risk in haemodialysis. However, there is a group of maintained hyperhydrated patients. The aim of the present study is to identify the characteristics of patients with maintained hyperhydrated status (AvROH higher than 15% or AWOH higher than 2.5 liters). The secondary aim is to show the hemodynamic and analytical changes that are related to the reduction in hyperhydration status. Methods: Longitudinal cohort study during six months in 2959 patients in haemodialysis (HD) that are grouped according to their hydration status by BCM. And we compare their clinical, analytical and bioimpedance spectroscopy parameters. Results: The change in overhydration status is followed by a decrease in blood pressure and the need for hypotensive drugs (AHT) and erythropoiesis stimulating agents (ESA). The target hydration status is not reached by two subgroups of patients. First, in diabetic patients with a high comorbidity index and high number of hypotensive drugs (AHT) but a great positive sodium gradient during dialysis sessions; and, younger non-diabetic patients with longer time on hemodialysis and positive sodium gradient, lower fat tissue index (FTI) but similar lean tissue index (LTI) and albumin than those with a reduction in hyperhydration status. Conclusion: Those patients with a reduction in hyperhydration status, also show a better control in blood pressure and anemia with less number of AHT and ESA. The maintained hyperhydrated patients, diabetic patients with many comorbidities and young men patients with longer time on hemodialysis and non-adherence treatment, can profit from a constant monitoring of their hydration state as well as an individualized treatment (dialysis and drugs).
Introducción: La hiperhidratación es un importante y modificable factor de riesgo cardiovascular para los pacientes en hemodiálisis (HD). Su diagnóstico hasta el momento se había basado en métodos clínicos exclusivamente. En la actualidad disponemos de nuevas herramientas para valorar de forma más objetiva el estado hídrico de los pacientes en HD, como el BCM (Body Composition Monitor). Una sobrehidratación relativa (AvROH) mayor al 15 % por BCM (es decir, unos 2,5 litros de sobrehidratación absoluta o AWOH) se ha relacionado con mayor morbimortalidad en HD. Existe un grupo de pacientes en los que corregir la hiperhidratación resulta especialmente dificultoso. El objetivo de este estudio es identificar las características de aquellos pacientes en los que no conseguimos alcanzar un estado de hidratación, AvROH, menor del 15 % o un AWOH menor a 2,5 litros. Otro objetivo secundario es observar los cambios hemodinámicos y analíticos que la corrección de la hiperhidratación acarrea. Métodos: Estudio de cohortes longitudinal de seis meses de duración en 2959 pacientes en HD que son agrupados en función de su situación hídrica por BCM y en los que comparamos parámetros clínicos, analíticos y de bioimpedancia espectroscópica. Resultados: En aquellos pacientes en que se corrige la hiperhidratación, el cambio se acompaña de un descenso en la tensión arterial y el número de antihipertensivos (AHT), así como del consumo de agentes estimulantes de la eritropoyesis. Los pacientes que se mantienen hiperhidratados se pueden dividir en dos subgrupos: por un lado, pacientes diabéticos con elevado índice de Charlson y consumo de AHT, pero con un gradiente de sodio muy positivo intradiálisis; y por otro lado, jóvenes no diabéticos con elevado tiempo en HD con gradiente positivo de sodio en HD, menor índice de tejido graso, pero similar índice de tejido magro y albúmina que aquellos en que se reduce la hiperhidratación. Conclusiones: Observamos que aquellos pacientes en que se corrige la hiperhidratación presentan un mejor control de la tensión arterial y de la anemia con menor número de AHT y de agentes estimulantes de la eritropoyesis. En los pacientes que permanecen hiperhidratados, diabéticos pluripatológicos y varones jóvenes con elevado tiempo en diálisis y no adherentes al tratamiento o a las recomendaciones, se debe realizar un seguimiento especial y tratamiento dialítico y medicamentoso individualizado.
INTRODUCTION
Fluid overload is an important and modifiable cardiovascular risk factor for haemodialysis patients1-4, both by itself5-8 and because of its effect through high blood pressure9-13.
To date, clinical criteria has been used14-16 to adjust the dry weight of the haemodialysis patients, such as tolerance to the ultrafiltration during dialysis, high blood pressure, orthostatic hypotension, oedemas, and the presence of dyspnoea or asthenia. Imaging tests, such as the cardio-thoracic ratio, the diameter of the inferior vena cava or an echocardiogram have rarely been used and nor have laboratory tests such as the N-terminal propeptide B-type natriuretic peptide14,17, the haematocrit or the albumin for its soluble components16. Thus, with no other tools, the type and the methodology of the dialysis can determine the dry weight of the patient6 and therefore their hydration state.
Today we have new techniques to add to the traditional methods for ascertaining the hydration and nutritional state of the haemodialysis patients and, consequently, for deciding their dry weight. They are body composition monitors, among which the BCM (Body Composition Monitor, Fresenius Medical Care) should be highlighted for its ease of use and, above all, for having been validated both in samples of healthy people and in haemodialysis patients18-20.
The BCM uses the electric properties of the biological tissue (spectroscopic bioimpedance) in order to ascertain the body composition of the subjects through parameters like the lean tissue index (LTI), fat tissue index (FTI) or the "normohydrated weight" of the patient, as well as the distribution of fluids in the body18,20.
The aim of this study is to compare the characteristics of the overhydrated patients with the normohydrated ones by using the BCM. After trying to control the fluid overload in the overhydrated patients for six months, those in which we did not manage to achieve a more appropriate hydration state were studied, absolute overhydration < 2,5 l or relative overhydration < 15 %.
MATERIAL AND METHOD
Patients
A longitudinal cohort study was conducted on 2959 prevalent haemodialysis patients (more than three months on haemodialysis) coming from 49 Spanish HD units in the Fresenius Medical Care network. The inclusion period went from December 2011 (the first measuring of the first patient in the cohort) to December 2012 (the sixth measuring of the last patient included in the cohort).
The criteria for patients to be included were: patients over the age of 18, dialysed with high permeability membrane three times a week on average and with an average effective time of 240 minutes per session. Amputees or patients with pacemakers were excluded. All of them had a monthly measuring with the BCM.
All of them are registered on the EuCliD® database (European Clinical Database of Fresenius Medical Care), already described in previous works21-23 after signing the corresponding informed consent.
Design
The patients included in the study were classified as overhydrated (AvROH > 15 %) or normohydrated (AvROH < 15 %) based on the results of the BCM measurements. It was attempted to bring the overhydrated patients into the normohyrdation range by means of advice on diet and lifestyle and ultrafiltration (adjusting the dry weight). Those which did not achieve this after six months due to poor tolerance were classified as "persistently overhydrated".
Hydration state assessed by the BCM
All patients had a monthly measuring with the BCM and the first six measurements were assessed. Measuring with the BCM is carried out by trained and educated nursing staff who follow a common protocol for arranging the patient and the electrodes before the haemodialysis sessions. The measurements with less than 80% quality were discarded.
The following parameters are included from the BCM: LTI (kg/m2), FTI (kg/m²), extracellular water (ECW, litres), intracellular (litres) and normohydrated weight (kg). Absolute overhydration (OH, litres) is the difference between the pre-dialysis weight and the normohydrated weight given by the BCM. Relative overhydration (ROH = OH/ECW, %) is overhydration normalised to the ECW of the patient, which facilitates the comparison between patients. To avoid bias due to the day on which the measuring took place, we used the average of absolute overhydration (AWOH, litres) and of relative overhydration (AvROH, %) using the data from the two sessions prior to the day which we applied the BCM.
AvWg (litres) is defined as the average inter-dialysis gain in regard to the dry weight determined by the doctor using clinical methods.
According to the literature, a relative overhydration greater than 15% (AvROH) by the BCM leads to a greater risk of death in haemodialysis patients6. Thus, we took the 15% as a reference value for defining the "pathological" overhydration and treatment purpose in our work.
We registered the average pre-dialysis diastolic and systolic blood pressure in a supine position before connection to the extracorporeal circuit, and we calculated the month's average.
Treatment, analytical and demographic parameters or those related to haemodialysis sessions
We collected the age, body mass index (BMI), time on HD, the Charlson index and the possible presence of diabetes mellitus.
The blood test was monthly, pre-dialysis and in the mid-week session. The variables analysed were: haemoglobin, ferritin, transferrin saturation index (TSI), C-reactive protein (CRP) and plasma sodium.
In relation to HD we recorded: vascular access in use, dialysis technique, effective time of dialysis, salt concentration in the dialysis liquid (DL) and salt gradient as a difference between the plasma sodium and the sodium prescribed for the bath; intravenous iron, erythropoiesis-stimulating factors and the calculation of the erythropoietin resistance index (ERI); number of antihypertensive drugs (AHD, compressed) a month; and eKt/V by ionic dialysance using the urea volume given by the BCM.
Statistical analysis
The normality of the distribution in the continuous variables was checked by means of the Kolmorgov-Smirnov test, changing the variables with non-parametric distribution such as the CRP by calculating its logarithm.
We express the quantitative variables as averages and standard deviations. The bivariate comparisons were conducted with the t-Student, Wilcoxon/Anova or U-Mann Withney/Kruskal Wallis test, as appropriate. The comparisons between qualitative variables expressed as a frequency or percentage were carried out with the χ2 test. A result was considered as significant when the p-value was < 0.05 (95% trusted).
The ORD group (Optimizing Results in Dialysis) arose in 2010 with the aim of identifying risk factors and possible treatment actions in the Spanish haemodialysis population, by using the database from the Fresenius Medical Care Centres in Spain to do so.
In regard to the limitations of our study, we have to say that there could be certain bias for not having recorded the residual kidney function of the patients. Although a long period of time on haemodialysis, as is the case with our cohort, is linked to scarce residual diuresis.
RESULTS
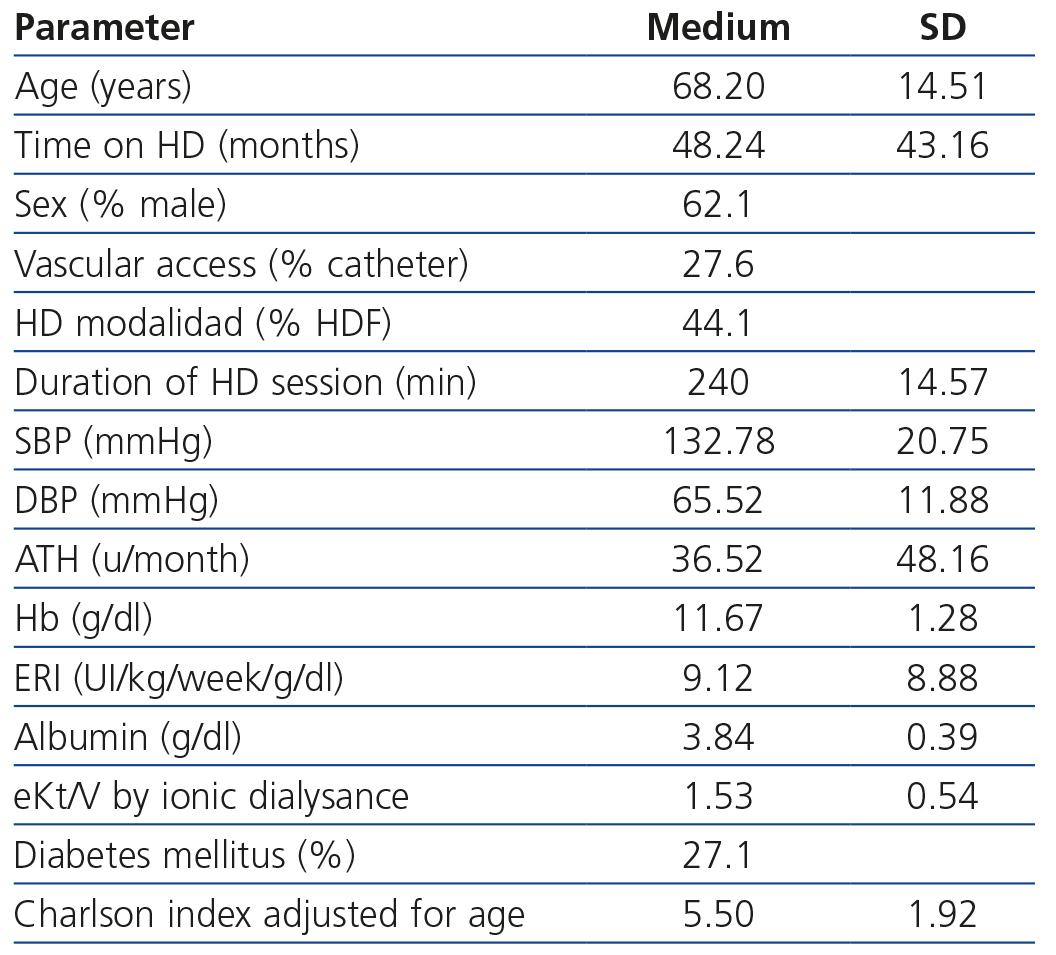
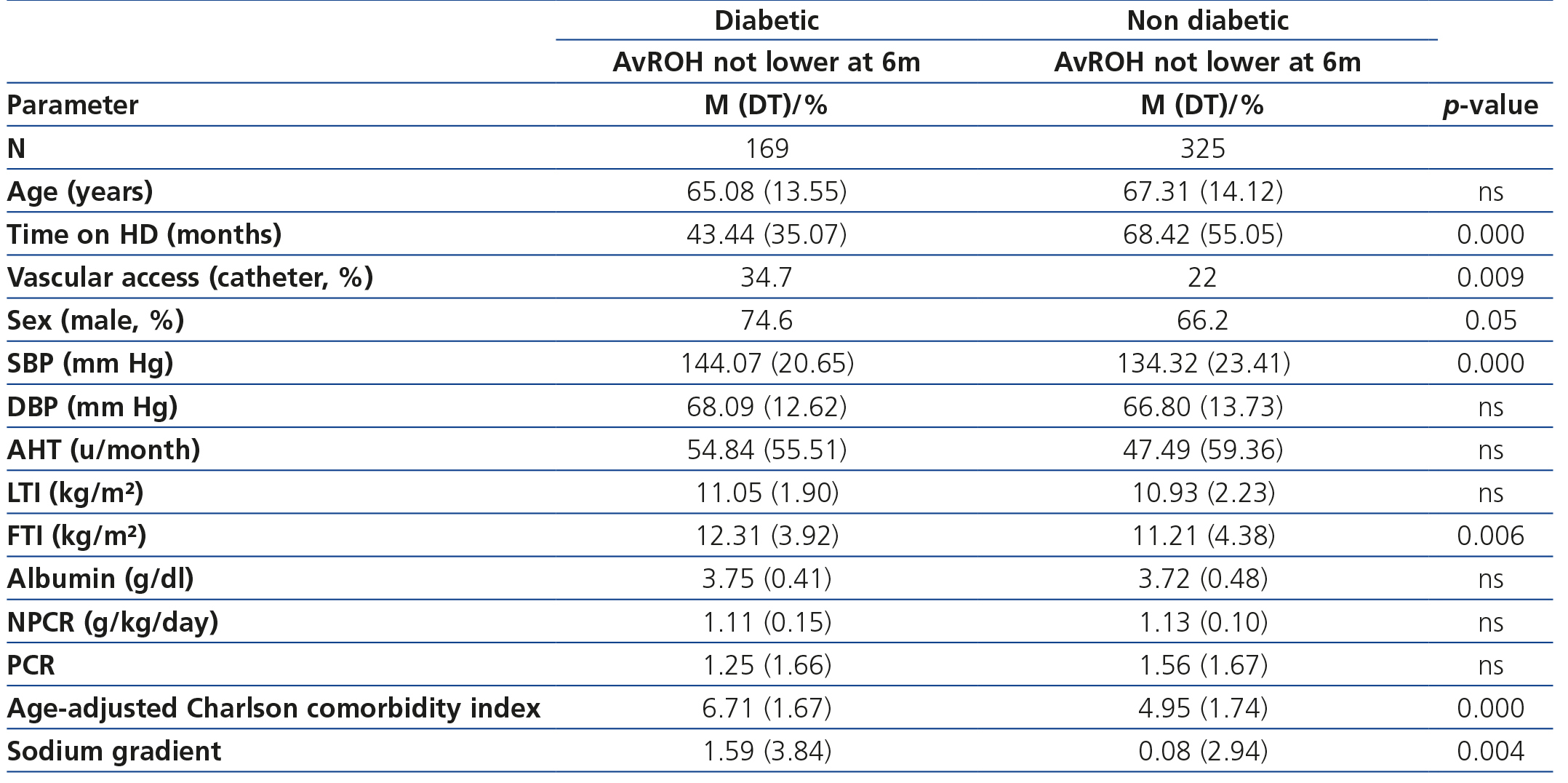
Our sample is made up of 2959 patients. The characteristics at the beginning of the study are described in Table 1.
The most frequent kidney diagnosis was undetermined aetiology (30.7%), followed by diabetic nephropathy (19.4%).
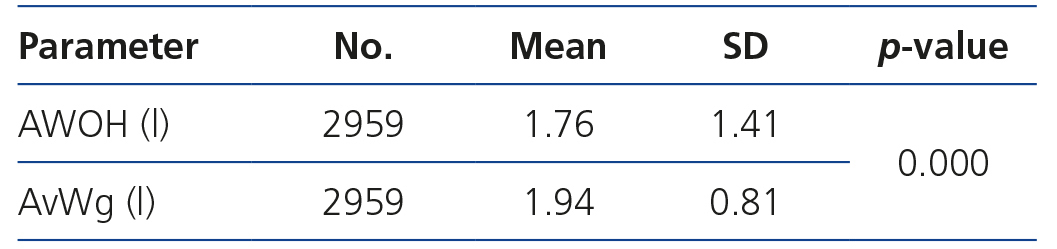
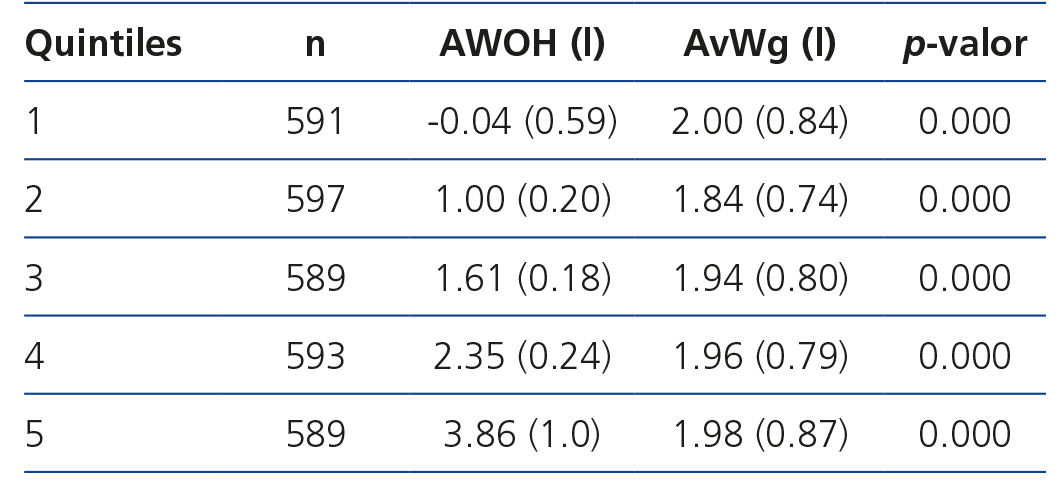
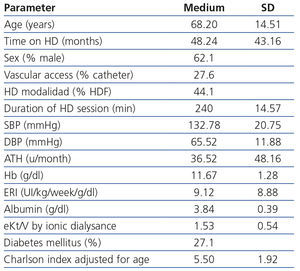
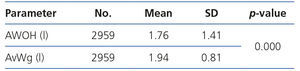
In regard to the baseline anthropometric characteristics, the average BMI was 27.06 (5.14) kg/m², with an average LTI of 11.34 (2.64) kg/m² and an average FTI of 14.76 (5.86) kg/m². In regard to the hydration state: the average AWOH was 1.76 (1.41) l, which corresponds to an average AvROH of 10.63 (8.04) % and an average AvWg of 1.94 (0.81) l (table 2). In the AWOH quintiles (table 3) differences can be seen between the patient's gain in regard to the normohydrated weight calculated by the BCM (absolute overhydration) and the patient's gain in regard to the dry weight determined by the doctor using clinical methods.
Of the 2959 patients included in the study, there were 819 that are overhydrated at baseline according to the BCM, on presenting an AvROH > 15%.
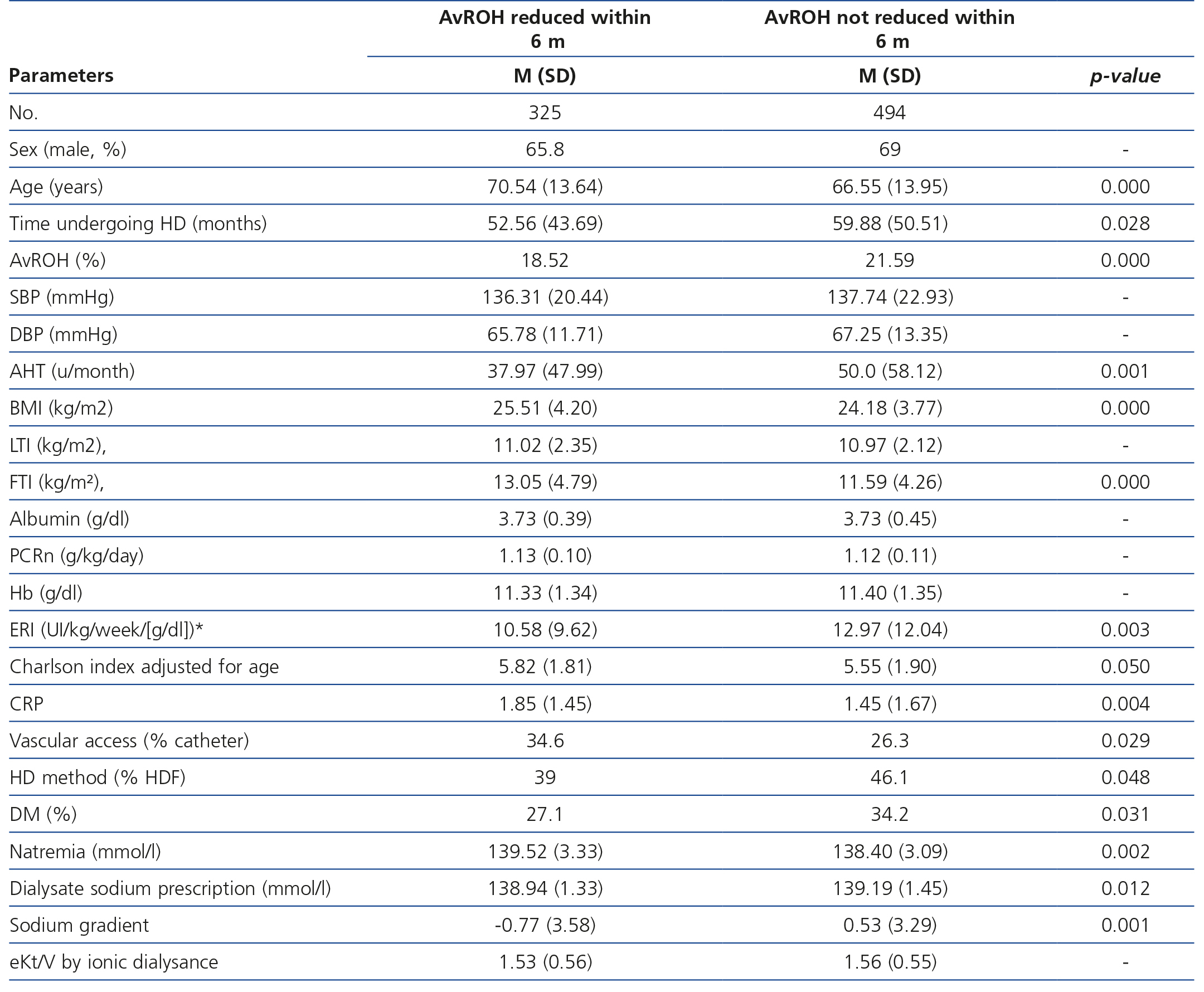
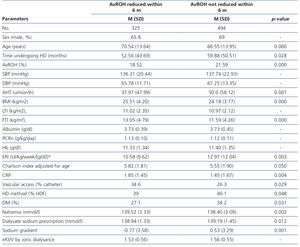
After six months using the BCM as a guide for adjusting the patient's dry weight, we see that of the 819 patients overhydrated at baseline there were 325 in which we managed to reduce their initial AvROH greater than 15% to lower values (from 18.52 ± 3.5 % a 11.16 ± 3.02 %). This change is accompanied by a decrease in systolic blood pressure (136.31 ± 20.44 to 129.78 ± 21.42 mm Hg), diastolic blood pressure (65.78 ± 11.71 to 62.87 ± 10.89 mm Hg) as well as the consumption of AHD drugs (37.97 ± 47.99 to 32.56 ± 41.69 units a month) and of the ERI (10.92 ± 9.72 to 8.71 ± 8.13 UI/Kg/week/g/dl).
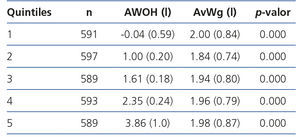
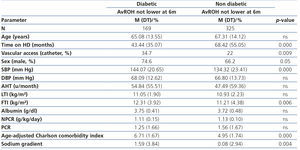
In the remaining 494 patients out of the 819 initially overhydrated ones, we did not manage to reduce the average relative overhydration to values below 15%. This group presents characteristics different to the one in which we managed to correct the initial overhydration. The characteristics are displayed in Table 4 where we can see that it deals with, in general, younger males, but with lower FTI and more time on HD, with a high percentage of them being diabetic, with a high rate of arteriovenous fistula as vascular access, and that consume more AHD drugs with a positive salt gradient during the HD session. The characteristics of the group of persistently overhydrated patients (n = 494) changed depending on whether the person was diabetic or not, as shown in Table 5. We see that the non-diabetic overhydrated patients are younger, but have spent longer time on HD, with low FTI and positive salt gradient, whereas the diabetics have a higher FTI, greater percentage of males, they consume more AHD drugs and the salt gradient is even more than that of the overhydrated non-diabetics.
DISCUSSION
On assessing the hydration state of our HD sample with the BCM and with traditional methods we see that there is a certain discrepancy between the overhydration measured by the BCM, i.e. the patient's fluid overload in regard to the normohydrated weight calculated by the BCM (AWOH) and the inter-dialysis gain, i.e. the patient's fluid overload in regard to the dry weight determined by the doctor using solely clinical criteria (AvWg). These differences are statistically significant overall (Table 2) as well as in all AWOH quintiles (Table 3), with there being "dehydrated" patients according the BCM and at the same time being overhydrated according to clinical criteria.
Using the BCM alongside the normal clinical methods for six months in order to adjust the patients' dry weight and to reach a relative overhydration less than 15% pre-dialysis, we see that those patients in whom we failed to correct the overhydration are younger but with a lower FTI than the rest. We also observe that they present a high prevalence of diabetes mellitus, have spent more time on dialysis, are mainly males with arteriovenous fistula, use a greater number of AHD drugs and have a positive salt gradient during the HD session. However, we did not find differences in regard to albumin and LTI and it even concerned patients with a lower age-adjusted Charlson comorbidity index (Table 4)
Furthermore, on analysing the characteristics of this persistently overhydrated group, we saw that we were actually presented with two different subgroups.
On the one hand, we had younger non-diabetic patients (compared with those in which overhydration was corrected), with a low FTI and with more time on HD, carriers of arteriovenous fistula and with a positive salt gradient during the HD session. Both the lower age8,24 and the greater time on HD5,24 have been linked to overhydration in the literature, where it is affirmed that the older patients are more compliant. Although it is true that the sensation of thirst reduces with age and this is one of the reasons why it is important to achieve a negative or neutral salt gradient during HD sessions25-27, especially in young people. A notable factor is that despite being younger than those in which overhydration was corrected, they presented similar LTI and albumin. Therefore, it is not a case of better nourished patients nor of comorbid ones (age-adjusted Charlson comorbidity index from 4.95 as opposed to 5.82), but of patients not adhering to treatment, which can be strengthened by the positive salt gradient inter-dialysis.
In addition, we have the subgroup of diabetics with a high FTI, carriers of arteriovenous fistula and with a high percentage of males, in which we used more AHD drugs in order to adequately control blood pressure, but also with a positive salt gradient during the HD session. As in previous studies, diabetes is linked to high FTI5, in the same way as being male and diabetic has been linked to high inter-dialysis gains8.
Finding a greater percentage of diabetics among the group of patients that did not manage to correct overhydration (34.2% as opposed to 27.1%) is, in part, probably due to the presence of diabetic neuropathy and poor tolerance to the ultrafiltration that this leads to, as well as a high Charlson index. This would also explain these patients using such a positive salt gradient during the HD session.
However, there were also diabetics among the group of persistently overhydrated patients which used more AHD drugs (54.84 as opposed to 47.49 units/month), although they showed greater figures of systolic blood pressure (144.07 as opposed to 134.32 mmHg), which can be attributed to a greater thickness of the vascular wall4. Although it is a case of values that are far from the 110 mmHg which have been linked to greater mortality in HD28.
Therefore, all this demonstrates that the haemodynamic management or the management of the cardiovascular system of diabetic patients is especially complex and that employing a positive salt gradient to improve haemodynamic tolerance to the HD sessions is a frequently used resource. Consequently, we must ascertain the damaging effects of a positive salt gradient for any patient, such as thirst, inter-dialysis gains25-27 and the increase of ECW with the consequent rise in blood pressure, but also the adjustment to HD does not just depend on the DL, but also other factors such as: the compliance of the patient transgressing salt and/or water25-27; the patient's comorbidities: cardiac patients, damaged peripheral vascular resistances, consumption of hypotensive medication or the presence of hypoalbuminaemia12,29-31; and finally, those aspects related to the dialysis patterns: technique, bath, duration and frequency of the sessions32-36.
In comparison with this group that has remained overhydrated despite the monitoring, we have those patients in which we did manage to reduce overhydration to values which according to the literature lead to lower mortality (AWOH < 2.5 l or AvROH < 15%). We see that this change is accompanied by a statistically significant decrease in systolic and diastolic blood pressure and in the consumption of AHD drugs1. The effect on blood pressure is probably due to acting on its dependent-volume component. In regard to anaemia, we see that after correcting overhydration fewer erythropoiesis-stimulating factors are used for maintaining the haemoglobin at optimum values37,38, which leads to a significant decrease in ERI, as well as the risk some publications attribute to high doses of erythropoiesis-stimulating agents39. The result on the ERI could be due to haemoconcentration and, perhaps, to the impact of overhydration on the inflammatory state of the patient40, which would become lower. Although it is true that the change is not accompanied by a statistically significant reduction of other inflammatory markers such as CRP.
Therefore, we must bear various aspects in mind when controlling overhydration in haemodialysis patients. Firstly, carrying out a periodic diagnosis/observation (monthly or bi-monthly) of this, by using clinical methods along with new complementary tools that are more objective such as the BCM. Secondly, specifically treating the cause of overhydration (avoiding excessive water intake, achieving good glycaemic control, appropriately reducing/adjusting the patient's dry weight and preserving residual kidney function). Finally, achieving better haemodynamic tolerance to the HD sessions by individualising the dialysis technique, its duration, the maximum rate of ultrafiltration per hour and per session, the temperature of the DL and its composition (sodium, potassium, calcium, bicarbonate)32-36, as well as avoiding as far as possible AHD drugs or adjusting the time of administration to the patient's characteristics7,16,41,42.
Good control of the hydration state of the people on dialysis requires an analysis of the patient and of their treatment (dialysis and drugs). It is a complex process that must form part of our daily clinical practice43-47, in order to remove the risk that overhydration carries with it, and also to achieve greater control over blood pressure and anaemia.
In conclusion, we identified those patients in which correcting overhydration was especially difficult and we saw that there were two subgroups of patients with very different characteristics. On the one hand, co-morbid diabetic males that used a large number of AHD drugs to control overhydration, to whom we applied a very high positive salt gradient to in HD. On the other hand, non-diabetic young patients on HD for a long time and who did not adhere to the treatment or recommendations, which could benefit from a positive salt gradient. In both subgroups it is especially convenient to add new tools and strategies to our daily practice in order to appropriately manage their cardiovascular system. Additionally, in those patients in which overhydration was corrected, the change was accompanied by a fall in blood pressure and in the number of AHD drugs, as well as ERI and in the consumption of erythropoiesis-stimulating agents.
It is still necessary to demonstrate in prospective studies if an objective guide for overhydration could lead to an improvement in survival, as well as following the evolution of the "dehydrated" patients in relation to mortality.
Acknowledgements
We would like to thank all the doctors at the Fresenius Medical Care clinics in Spain for their participation in the inclusion and collection of data, without which this work could not have been done.
Conflicts of interest
The authors declare the following potential conflicts of interest.
Some of the authors are members of the ORD scientific group promoted by Fresenius Medical Care Spain.
Table 1. Baseline characteristics of the 2959 patients
Table 2. Baseline hydration state of the 2959 patients. Comparison of average overhydration calculated by the BCM (AWOH) and average overhydration according to clinical methods. (AvWg)
Table 3. Comparison of the average overhydration by the BCM and the average overhydration according to clinical methods in the different AWOH quintiles
Table 4. Baseline characteristics of the patients with AvROH on T0 greater than 15% grouped according to whether the overhydration descends or not after six months of monitoring with the BCM
Table 5. Baseline characteristics of the patients who did not correct their overhydration in six months of monitoring, grouped in diabetics and non-diabetics.