Chronic kidney disease (CKD) and atrial fibrillation (AF) frequently coexist, amplifying the risk of cardiovascular events and mortality. In patients with CKD stage 3 and non-valvular AF, direct oral anticoagulants (DOACs) have shown, compared to vitamin K antagonists (VKA), equal or greater efficacy in the prevention of stroke and systemic embolism, and greater safety. There are no randomizedtrials of the efficacy and safety of DOACs and VKA in advanced CKD. On the other hand, observational studies suggest that DOACs, compared to warfarin, are associated with a lower risk of acute kidney damage and generation/progression of CKD. This paper reviews the epidemiological and pathophysiological aspects of the CKD and AF association, the evidence of the efficacy and safety of warfarin and ACODs in various stages of CKD with AF as well as the comparison between warfarin and ACODs in efficacy and anticoagulant safety, and in its renal effects.
La enfermedad renal crónica (ERC) y la fibrilación auricular (FA) frecuentemente coexisten amplificando el riesgo de eventos cardiovasculares y de mortalidad. En pacientes con ERC estadio 3 y FA no valvular, los anticoagulantes orales de acción directa (ACOD) han demostrado, comparados con antagonistas de la vitamina K (AVK), igual ó superior eficacia en la prevención de ictus y embolismo sistémico, y mayor seguridad. No existen ensayos randomizados de la eficacia y seguridad de ACOD y AVK en la ERC avanzada. Por otra parte, estudios observacionales sugieren que los ACOD, comparados con warfarina, se asocian a menor riesgo de daño renal agudo y de generación/progresión de ERC. En este trabajo se revisan los aspectos epidemiológicos y fisiopatológicos de la asociación ERC y FA, las evidencias de la eficacia y seguridad de la warfarina y de los ACOD en las diversas fases de la ERC con FA así como la comparación entre warfarina y ACOD en la eficacia y seguridad anticoagulante, y en sus efectos renales.
Chronic kidney disease (CKD) is defined by the presence structural or functional abnormalities with clinical significance for at least three months. Its most common signs are a reduction in glomerular filtration rate (GFR) and/or albuminuria. Formulas for determining estimated GFR (eGFR), such as the Modification of Diet in Renal Disease (MDRD) equation and the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) equation, are accepted.1–3
Calculation of the albumin-to-creatinine ratio in the first morning urine is the most commonly accepted method to determine albuminuria. A combination of values of eGFR (ml/min) and albuminuria (mg/g) serves to establish the different stages of CKD2,3: stage 1: GFR > 90 and albuminuria; stage 2: GFR 60–89 and albuminuria; stage 3a: GFR 45–59; stage 3b: GFR 30–44; stage 4: GFR: 15−29; stage 5: GFR < 15; stage 5D: dialysis. In any stage, albuminuria involves higher renal and vascular risk. Stage 2 corresponds to mild CKD, stage 3 to moderate CKD, stage 4 to severe CKD, stage 5 to kidney failure without renal replacement therapy and stage 5D to kidney failure with renal replacement therapy.4
The prevalence of CKD in Spain is 15%. It is more prevalent in men, advanced age and subjects with cardiovascular disease (CVD) or cardiovascular risk factors.5 CKD is a significant risk factor for CVD. Diabetes mellitus (DM) and hypertension (HTN) are the most significant causes of CKD.
The prevalence of atrial fibrillation (AF) in the general population is 0.95%. In those over 60 years of age, its prevalence reaches 8.5% and it is associated with CVD and HTN.6
CKD is associated with AF. Subjects with an increase in albuminuria and/or reduction in GFR have a higher incidence of AF. In a large study including 10,328 subjects followed up for 10 years. AS compared with patients with eGFR ≥ 00A0;90 ml/min/1.73 m2, those with stage 2 CKD the hazard ratio (HR) for AF was 1.3 (95% CI: 1.1–1.6) in those with stage 4 CKD the HR was 3.2 (95% CI: 2.3–4.5). The risk was especially high when a reduction in eGFR was combined with macroalbuminuria (HR 13; 95% CI: 6–28).7 In a meta-analysis of 25 studies in subjects with CKD and dialysis, the prevalence of AF was 11.6%.8 Older age and longer period of time on dialysis were independently associated with AF.9 In patients ≥67 years of age, the incidence of AF in the first three months on peritoneal dialysis was 19/100 patients/year, and 37/100 patients/year on haemodialysis (HD).10
Given the consistency of the association between CKD and AF, the guidelines include CKD as a risk factor for AF.11
Various mechanisms may account for the higher frequency of AF in CKD. The two diseases share risk factors (advanced age, HTN, diabetes, CVD, obesity, etc.) and pathogenic mechanisms, such as inflammation, oxidative stress and increased activity of the renin-angiotensin-aldosterone system (RAAS). In CKD, additional mechanisms such as vascular calcifications, increased sympathetic activity, arterial stiffness and fibroblast growth factor (FGF23)12 directly or indirectly promote the onset of AF. The association between CKD and AF persists in all subgroups of CKD after adjusting for other comorbidities and vascular risk factors, suggesting the involvement of additional factors particular to CKD.13
Consequences of atrial fibrillation in chronic kidney diseaseEffects of atrial fibrillation on kidney function in chronic kidney diseaseCKD promotes the onset and persistence of AF, which in turn has an impact in kidney function. In a prospective population-based study, after six years of follow-up, the risk of onset of AF was 22% in subjects with an eGFR between 60 and 30, and 57% in subjects with an eGFR < 30 ml/min/1.73 m2. During the follow-up, subjects with initial AF were found to have an increased risk of a reduction in GFR and the onset of proteinuria, regardless of whether they had treated HTN or DM.14 CKD promotes the recurrence of AF following catheter ablation and, in turn, the restoration of sinus rhythm results in sustained improvement in kidney function.15,16 In adults with CKD, the onset of AF promotes the progression of the kidney disease.17 In addition to the possible haemodynamic effects of AF on kidney function, this bidirectional relationship between CKD and AF supports the notion that the two diseases share abnormal molecular signalling pathways that contribute to their pathogenesis.18,19
Effects of atrial fibrillation on cardiovascular events in chronic kidney diseaseCKD carries a high risk of cardiovascular (CV) and thromboembolic events based in pathophysiological abnormalities that promote hypercoagulability, such as greater left atrial blood stasis and an increase in procoagulant and proinflammatory mediators.20,21
Furthermore, in CKD, abnormalities are observed in fibrin clot structure that increase with CKD stage and may lead to greater resistance to fibrinolysis.22,23
AF increases the risk of stroke by four to five times. In all stages of CKD, AF increases the incidence of stroke and mortality.8,24 Subjects with both CKD and AF are at higher risk of stroke and of mortality than those with CKD without AF.8,25
The Chronic Renal Insufficiency Cohort (CRIC) study confirmed that, in subjects with CKD and eGFR 20−60 ml/min/1.73 m2, new-onset AF is independently associated with higher risks of heart failure (HF), myocardial infarction, stroke and death.26 In subjects with CKD on dialysis and new-onset AF, adjustment for competing risk of hospital death may reduce the significance of the role of AF in stroke and thus lessen the efficacy of some preventive strategies for stroke.27
Stratification of risk of stroke in atrial fibrillation with chronic kidney diseaseA key element in preventing AF-related stroke is effective risk stratification. CHADS2 and CHA2DS2-VASc scores constitute a validated tool for assessing the risk of cerebrovascular accident and systemic embolism.12 In patients on dialysis, both CHADS2 and CHA2DS2-VASc predict the risk of stroke.28
Since kidney dysfunction is a powerful predictor of risk ofstroke, it has been proposed that it be included in stroke risk stratification. Adding creatinine clearance (CrCl), estimated by the Cockcroft-Gault (CG) formula, to CHADS2 (adding 2 points if CrCl <60 ml/min to arrive at the so-called R2CHADS2) slightly improves the net index of reclassification of risk of stroke and systemic embolism compared to CHADS2 and CHA2DS2-VASc. However, the performance of R2CHADS2, in terms of the statistic “c”, is modest.29 Adding eGFR determined by MDRD to CHADS2 and CHA2DS2-VASc did not contribute information independently predictive of stroke.30The anticoagulation and risk factors in atrial fibrillation (ATRIA) scoring system, which includes an eGFR <45 ml/min and proteinuria, offers a slight marginal improvement, compared to CHADS2 and CHA2DS2-VASc, in the c-statistic in predicting stroke in patients with AF.31
CKD is associated with risk factors of stroke included in CHADS2 and CHA2DS2-VASc. Hence, there is an unsurprising lack of "independent" additive effects of kidney function parameters when they are added to them. The CHA2DS2-VASc remains the most commonly recommended scoring system for stroke risk stratification.11
Several haemorrhage risk scoring systems, including HAS-BLED, include kidney dysfunction, which increases the risk of bleeding. The guidelines indicate that, in generally, an elevated risk of haemorrhage should not ruled out to anticoagulant therapy being. Rather, treatable risk factors for haemorrhage must be identified and corrected.11
Prevention of stroke and oral anticoagulation in chronic kidney disease with atrial fibrillationThe most effective treatment for thromboprophylaxis of stroke and systemic embolism in subjects with AF is oral anticoagulation. Drugs that inhibit vitamin K metabolism (coumarins, warfarin and acenocoumarol), which is required for synthesising several clotting factors, have been available for more than 50 years. Other drugs that inhibit factor Xa (rivaroxaban, apixaban, edoxaban and betrixaban [the latter is not on the European market]) and thrombin (dabigatran), known as oral anticoagulants of a direct action (DOACs), have been available for 10 years.
Adjusted doses of warfarin, compared to "no treatment" or to antiplatelet therapy, reduce the incidence of stroke in patients with non-valvular AF.32 Despite their effectiveness, vitamin K antagonists (VKAs) carry disadvantages: narrow therapeutic range, slow onset and slow disappearance of their effects, drug interactions and dietary restrictions, in addition to requirements for monitoring and dose adjustment.33
Anticoagulation is particularly complex in patients with CKD. This situation entails a confluence of procoagulant and prohaemorrhagic phenomena. The former result from common vascular abnormalities, increased proinflammatory mediators and endothelial dysfunction, plus resistance to fibrinolysis and greater platelet aggregation.21,23,34 In more advanced stages of CKD the bleeding tendency is due to platelet dysfunction and their deficient adherence to the subendothelium. Effects that are enhanced by concomitant anaemia, which is actually common.34
Warfarin in chronic kidney diseaseFew studies have been conducted with warfarin in patients with AF and CKD, and those with stage 4, 5 or 5D CKD have been systematically excluded from clinical trials. Administration of warfarin at an adjusted dose (international normalised ratio [INR] 2−3), compared to aspirin plus fixed low doses of warfarin, reduced the risk of stroke/systemic embolism by 76% with no increase in major haemorrhages in a limited number of patients with stage 3 CKD.35
In a systematic review and meta-analysis of observational studies that included 11 cohorts (41,767 patients with CKD stage 3 or 4, and 6776 patients with CKD stage 5D), warfarin reduced the risk of stroke and mortality (by 36% and 25%, respectively), and there was no increase in the risk of major haemorrhages in the group with CKD stage 3 or 4. In patients with CKD on replacement therapy with dialysis, warfarin neither decreased the risk of stroke/systemic embolism nor decreased the risk of mortality, but did bring about a significant increase in major haemorrhages. This study36 concluded that warfarin has a favourable risk/benefit effect in moderate CKD, but not in stage 5D CKD. However, analysis of studies (all of them observational) on the effect of warfarin in subjects with AF and CKD on dialysis there were observed highly variable results: reduction in overall mortality, neutral effects, increase in recurrent hospitalisations for CV-related reasons or, in some studies, an increase in embolic stroke and haemorrhage.37–39 These disparities may have been due in part to differences in anticoagulation characteristics. Observational studies featuring INR results have shown that time in therapeutic range (TTR), a measure of anticoagulation quality ( is recommended to be >70%), is lower in subjects with CKD and that this is linked to embolic and haemorrhagic events.40The lower the GFR, the lower the TTR and the larger the number of strokes.41
The impact of CKD on TTR may be attributed to several causes: although warfarin is eliminated through the liver, it is possible that CKD affects its metabolism and its bioavailability by altering the activity of cytochrome p450 2C942; in CKD there may be lower treatment adherence due to the polymedication which is common in these patients and, finally, dietary restrictions due to the risk of hyperkalaemia and intestinal dysbiosis, also common in CKD,43 may affect intake and intestinal production of vitamin K.
Often, in moderate to severe CKD, a lower dose of warfarin is required to maintain therapeutic anticoagulation, anticoagulation management is deficient and a higher risk of haemorrhages is present.44,45
Direct-acting oral anticoagulants in chronic kidney disease and atrial fibrillationThe four trials of phase 3 of DOACs (dabigatran, rivaroxaban, apixaban and edoxaban) analysed the efficacy in prevention of stroke/systemic embolism and safety (major haemorrhagic complications) of DOACs in patients with non-valvular AF at moderate to high risk by comparing them to warfarin.46–49 A meta-analysis of the four trials found that DOACs show greater efficacy in reducing stroke/systemic embolism, a trend towards a lower risk of major haemorrhages, lower mortality and risk of haemorrhagic stroke, and a higher risk of gastrointestinal haemorrhage.50 This clearly reflects a favourable risk/benefit profile for DOACs compared to warfarin.
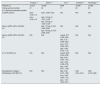
When considering the use of DOACs in patients with CKD and non-valvular AF, it is important to bear in mind the metabolism of DOACs.51,52 All of them are resecreted by the gut through glycoprotein P. Apart from dabigatran, all are metabolised to different degrees by cytochrome p450, subtype 3A4 and, above all, they differ in terms of degree of excretion through the kidneys (Table 1). These pharmacodynamic characteristics that led to one of the exclusion criteria in studies of DOACs (patients CKD stage 4, 5 or 5D CKD). Kidney function was also what determined the dose (Table 1). Despite a lack of clinical studies on safety, based on pharmacokinetic studies, recommendations for prescription and dose adjustment of DOACs based on kidney function have been proposed. These recommendations vary depending on the regulatory agency and the guidelines53–55 (Table 2).
Metabolism of direct-acting oral anticoagulants (DOACs) and patients with chronic kidney disease (CKD) included in the pivotal trials of DOACs.
| Dabigatran | Rivaroxaban | Apixaban | Edoxaban | |
|---|---|---|---|---|
| Mechanism of action | Direct thrombin inhibitor | Direct factor Xa inhibitor | Direct factor Xa inhibitor | Direct factor Xa inhibitor |
| Half-life (hours) | 12−17 | 5−9 | 12 | 10−14 |
| Renal clearance (%) | 80 | 35 | 27 | 50 |
| Dialyzable | Yes | No | No | No |
| Exclusion criterion in patients with CKD in the pivotal trials (CrCl [ml/min]) | <30 | <30 | <25 | <30 |
| % of patients with CKD in the pivotal trials | 20% with CrCl 30−49 ml/min | 21% with CrCl 30−49 ml/min | 15% with CrCl 30−50 ml/min | 19% with CrCl <50 mL/min |
| Dose adjustment in patients with CKD in the pivotal trials | None | 15 mg/day if CrCl 30−49 ml/min | 2.5 mg/2 times/day if CrCl ≥1.5 mg/dl + age ≥80 or weight ≤60 kg | 30 or 15 mg/day if CrCl <50 ml/min |
CrCl: creatinine clearance.
Dose of oral anticoagulants depending on kidney function (according to EMA, FDA and KDIGO)a.
| [0,2–6]Creatinine clearance (CG) (ml/min) | |||||
|---|---|---|---|---|---|
| >50 | 30−39 | 15−29 | <15 | Dialysis | |
| VKAs | Maintain TTR ≥ 70% | Maintain TTR ≥ 70% | Maintain TTR ≥ 70% | Maintain TTR ≥ 70% | Maintain TTR ≥ 70% |
| Dabigatran | 150 mg ⋅2 or 110 ⋅2 if age ≥80, receiving verapamil or haemorrhagic risk | 150 mg ⋅2 or 110 ⋅2 if age ≥80, receiving verapamil or haemorrhagic risk | -EMA: not recommended | Not recommended | Not recommended |
| -FDA: reduced dose (75 mg ⋅2 (only available in the United States) | |||||
| -KDIGO: 75 mg ⋅2b | |||||
| Rivaroxaban | 20 mg/day | 15 mg/day | 15 mg/day | Not recommended | Not recommended |
| -KDIGO: 15 mg/day could be considered | KDIGO: unknown effect. 15 mg/dayb | KDIGO: unknown effect. 15 mg/dayb | |||
| Apixaban | 5 mg ⋅2 or 2.5 mg ⋅2 if ≥2 of the following: age ≥80; Cr ≥1.5 mg/dl; weight ≤60 kg | 5 mg ⋅2 or 2.5 mg ⋅2 if ≥2 of the following: age ≥80; Cr ≥1.5 mg/dl; weight ≤60 kg | -EMA: 2.5 mg ⋅2 | -EMA: not recommended | EMA: not recommended |
| -FDA: 5 mg ⋅2 | -FDA: 5 mg ⋅2 | FDA: 5 mg ⋅2 | |||
| -KDIGO: 2.5 mg ⋅2 could be considered | -KDIGO: unknown effect (2.5 mg ⋅2)b | KDIGO: unknown effect (2.5 mg ⋅2)b | |||
| Edoxaban | 60 mg/day | 30 mg/day | 30 mg/day | Not recommended | Not recommended |
| -KDIGO: 30 mg/day could be considered | |||||
VKAs: vitamin K antagonists; CG: Cockcroft-Gault; EMA: European Medicine Agency; FDA: Food and Drug Administration; KDIGO: Kidney Disease Improving Global Outcomes; TTR: time in therapeutic range.
There are no data on clinical safety and efficacy; the doses for dabigatran (75 mg ⋅2), rivaroxaban (15 mg/day) and apixaban (5 mg ⋅2) included by the FDA are based on limited pharmacokinetic and pharmacodynamic data. The KDIGO guideline suggests considering apixaban at low doses of 2.5 mg ⋅2 if GFR is <15 ml/min and on dialysis.
It is important to point out several things:
- 1
There is a lack of randomised trials of DOACs in subjects with stage 4, 5 or 5D CKD.
- 2
In basic studies, initial DOAC doses were not modified according to changes in kidney function over time.
- 3
Determination of kidney function in these studies with DOACs was done with estimated CrCl using the Cockcroft-Gault formula.
The four phase 3 trials that compared DOACs to warfarin did a subanalysis of safety and efficacy in the subgroup of subjects with CKD, defining kidney function in terms of CrCl (normal: CrCl >80 ml/min; mild CKD: CrCl 50−80 ml/min; moderate CKD: CrCl 30−50 ml/min). All of them excluded subjects with CrCl <30 ml/min, except the apixaban study, which excluded those with a CrCl <25 ml/min. Out of a total of 70,952 patients included in the four studies, 45,265 had mild to moderate CKD (stage 2 or 3), and very few (n = 390) had severe CKD (stage 4).56–59
As shown in Table 3, DOACs represent a safer and more effective option than warfarin in subjects with mild to moderate CKD. Furthermore, some advantages and beneficial effects of DOACs versus warfarin are not detected in subjects with normal kidney function.
Hazard ratio for stroke/systemic embolism and major haemorrhage in patients treated with direct-acting oral anticoagulants versus those treated with warfarin depending on degree of kidney function.
| [0,2,3]CrCl >80 ml/min | [0,4,5]CrCl 50–80 ml/min | [0,6,7]CrCl <50 ml/min | ||||
|---|---|---|---|---|---|---|
| Stroke/SE | MH | Stroke/SE | MH | Stroke/SE | MH | |
| Drug | HR (95% CI) | HR (95% CI) | HR (95% CI) | HR (95% CI) | HR (95% CI) | HR (95% CI) |
| Dabigatran58 | ||||||
| 110 mg ⋅2 | 0.84 (0.54−1.32) | 0.61 (0.44−0.84) | 0.93 (0.70−1.23) | 0.76 (0.62−0.94) | 0.85 (0.59−1.24) | 0.99 (0.77−1.28) |
| 150 mg ⋅2 | 0.67 (0.42−1.09) | 0.84 (0.62−1.13) | 0.68 (0.50−0.92) | 0.91 (0.75−1.11) | 0.56 (0.37−0.85) | 1.01 (0.79−1.30) |
| Rivaroxaban56,a | 0.78 (0.63−0.98) | 1.04 (0.96−1.13) | 0.78 (0.63−0.98) | 1.04 (0.96−1.13) | 0.84 (0.57−1.23) | 0.98 (0.84−1.14) |
| Apixaban57 | 0.88 (0.64−1.22) | 0.80 (0.61−1.04) | 0.74 (0.56−0.97) | 0.77 (0.62−0.94) | 0.79 (0.55−1.14) | 0.50 (0.38−0.66) |
| Edoxaban59,b | 1.36 (0.88−2.10) | 0.60 (0.42−0.85) | 0.78 (0.64−0.96) | 0.89 (0.75−1.04) | 0.87 (0.65−1.18) | 0.76 (0.58−0.98) |
CrCl: creatinine clearance; MH: major haemorrhage; SE: systemic embolism.
The effects of direct anticoagulants that, compared to warfarin, were more beneficial in those with kidney dysfunction compared to those with normal kidney function appear in bold.
The effects of DOACs versus warfarin in subjects with or without CKD were also compared using meta-analyses that included four phase 3 trials of DOACs. A meta-analysis by Zou et al.60 found that as compared to warfarin, DOACs caused a similar decrease in risk of stroke/systemic embolism in subjects with normal kidney function (relative risk [RR]: 0.93; 95% CI: 0.81–1.01). However, a reduction in risk was significantly greater in cases of mild CKD (stage 2) (RR: 0.79; 95% CI: 0.68−0.91) and moderate CKD (stage 3) (RR: 0.87; 95% CI: 0.69−0.94). The decrease in major haemorrhages in those patients treated with DOACs was greater with warfarin — both in normal kidney function and CKD.
Similar results were obtained in a meta-analysis by Del Carpio et al.61 The reduction in risk of stroke/systemic embolism in those treated with DOACs versus warfarin was greater in those who had mild CKD (RR: 0.79; 95% CI: 0.66−0.94) or moderate CKD (RR: 0.71; 95% CI: 0.62−0.81), whereas it was similar in those with normal kidney function (RR: 0.95; 95% CI: 0.81–1.15). Both meta-analyses showed a trend towards a greater reduction in haemorrhages with DOACs in patients with a more advanced stage of CKD, although there was a great heterogeneity.
In a Cochrane review of patients with CKD and non-valvular AF enrolled in phase 3 trials of DOACs (12,155 with stage 3 CKD and 390 with stage 4), subjects treated with DOACs compared to subjects receiving warfarin had a lower risk of stroke/systemic embolism (RR: 0.81; 95% CI: 0.65–1) and a tendency to have fewer major haemorrhages (RR: 0.79; 95% CI: 0.59–1.04).62 The major limitation of this study, as the authors acknowledged, was that it only represented patients with stage 3 CKD.
All these meta-analyses have the disadvantage that the subgroups included by kidney function were not predetermined and the comparative analysis was not prespecified in the phase 3 studies. Despite this, the results supported the notion that DOACs have greater safety and efficacy versus warfarin in the presence of mild or moderate CKD.
A recent systematic review of randomised studies, cohort studies and case series63 found that, in moderate CKD, dabigatran and apixaban, compared to warfarin, reduced the risk of stroke/systemic embolism (dabigatran: HR 0.55 and 95% CI: 0.34−0.85; apixaban: HR: 0.61 and 95% CI 0.39−0.94), while edoxaban and apixaban were associated with a lower number of major haemorrhages than warfarin.
Probably the best information supporting the choice of optimal anticoagulation (DOACs versus warfarin) is based on the “net clinical benefit” (NCB), which incorporates the risk of stroke/systemic embolism and the risk of major haemorrhages. It is calculated according to the following formula:
A recent meta-analysis of phase 3 studies of DOACs analysed the NCB.64 Compared to warfarin, DOACs had a positive NCB in subjects with mild CKD (1.59; 95% CI: 1.03–2.15) or moderate CKD (2.74; 95% CI: 1.72−3.76). They also had a superior NCB to warfarin in subjects with normal kidney function. It should be noted that the NCB progressively increased as the stage of CKD increased. In a frail population, the greatest determinant of NCB in favour of DOACs was the lower rate of major haemorrhages when they were used. Therefore, based on NCB analysis, DOACs are preferable to warfarin in AF in subjects with mild to moderate CKD (stage 2 or 3).
The phase 3 studies included subjects with normal kidney function and mild or moderate CKD (stage 2 or 3), very few cases of severe CKD (stage 4) and no cases of stage 5 or 5D CKD.
A recent prospective, randomised, open-label study that enrolled a limited number of patients (42–46/group) with CKD and non-valvular AF treated with HD compared the effects of three oral anticoagulation strategies (VKAs, rivaroxaban 10 mg/day and rivaroxaban 10 mg/day + vitamin K2) on the progression of cardioaortic calcium deposits (primary objective). After 18 months of follow-up, no significant intergroup differences were seen in terms of progression of CV calcifications. The number of severe haemorrhagic complications was significantly lower in those treated with rivaroxaban. However, the study had neither a suitable design nor suitable power for comparing CV or haemorrhagic events.65
In a retrospective study that enrolled subjects with CKD and AF treated with dialysis, both dabigatran (n = 281) and rivaroxaban (n = 244), compared to warfarin (8064), were associated with a higher risk of haemorrhage and death.66 However, analysis of an extensive database of patients with stage 4 CKD (n = 1349) or stage 5/5D CKD (n = 5395) and non-valvular AF and a follow-up of 1.5 years found that, following rigorous adjustment of baseline covariates (propensity score), patients treated with rivaroxaban (n = 1896) had a significant reduction (32%) [95% CI: 1–53%] in haemorrhagic complications compared to those treated with warfarin (n = 4848), with no differences in stroke or systemic embolism.67
Another observational study that compared apixaban to warfarin in subjects with CKD stage 4 (n = 197) or CKD stage 5D (n = 105) confirmed that those receiving apixaban had, as of six months of follow-up, less risk of haemorrhage (the risk of stroke/systemic embolism remained the same).68
An additional retrospective study of subjects with AF and CKD on treatment with HD69 compared warfarin (n = 23,172) to apixaban (n = 2351). Those treated with apixaban at doses of 2.5 mg/2 times/day had fewer major haemorrhages (HR: 0.72; 95% CI: 0.59−0.87) (p < 0.001) and a similar risk of stroke/systemic embolism (HR: 0.88; 95% CI: 0.69–1.12; p = 0.29), whereas apixaban at doses of 5 mg/2 times/day, compared to warfarin, reduced the risk of stroke/systemic embolism (HR: 0.64; 95% CI: 0.42−0.87; p = 0.04) and mortality (HR: 0.63; 95% CI: 0.46−0.85; p = 0.003).
The latter study, along with another study of rivaroxaban or dabigatran and 14 studies of warfarin versus no treatment, was included in a recent network meta-analysis which concluded that, in patients with AF on HD, oral anticoagulation was not associated with a lower risk of thromboembolism. In these patients, apixaban 5 mg/2 times/day reduced mortality. Warfarin, dabigatran and rivaroxaban were associated with a higher risk of haemorrhage than apixaban.70
However, other data have suggested similar efficacy and safety for rivaroxaban and apixaban in patients with stage 5 or 5D CKD. A retrospective analysis of 2623 subjects with non-valvular AF and stage 5 or 5D CKD did not find, following rigorous adjustment of baseline covariates, differences in terms of risk of stroke/systemic embolism or major haemorrhages among patients treated with rivaroxaban (n = 787) or apixaban (n = 1836). Most patients received standard doses of these DOACs.71
In summary, there are data from randomised studies showing a greater NCB for DOACs versus warfarin in mild to moderate CKD (stages 2 and 3) with non-valvular AF. There are no solid randomised studies on DOACs in stages 4, 5 or 5D. Observational studies have suggested that apixaban, and in some studies with rivaroxaban, may offer advantages over warfarin (fewer strokes/systemic embolisms and/or fewer major haemorrhages).
Despite the lack of specific studies in subjects with CKD and AF, the use of DOACs is common in these patients. A recent multinational registry that analysed the main factors that determine the choice of type of oral anticoagulant in patients with newly diagnosed non-valvular AF included 2623 subjects with stage 3–5 CKD. Of these, 45.8% were receiving treatment with DOACs.72
Effect of oral anticoagulants on kidney functionAcute kidney injury/nephropathy associated with anticoagulantsDOACs are safe and effective as anticoagulant therapy in subjects with mild or moderate CKD and AF. They are also safe and effective (with suitable dose adjustment) when kidney function is reduced once anticoagulant therapy is started.73
Acute deterioration of kidney function related to oral anticoagulant therapy merits special consideration. In 2009, a group from the University of Ohio published nine cases of acute kidney injury (AKI) in subjects treated with warfarin. Its clinical expression included not only elevation of serum creatinine, but also microscopic or macroscopic haematuria, absence of other causes of acute renal failure and, often, supratherapeutic INR. In terms of pathology, it was characterised by dysmorphic erythrocytes in the Bowman's space, tubular necrosis, tubular deposits of haemosiderin and intratubular haematic casts.74 All the cases featured different forms of underlying chronic nephropathy (three cases with IgA nephropathy). This condition was named "warfarin-related nephropathy" (WRN). Recently a case was published of nephropathy associated with acenocoumarol in a patient with AF, an INR of 6.2 and IgA nephropathy.75
Subsequent studies showed, in subjects treated with warfarin, with or without underlying CKD and with a rate of 16–33%, episodes of AKI associated with INR > 3 and no other apparent cause of acute kidney failure. These episodes were classified as WRN.76–78
It must be noted, however, given the inherent risk of kidney biopsy in subjects with elevated INR, that WRN was diagnosed clinically in most of those studies. AKI in this type of patient, in whom there is often a great deal of cardiovascular comorbidity, may be of another origin (HF, atheroembolism, gastrointestinal haemorrhage, onset of RAAS blockade, tubulointerstitial nephritis, obstruction by clots, etc.). Other comorbidities in addition to CKD, such as advanced age, DM, HTN and CVD, are risk factors for these episodes of AKI which, moreover, accelerate CKD progression and are associated with lower survival.76,79
There are also published cases of AKI linked to DOACs with clinical and pathological findings similar to those found in WRN.80–86 This has impelled replacement of the term WRN with “anticoagulant-associated nephropathy” (AAN). To our knowledge, seven cases of AAN associated with DOACs confirmed by renal biopsy have been published (Table 4). In all of them, AKI and pathology data corresponding to glomerular haemorrhage and tubular haematic casts were added to CKD (IgA nephropathy). As occurs with dicoumarols, there may be other causes of AKI linked to DOACs, including atheroembolism and tubulointerstitial nephritis.87,88
Published cases of acute nephropathy associated with anticoagulants (biopsied) in subjects treated with direct-acting oral anticoagulants.
| AgentRef. dose/indication | Age/sex | Baseline Cr (mg/dl) | Peak Cr (mg/dl) | Haematuria | Kidney biopsy |
|---|---|---|---|---|---|
| Dabigatran80 | 67/m | 0.53 | 3.6 | Macroscopic | -Intratubular haematic casts/diffuse tubular damage/interstitial haemorrhage/IgA nephropathy |
| 150 ⋅2/DVT | |||||
| Dabigatran81 | 69/m | 1.50 | 8.0 | >100 erythrocytes/field | -Intratubular haematic casts/interstitial haemorrhage/tubular necrosis/IgA nephropathy |
| 110 ⋅2/AF | |||||
| Dabigatran82 | 67/h | 1.00 | 5.5 | Macroscopic | -Intratubular haematic casts/diffuse tubular damage/IgA nephropathy |
| 150 ⋅2/AF | |||||
| Dabigatran83 | 78/m | 1.00 | 6.8 | Macroscopic | -Intratubular haematic casts/diffuse tubular damage/IgA nephropathy |
| 110 ⋅2/AF | |||||
| Dabigatran84 | 61/h | 0.98 | 4.7 | Macroscopic | -Intratubular haematic casts/tubular necrosis/IgA nephropathy |
| 110 ⋅2/AF | |||||
| Rivaroxaban85 | 75/h | 1.13 | 4.3 | Macroscopic | -Intratubular haematic casts/tubular necrosis/IgA nephropathy |
| 10 mg/day/AF | |||||
| Apixaban86 | 82/m | 3.26 | 8.2 | 20−50 erythrocytes/field | -Intratubular haematic casts/tubular necrosis/mesangial IgA deposits |
| 2.5 mg ⋅2/AF |
AF: atrial fibrillation; Cr: creatinine; DVT: deep vein thrombosis; F: female; M: male.
There are several possible pathogenic mediators of AKI in AAN: disruption of the glomerular filtration barrier promotes the passage of erythrocytes to the Bowman's space and the kidney tubules. Formation of haematic casts causes obstruction of and damage to the tubules. Haemoglobin has toxic effects on the kidney tubules and, after it is incorporated into tubular cells, haem and iron promote tubular damage secondary to the production of reactive oxygen species, oxidative stress, mitochondrial damage, apoptosis and the production of proinflammatory cytokines, among other things.89
The mechanism by which oral anticoagulants alter the permeability of the glomerular barrier and promote haematuria is not clearly understood. Some experimental models of AKI due to anticoagulants emulate what has been observed in cases of AAN.90,91 Administration of type 1 protease-activated receptors (PAR1) to animals in experiments has caused haematuria, tubular haematic casts and increased creatinine.91 Various PAR subtypes that may be activated by thrombin, factor Xa or activated protein C (aPC) are found in the endothelium, mesangium and podocytes, among other cells.92,93 It has been speculated that oral anticoagulants, by inhibiting thrombin, impede activation of PARs in the endothelium and thus increase the permeability thereof. Other experimental data, however, have shown that PAR1 activation by thrombin promotes an increase in glomerular permeability, inflammation and podocyte damage.94,95
The reason for this discrepancy is unknown. A dual and opposite effect of thrombin on endothelial permeability mediated by PAR1 activation has been demonstrated. At low concentrations, it decreases endothelial permeability, whereas at high concentrations, it increases it.96
aPC (activated by thrombin) may also play a role. Through stimulation of podocyte PAR3 and dimer formation with PAR2/PAR1, it prevents podocyte apoptosis.97
The elevated frequency of underlying IgA nephropathy confirmed in the majority of biopsied cases with AAN suggests a potentially mutually enhancing relationship between these two diseases. Supratherapeutic anticoagulation would induce an increase in the permeability of the glomerular barrier and haematuria, which would be more intense in the presence of underlying nephropathy. Haematuria, for its part, causes podocyte damage, exerts toxic effects on tubular cells and magnifies the inflammatory process of the underlying nephropathy.98
Most studies in subjects with AF that have compared warfarin to DOACs lack a suitable design as well as monitoring of creatinine with pre-specified intervals that would enable precise determination of AKI frequency. There are, however, several post hoc studies that have analysed AKI in subjects with AF treated with DOACs versus those treated with warfarin.99–103 As shown in Table 5, in most studies, treatment with DOACs was associated with a lower risk of AKI than warfarin.
Hazard ratio of acute kidney injury (AKI) in subjects with non-valvular AF treated with direct-acting oral anticoagulants (DOACs) versus those treated with warfarin.
| Ref. study | Patients (n) | DOACs | HR (95% CI) | Observations |
|---|---|---|---|---|
| Shin99 | 6412 | Overall | 0.79 (0.68−0.92) | -Greater reduction of risk of AKI in those with normal baseline kidney function |
| Dabigatran | 0.70 (0.52−0.66) | -56.7% of patients treated with warfarin had a TTR < 60% | ||
| Rivaroxaban | 0.83 (0.66−1.05) | |||
| Apixaban | 0.86 (0.68−1.10) | |||
| Chan100 | 7702 without CKD | Dabigatran | 0.62 (0.49−0.77) | -In those treated with warfarin, the risk of AKI increased as the CHA2DS2-VASc increased. In those treated with dabigatran, it remained stable |
| 2256 with CKD | Dabigatran | 0.56 (0.46−0.69) | ||
| Yao101 | 9769 | Overall | 0.68 (0.58−0.81) | -The group treated with warfarin with INR > 3 had a higher risk of AKI |
| Dabigatran | 0.55 (0.40−0.77) | -In all INR ranges, the risk of AKI was lower with DOACs | ||
| Rivaroxaban | 0.69 (0.57−0.84) | |||
| Apixaban | 0.84 (0.66−1.07) | |||
| Coleman102 | 74,599 | Rivaroxaban | 0.81 (0.75−0.81) | |
| Hernández103 | 21,682 with DM | Rivaroxaban | 0.83 (0.74−0.92) |
AF: atrial fibrillation; CKD: chronic kidney disease; DM: diabetes mellitus; TTR: time in therapeutic range.
Several observational studies and real-life analyses using an extensive database of subjects with variable follow-up and rigorous comparison of covariates (standardised absolute differences <0.1 [propensity score]), are more suitable for identifying a possible role of oral anticoagulants in the onset and progression of CKD (Table 6).101–105 Analysis of various parameters of kidney function (variation in CrCl, reduction of eGFR >25% or 35%, doubling of creatinine level and development of CKD stage 5 or initiation of dialysis) revealed that, in patients with AF, DOACs are more renoprotective than warfarin. The benefit was more obvious with rivaroxaban and dabigatran. Analysis of the subgroup of subjects with supratherapeutic doses of warfarin (INR > 3) revealed an even greater renal benefit on the part of DOACs.
Comparative studies of direct-acting anticoagulants versus warfarin on kidney function (CKD onset/progression).
| Fordyce104 | Bohm105 | Yao101 | Coleman102 | Hernández103 | |
|---|---|---|---|---|---|
| Patients (n) | 12,612 | 16,490 | 9769 | 72,599 | 21,682 |
| Follow-up time (months) | 21 | 30 | 11 | 20 | 20 |
| [0,1–6]Kidney parameters studied | |||||
| Δ eGFR (ml/min) | warf.: -4.30 ± 14 | warf.: -3.68 ± 0.24 | N/A | N/A | N/A |
| rivar.: -3.50 ± 15 | dab. 110 mg ⋅2: -2.57 ± 0.24a | ||||
| dab. 150 mg ⋅2: -2.46 ± 0.23a | |||||
| Drop in eGFR >25%: HR (95% CI) | dab. 110 mg ⋅2: 0.81 (0.69−0.96) | N/A | N/A | N/A | |
| dab. 150 mg ⋅2: 0.79 (0.68−0.93) | |||||
| Drop in eGFR ≥30%: HR (95% CI) | N/A | N/A | overall: 0.77 (0.66−0.89) | N/A | N/A |
| dab.: 0.72 (0.56−0.93) | |||||
| rivar.: 0.73 (0.62−0.87) | |||||
| apix.: 0.88 (0.70−1.10) | |||||
| Cr ⋅2: HR (95% CI) | N/A | N/A | overall: 0.62 (0.40−0.95) | N/A | N/A |
| dab.: 0.64 (0.30−1.34) | |||||
| rivar.: 0.46 (0.28−0.75) | |||||
| apix.: 0.80 (0.41−1.56) | |||||
| Development of stage 5 CKD/dialysis: HR (95% CI) | N/A | N/A | dab.: 0.45 (0.13−1.59) | 0.82 (0.74−0.91) | 0.82 (0.70−0.96) |
| rivar.: 0.63 (0.35−1.15) | |||||
| apix.: 1.02 (0.45−2.31) | |||||
apix.: apixaban; dab.: dabigatran; CKD: chronic kidney disease; eGFR: estimated glomerular filtration rate; HR: hazard ratio; N/A: not available; rivar.: rivaroxaban; warf.: warfarin.
The greater renoprotective effect of DOACs compared to warfarin may be based in its more predictable dose/response effect and lower risk of haemorrhages, the presence of fewer AKI events that might lead to progressive deterioration of kidney function and the possible anti-inflammatory effects of DOACs. Experimental models of hypertensive kidney damage mediated by AII have shown an increase in expression of PAR2 and of proinflammatory genes (TNFα, PAI y MCP-1) in podocytes. Treatment with rivaroxaban induced a reduction in PAR2 expression and in proinflammatory genes, as well as attenuation of podocyte structural abnormalities.106
Moreover, VKAs decrease vitamin K-dependent matrix Gla protein (MGP) activity, which may promote vascular calcification107 and calciphylaxis in subjects on dialysis. An increase in arterial stiffness secondary to arterial calcification promotes systolic HTN and an unbuffered increase in aortic pulsatility that is deleterious to the kidneys.108
The results of the Factor Xa Inhibition in Renal Patients with Non-valvular Atrial Fibrillation Observational Registry (XARENO) clinical trial will provide more precise information on the effects of oral anticoagulation on kidney function in subjects with non-valvular AF.109 The trial will analyse the effects on kidney function and on haemorrhagic and CV events in patients with CKD stage 3–4 (eGFR: 15−50 ml/m) and non-valvular AF of three oral anticoagulation strategies: rivaroxaban, VKAs or no anticoagulation.
Management of kidney function during oral anticoagulant therapyComparative studies of warfarin versus DOACs in patients with non-valvular AF have confirmed that deterioration of kidney function is very common. In a two-year period, approximately one in four patients has a drop in eGFR of at least 30%, and one in seven patients has an episode of AKI.101 This is very important, because the drop in kidney function is associated with a higher risk of stroke, haemorrhage and mortality.110
Moreover, changes in kidney function require adjustments of anticoagulant doses. The need for frequent monitoring of kidney function in these patients must be stressed. The guidelines propose monitoring of GFR every 6 months and more frequent monitoring in cases of CKD.11 It is recommended that the time in moths to follow patients is determined by dividing GFR by 10, as an empirical formula. This raises a question that we feel is important: how is kidney function determined? Phase 3 trials of DOACs have used calculated creatinine clearance (C–G), but in clinical practice are used formulas for estimating GFR (CKD-EPI and MDRD).
A study of 831 subjects with CKD and AF analysed the concordance between kidney function estimation with C–G and with CKD-EPI and MDRD. Concordance was confirmed in 64%, but in 29% of subjects, CKD-EPI and MDRD underestimated kidney function, which would lead to underdosing of DOACs. That study used MDRD and CKD-EPI results corrected to a standard body surface area of 1.73 m2, whereas CG was not corrected.111 However, another study showed that, compared to CG, both CKD-EPI and MDRD often underestimated kidney function, which would lead to overtreatment with DOACs.112 This discrepancy in new oral anticoagulant dosage regimens using different equations was greater in elderly patients with deterioration of kidney function and for dabigatran and rivaroxaban dosage regimens. In that study, both CKD-EPI and MDRD were corrected for actual body surface area. These results were consistent with those of another study in which CrCl with 24 -h urine was similar to that estimated by CG and inferior to eGFR by MDRD and CKD-EPI.113 Therefore, it is necessary to emphasise the limitations of formulas for estimating GFR, especially in older subjects, when adjusting doses of DOACs (if they are used, the difference compared to CG is reduced by correcting for actual body surface area). Dose adjustment of DOACs in patients with CKD is to be determined using CrCl estimated by CG.
Proposed anticoagulant therapy in chronic kidney disease with atrial fibrillation: authors’ opinion and rationaleThe proposals/recommendations of the updated guidelines on oral anticoagulant treatment of AF associated with CKD are imprecise and diverse (Table 7).
Declaration of guidelines on oral anticoagulation in chronic kidney disease (CKD) with associated atrial fibrillation (AF).
| Guidelines | Year/bibliographic reference | Proposal/Recommendation |
|---|---|---|
| KDIGO | International meeting, Berlin 2016/Eur Heart J 2018; 39:2314–232555 | -In moderate CKD with AF, DOACs are not inferior to warfarin, but they have a better safety profile |
| -In patients with CrCl 25−50 ml/min, apixaban and edoxaban cause fewer haemorrhagic events than warfarin, although, given the lack of studies directly comparing DOACs, no particular DOAC can be recommended in these patients | ||
| -There are no randomised trials of anticoagulation in CKD and AF with GFR < 15 ml/min or in dialysis. Low doses of apixaban or rivaroxaban can be considered until there are new safety data | ||
| European Society of Cardiology (ESC) | 2016/Eur Heart J 2016; 37:2893–296211 | -In moderate CKD with AF, DOACs, compared to warfarin, reduce the risk of stroke/systemic embolism and major haemorrhages |
| -Clinical trials comparing VKAs and DOACS must be conducted in patients with AF and CKD being treated with dialysis | ||
| American Heart Association (AHA) | 2019/J Am Coll Cardiol. 2019; 74:104–13254 | -In moderate or severe CKD with AF and elevated CHA2DS2-VASc, treatment with DOACs at limited doses can be considered (recommendation class IIb/level of evidence B–R) |
| -In patients with advanced CKD (CrCl <15 mL/min) or on dialysis with elevated CHA2DS2-VASc, it is reasonable to prescribe warfarin or apixaban (IIb/B-NR). Other DOACs are not advisable in these patients |
AHA: American Heart Association; CrCl: creatinine clearance; DOACs: direct-acting oral anticoagulants; ESC: European Society of Cardiology; GFR: glomerular filtration rate; KDIGO: Kidney Disease Improving Global Outcomes; VKAs: vitamin K antagonists.
Bearing in mind the current evidence of the benefits of DOACs in mild or moderate CKD with non-valvular AF, the absence of randomised clinical trials with oral anticoagulants in subjects with stage 4, 5 or 5D CKD, the data from observational studies in those subjects and the disadvantages of using VKAs in subjects with CKD, we believe the following proposal for anticoagulant therapy in patients with CKD and non-valvular AF seems reasonable. This proposal may be modified after the results of the current clinical trials in CKD with AF become available114–119 (Table 8).
Current clinical trials on oral anticoagulation in chronic kidney disease (CKD) with atrial fibrillation (AF).
| Trial/identifier/initialism/date accessed/status/ref. | Study population | Drugs compared | Primary objective |
|---|---|---|---|
| NCT02066662/03/05/2020/active, not recruiting114 | Subjects with AF and/or PE with eGFR >15 ml/min with coronary and/or valvular calcifications | VKA (phenprocoumon) (INR 2−3) versus | Progression of coronary/valvular calcifications (cardioTAC) |
| -AF: rivaroxaban 20 mg/day (eGFR >49 ml/min); 15 mg/day (eGFR 15−49 ml/min) | |||
| -PE: rivaroxaban 15 mg ⋅2/day from day 1 to day 21 and 20 mg/day from day 22 onwards | |||
| NCT02933697/AXADIA/03/05/2020/recruiting115 | Subjects with CKD on HD with non-valvular AF and CHA2DS2-VASc ≥2 | VKA (phenprocoumon) (INR: 2−3) versus apixaban 2.5 mg ⋅2 | Incidence of major and minor haemorrhages |
| NCT02942407/RENAL-AF/03/05/2020/finished116 | Subjects with CKD on HD with non-valvular AF and CHA2DS2-VASc ≥2 | VKA (warfarin) (INR 2−3) versus apixaban 5 mg ⋅2 | Incidence of major and minor haemorrhages |
| NCT02886962/AVKDIAL/03/05/2020/recruiting117 | Subjects with CKD on HD with non-valvular AF and CHA2DS2-VASc ≥2 | VKA (INR 2−3) versus no anticoagulation | Incidence of severe haemorrhages and thrombosis |
| NCT02039167/WatchAFIB/03/05/2020/finished118 | Subjects with CKD (with eGFR < 30 ml/min) with non-valvular AF and CHA2DS2-VASc ≥2 | LAAC (WATCHMAN device) versus VKAs (INR 2−3) | Incidence of major and moderate haemorrhages |
| NCT03446794 (WATCH-HD)/27/07/20/recruiting137 | Patients with non-valvular AF and CKD on treatment with haemodialysis | LAAC (WATCHMAN device) versus no intervention | Mortality, stroke and haemorrhages |
eGFR: estimated glomerular filtration rate; HD: haemodialysis; LAAC: left atrial appendage closure; PE: pulmonary embolism; VKAs: vitamin K antagonists.
In these patients, therapy with oral anticoagulants, preferably DOACs, must be considered, especially if the risk factor is DM or age 65–74 years.
Rationale. A risk factor for stroke unrelated to gender causes a significant risk of stroke and death. There are no randomised studies, but there are data showing a net benefit of oral anticoagulation in these patients.120 However, there is a great deal of heterogeneity, and therefore the decision must be based on individual characteristics, taking into account risk of bleeding and clinical factors determining an increase in thromboembolic risk. DM and age 65–74 years are the factors associated with a higher rate of thromboembolism.121 The presence of CKD, manifested by an increase in albumin excretion and/or mild or moderate reduction in GFR, would increase this risk even more.122,123
Although there are no controlled studies in these moderate-risk patients, DOACs, compared to warfarin, have demonstrated greater or equal efficacy with a lower haemorrhagic risk in subjects with stage 2−3 CKD and non-valvular high-risk AF.57,64 In addition, there are data suggestive of better preservation of kidney function with DOACs.101–105
Stage 2−3 chronic kidney disease and high thromboembolic risk (CHAD2DS2-VASc ≥2 in men and ≥3 in women)In these patients, treatment with oral anticoagulants (preferably DOACs; see Table 2) would be indicated.
Rationale. In subjects with CKD stage 3 and non-valvular high-risk AF, warfarin reduces the incidence of stroke and systemic embolism.35 In a study with a significant number of subjects with CKD and a CHAD2DS2-VASc of 4–5 (n = 13,435), warfarin, compared to those not receiving oral anticoagulation, reduced the combined incidence of embolic stroke, haemorrhagic stroke and death.124
In several meta-analyses including phase 3 studies of DOACs, patients with stage 2−3 CKD receiving DOACs presented fewer strokes and systemic embolisms and fewer major haemorrhagic complications (a positive NCB) than those receiving warfarin.60,61,64 The possible better preservation of kidney function with DOACs is another argument that would support a preference for DOACs over dicoumarols in these patients.
Chronic kidney disease stage 4 and 5In patients with CKD stage 4 or 5 and non-valvular AF, treatment with oral anticoagulants (preferably DOACs; see Table 2) should be considered.
Rationale. Very few patients with 5 CKD stage 4 or and AF are enrolled in controlled studies. However, we believe that these patients may benefit from anticoagulant therapy. In an observational study of subjects with CVD, AF and different stages of CKD (n = 1966 with CKD stage 4; n = 478 with CKD stage 5), warfarin significantly reduced mortality, readmission due to myocardial infarction and ischaemic stroke with no increase in haemorrhagic risk.125 Similar results were obtained in another observational prospective study of 8962 subjects with AF and different stages of CKD, including 341 patients with GFR < 30 ml/min/1.73 m2 (86% with CHAD2DS2-VASc >2).126 VKA treatment is associated with lower mortality and a lower incidence of ischaemic stroke and systemic embolism. At baseline, the percentage of subjects with elevated risk of bleeding (HAS-BLED ≥3) was higher in CKD stage 4 (38%) and CKD stage 5 (52%) compared to 12% in CKD stage 3 and 5% in CKD stage 2. An NCB (reduction in ischaemic stroke versus increase in haemorrhagic stroke) was seen. The NCB in those with a GFR < 30 ml/min/1.73 m2 was 6.69 (95% CI: 3.27–12.78).126
Observational studies in subjects with stage 4 or 5 CKD and AF have confirmed that rivaroxaban and apixaban compared to warfarin cause fewer haemorrhagic complications, with no differences in ischaemic stroke or systemic embolism.67,68 A recent meta-analysis of 43,850 patients with stage 4, 5 or 5D CKD found that, in most of those who were receiving oral anticoagulation for AF, apixaban was associated with a lower number of major haemorrhages than warfarin (OR: 0.27; 95% CI: 0.07−0.95), with no differences in thromboembolic complications.127
Patients with chronic kidney disease stage 5D (dialysis)In patients with CKD on dialysis, and non-valvular AF, at high thromboembolic risk (CHAD2DS2-VASc ≥2 in men and ≥3 in women), treatment with oral anticoagulants, Apixaban may offer advantages over VKAs in cases with a low time in therapeutic range (TTR), vascular calcifications or risk factors for calciphylaxis.
Rationale. Given the lack of randomised studies and the varied results with regard to the safety and efficacy of oral anticoagulation in patients with CKD and AF treated with dialysis, there is a great deal of debate as to its suitability. In studies that enrolled a high proportion of low-risk patients, VKAs did not have any significant benefits with regard to mortality or thromboembolic events.128 However, in subgroups of patients with CKD on dialysis with a high risk of thromboembolism, warfarin caused a significant drop in mortality and a non-significant reduction in the composite objective for death/stroke/systemic embolism/haemorrhages.37
In CKD treated with VKAs, there was a substantial reduction in TTR, which was associated with embolic and haemorrhagic events.40 Just 21% of patients on dialysis treated with warfarin had a TTR > 60%.129
An observational study and a meta-analysis demonstrated that, in subjects with CKD on dialysis and AF with elevated risk of thromboembolism (CHAS > 5), apixaban was associated with greater safety (fewer haemorrhages) than and similar efficacy to warfarin.69,70
Coronary and extracoronary calcifications are highly prevalent in subjects with CKD and are associated with CV mortality.130 Matrix Gla protein inhibits vascular calcification. Its action requires vitamin K-dependent carboxylation. VKA administration is associated with negative arterial and cardiac effects as well as coronary and extracoronary calcifications.131–133
Calcifying chronic arteriolopathy (calciphylaxis) is an uncommon but potentially fatal vascular disorder. Abnormalities of Phosphocalcic metabolism, DM and metabolic syndrome, among other things, together with VKA treatment, are risk factors for the development of calciphylaxis in patients with CKD on dialysis.134–136
If, after ruling out contraindications for anticoagulation and agreeing on the treatment with the patient, a decision is made to pursue oral anticoagulation, apixaban is a treatment option without the above-mentioned disadvantages and deleterious effects of VKAs. Apixaban was recently added to the American Heart Association/American College of Cardiology/Heart Rhythm Society (AHA/ACC/HRS) guidelines as a reasonable option for patients with AF and a high risk of thromboembolism with stage 5 or 5D CKD.54
Contraindications for oral anticoagulationCKD carries a higher risk of haemorrhage. When patients with CKD receive oral anticoagulation therapy, special attention must be paid to suitable treatment of all risk factors that may enhance bleeding (for example, there must be suitable monitoring of blood pressure and anaemia). Any treatable causes of haemorrhages present must be treated medically and/or surgically.
Oral anticoagulation must be avoided in patients with a history of cerebral haemorrhage and patients with recurring haemorrhages that cannot be treated. The guidelines consider left atrial appendage closure (LAAC) in patients with AF and a clear contraindication for long-term oral anticoagulation to be a possible treatment option.11 There are no randomised trials of LAAC in subjects with CKD. In an observational study of 1014 subjects enrolled in a multicentre registry of LAAC, a subgroup analysis of 375 subjects with CKD (stage 3, 4 or 5) found that LAAC is a safe and effective procedure for reducing stroke and haemorrhage risk in these patients.119 The NCT03446794 (WATCH-HD) clinical trial is currently under way. This trial will study the effects on mortality, stroke, systemic embolism and major haemorrhage of implanting the WATCHMAN® device to occlude the left atrial appendage in patients with CKD, treated with HD, and non-valvular AF with a high risk of thromboembolism and haemorrhage.137
Key concepts- 1
In CKD, there is a higher prevalence and incidence of AF, and these increase as the stage of kidney disease increases. The presence of AF in CKD increases the risks of stroke, CV events, mortality and progressive deterioration of kidney function.
- 2
Oral anticoagulation with dicoumarols in mild to moderate CKD (stages 2−3) with AF yields a net benefit. Results from randomised studies have shown a greater NCB for DOACs versus warfarin in non-valvular AF with mild or moderate CKD.
- 3
There are no solid randomised studies of oral anticoagulation in stage 4, 5 or 5D CKD with AF. Observational studies with warfarin in stage 5D CKD have yielded variable results. Often, subjects with CKD and AF treated with dicoumarols have deficient management of anticoagulation with a decreased TTR and a higher risk of haemorrhage. VKAs may promote vascular calcifications and are a risk factor for calciphylaxis. Observational studies have suggested that, in stages 4, 5 and 5D, apixaban and rivaroxaban may be safer and/or more effective than warfarin.
Given the higher risk of haemorrhage in CKD, special attention must be paid to monitoring of risk factors for bleeding (suitable monitoring of blood pressure and anaemia), and medical and/or surgical treatment of treatable causes of haemorrhage must be undertaken. Oral anticoagulation must be avoided and LAAC must be considered in patients with a history of cerebral haemorrhage and patients with recurring haemorrhages that cannot be treated.
Several randomised trials with VKAs, DOACs and LAAC currently under way will aid in guiding treatment decisions in patients with non-valvular AF and stage 5D CKD.
- 4
Treatment with dicoumarol, especially in cases of CKD and supratherapeutic INR, may be associated with AKI (nephropathy due to anticoagulants). This AKI increases the risk of stroke, haemorrhage and progressive deterioration of kidney function. DOACs may also cause nephropathy due to anticoagulants, especially in subjects with underlying nephropathy.
Some observational studies have suggested that, compared to warfarin, DOACs reduce the risk of AKI and of the onset/progression of CKD in patients with AF.
Deterioration of kidney function associated with an increase in CV events is often seen in patients with non-valvular AF. It is important to periodically determine kidney function (preferably using CrCl [CG]) to readjust doses of DOACs, which in different proportions are excreted through the kidneys.
None.
Please cite this article as: Gómez-Fernández P, Martín Santana A, Arjona Barrionuevo JD. Anticoagulación oral en la enfermedad renal crónica con fibrilación auricular. Nefrologia. 2021;41:137–153.