Introducción: En base a la premisa de que los pacientes portadores de catéteres tienen un peor pronóstico que los portadores de FAV, las guías de acceso vascular (AV) plantean unos objetivos ambiciosos (< 10% de Catéteres venosos tunelizados (CVT). En un intento de cambiar esta tendencia creciente en el uso de CVT iniciamos la “operación retirada de CVT”. Métodos: Al inicio del estudio 38 de los 173 pacientes dializados en la unidad lo hacían mediante un CVT (21.9%): 16 pacientes (42,1%) incidentes y 22 (57,8%) prevalentes. Se evaluaron aspectos físicos, psíquicos y vasculares de cada paciente portador de CVT. Se recogió edad, Indice de masa corporal, tiempo en HD, índice de comorbilidad de charlson (ICM), presencia de cardiopatía y diabetes mellitas, y número de AV previos. Tras 18 meses de seguimiento se evaluó la tasa de fallo primario, las complicaciones de la cirugía, el porcentaje de AV puncionables, el porcentaje de CVT retirados, la mortalidad y los ingresos hospitalarios Resultados: En 21 pacientes (55,2%) la decisión fue la no realización de un nuevo AV y el mantenimiento del CVT. En 9 pacientes por decisión del nefrólogo y familiares y en 11 por decisión del cirujano ante el agotamiento del lecho vascular. En 17 pacientes (44,7%) se realizó una FAV(50% incidentes y 45% prevalentes). La tasa de fallo primario fue del 0%. Se retiró el CVT al 64,7% (11/17). 18 meses después solo 4 pacientes permanecían sin CVT: 5 pacientes habían fallecido (4 con FAV funcionante y 1 con CVT tras ligadura de FAV por robo severo) y en 8 hubo que reintroducir de nuevo el CVT. Las complicaciones inmediatas de la cirugía vascular fueron: Un hematoma a tensión con necrosis de piel secundaria que requirió ingreso; dos síndrome de robo, uno que se solucionó con ejercicio y otro que precisó cierre quirúrgico; 2 infecciones, una en relación con hiperaflujo y trombosis de cava superior que precisó cierre quirúrgico. El tiempo medio libre de CVT fue de 5,2 meses (rango: 0,7- 14,3 meses).La mortalidad fue 29,4% (5/17) en el grupo en el que se actúo y 9,5% (2/21) en el otro grupo (RR 3,19; IC al 95%: 0,68-13,98; p: 0,11). Los pacientes a los que se realizó una FAV no mostraron diferencias significativas con el grupo al que no se le realizó una FAV en cuanto a edad, obesidad, Tiempo en HD, ICM, DM, sexo, nº AV, ingresos ni mortalidad. Conclusiones: Es posible mejorar la tendencia en el uso de catéteres permanentes, en un grado discreto y a lo largo de un proceso prolongado y no exento de complicaciones, algunas de ellas graves. En un porcentaje elevado de pacientes se confirma la imposibilidad de retirar el CVT. La patología asociada puede haber influido en los resultados. Los estándares de calidad deberían adecuarse a la realidad de la población que estamos tratando.
Introduction: In an attempt to reduce unnecessary tunnelled venous catheters (TVC) dependence in a prevalent population, a “TVC removal” programme was initiated in our unit. The objective was to diminish the number of TVC and to analyze the causes of their insertion and continuation. Methods: On 09/01/07, 38 out of 173 prevalent patients on haemodialysis were TVC dependant (21.9%), 16 incident patients (42.1%) and 22 (57.8%) prevalent patients. All of them were re-evaluated for placement of permanent vascular access including those previously rejected for surgery. Physical, psychic and vascular aspects of each patient were taken into consideration. The following variables were collected; age, body mass index (BMI), time on haemodialysis, Charlson Comorbidity Index, DM and vascular comorbidities and number of vascular accesses created prior to TVC placement. In those patients in whom AVF creation was feasible, after 18 months of follow-up the following parameters were evaluated: 1.Primary failure rate. 2. Surgical complications. 3. Percentage of usable AVF or AVG. 4. Percentage of removed TVC. 5. Mortality and hospitalization. Results: The decision not to carry out a permanent vascular access and to maintain TVC was made in 21 patients (55.2%). For 9 of them this was decided by the nephrologists and the family and for the remaining 11 patients, by the vascular surgeon after all vascular options were exhausted. A permanent VA was achieved in 17 patients (44.7%), 50% of them were incident patients and 45% prevalent patients. The primary failure rate was 0%. The TVC was withdrawn in 11 patients out of 17 (64.7%). Only 4 patients remained without TVC after 18 months of follow-up: 5 patients died (4 with AVF functioning and 1 underwent AVF ligation due to steal syndrome) and for 8 patients it was necessary to reintroduce the TVC again. Immediate complications after surgery were: 1 tense haematoma, complicated with skin necrosis, 2 infections and 2 steel syndromes with one requiring fistula ligation. Three patients required hospital admission following complications directly related to VA. The average time free from TVC was 5.2 months (range: 0.7- 14.3 months). The mortality rate was 29.4% (5/17) in the group of patients with a new VA and 9.5% (2/21) in the other group (RR 3.19; IC 95%: 0.68-13.98; p: 0.11). No significant differences were observed between patients who transitioned to a permanent vascular access and those who remained TVC in age, gender, BMI, time on dialysis, DM, comorbidity or number of previous VA attempts, hospitalizations or mortality. Conclusions: Permanent vascular access was possible in prevalent dialysis patients but this was achieved in a modest number of patients after a prolonged period and not without complications, some of which severe. The need for TVC dependence was confirmed in a high percentage of prevalent patients on dialysis. Comorbidity might have influenced the results. The quality standard should be adapted to the actual population on haemodialysis.
INTRODUCTION
It is generally accepted that AVF is the preferred vascular access in populations undergoing haemodialysis.1 It has been demonstrated that the use of catheters and vascular prostheses is an independent predictor of mortality.2 In addition, the use of catheters is associated with an increase in the risk of subsequent failure of ipsilateral vascular access3 and entails a higher economic cost.4 Nonetheless, and despite the proliferation in recent years of clinical practice guidelines which advise against its use, there is a growing trend in the use of catheters in most countries,5 and this trend is maintained and shows no sign being reduced.6 In a previous study carried out in our Unit we observed an increase in the use of permanent catheters, both in incident and prevalent patients, in spite of a policy in favour of native AVF being implemented by both the nephrologists and the vascular surgeons. In the year 2000 only 4.2% of our prevalent patients and none of the incident patients were dialysed using a catheter. However, five years later, in 2005, this percentage increased to 21.5% for prevalent patients and to 23.7% for incident patients (p < 0.0001).7 This trend has also been reported by others showing a higher probability of initiating haemodialysis with a catheter in 2002 compared with 1998.8
It is well known that there are significant differences between countries and centres regarding the prevalence of AVF, even when these have been adjusted for demographic characteristics6,9 and that specific initiatives to increase the number of AVFs has achieved good results (CIMINO).10 Our previous study5 indicated the possibility that the recent entry to dialysis programmes of increasingly elderly patients with increased levels of cardiovascular comorbidity and diabetes mellitus has hindered the implementation and maintenance of a working autologous vascular access. However, we should take into account the possibility that the ease of use of catheters due to the low level of technical skill required to insert them and the immediacy of their use after insertion, could dissuade us from attempting alternative vascular access, especially when the catheter used as a “bridge” (temporary access) was a TVC.
To assess this matter, and in an effort to avoid the unnecessary use of TVC, in the event that a TVC were present, we started the “Operation Catheter Removal”. The aim was to remove all the TVCs which were not mandatory in the prevalent population in haemodialysis and analyse the reasons for insertion and continuation of these TVCs.
METHODS
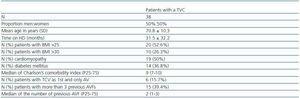
On 1 September 2007, a total of 173 patients were undergoing dialysis in our Unit, 38 of whom were using a TVC, corresponding to 21.9%. The average age of all patients in the Unit at the time of the study was 65.3 ± 14.5 years, and the average time in haemodialysis was 68.3 ± 65 months; 36.7% were women and 18.3% were diabetic. The median Charlson comorbidity index was 6 for incident patients and 8 for prevalent patients. The demographic characteristics of the patients fitted with a TVC at the beginning of the study are detailed in Table 1. Twenty-nine patients were aged over 65 years (76.3%); 13 of which, aged over 75, and 7 were aged over 80. 50% had some form of cardiomyopathy (three patients were fitted with valvular prostheses; three patients had moderate to severe valvulopathy and had not undergone surgery; four patients had an ejection fraction < 30%; two patients had ischaemic cardiomyopathy and had underwent coronary artery stenting; three patients had serious pulmonary hypertension; and four had hypertensive cardiomyopathy and moderate left ventricular hypertrophy [LVH]).
Our Dialysis Unit is subsidised by the Valencian Health Service and has its own surgeon, whose appointment waiting time is less than one week. Referral of patients to the centre is carried out by the referring hospital.
“Operation Catheter Removal” consisted of the reassessment of all patients fitted with a TVC, independently of age, comorbidity, number of previous AVFs or previous refusal by another surgical team to carry out vascular surgery for the creation of a fistula. A protocol was designed in which physical, psychological and vascular aspects were taken into account. The patients were assessed firstly by the Unit nephrologists, who reached a consensus on the decision; if the patient was considered as a candidate for surgery, he/she was subsequently assessed by the vascular surgeon together with the nephrologist. With regard to the decision to replace the TVC with an AVF, the baseline clinical condition of the patient was taken into account, the reason for the TVC having been fitted, the technical possibility of carrying out an AV and the individual preference of each patient or of the family. The follow-up period was 18 months.
The methods used for preoperative assessment of the vascular anatomy of the arm were: physical doppler ultrasound11 assessment and venography. The doppler ultrasound allowed the assessment of the distensibility and diameter of the vein and to determine whether the arterialized vein trajectory was homogeneous. If the trajectory was not homogeneous or there were images and flows compatible with possible stenosis, fistulography was carried out before a decision was made on the superficialisation of a venous trajectory, as well as to exclude central venous stenosis in suspected cases. The following variables were recorded in patients fitted with a TVC:
1. Age, sex, BMI, time on haemodialysis, presence of associated pathology (Charlson comorbidity index), cardiomyopathy and diabetes mellitus.
2. Number of vascular access prior to insertion of the TVC.
3. Reasons for insertion of the TVC.
4. Causes for an AVF not being carried out in cases in which it was not possible.
In patients who underwent AVF the following data was gathered:
1. Primary failure rate.
2. Complications due to the procedure.
3. Percentage of needling area of the fistulae and average time to maturity.
4. Percentage of TVCs removed.
5. Cause for failure of removal of TVC after 18 months follow-up period.
6. Admission to hospital.
7. Mortality.
STATISTICAL ANALYSIS
For statistical analysis, SPSS 12.0 for WindowsÆ software was used. The qualitative variables are shown as percentage, and the quantitative variables as mean ± standard deviation (SD). The comparison of quantitative variables was carried out using the Student-T test or analysis of variance (ANOVA) and for the qualitative variables, the Chi-square test.
RESULTS
At the beginning of the study, 38 patients of the Unit were fitted with a TVC (21.9%). Sixteen patients (42.1%) of which were incident patients who had been referred to our centre to initiate haemodialysis with a TVC from the referring hospital: in six of these cases (15.7%) the use of AVF had not been considered due to the characteristics of the patient and a TVC had been chosen as the first option for vascular access; three patients (7.8%) were referred after transplantation with a thrombosed fistula and who had had multiple previous vascular access, failed or thrombosed (> 3); in seven patients (18.4%) an AVF had been previously carried out (four primary failures, one failure to mature, one patient with a working AVF who refused needling and in another case it was necessary to ligate the AVF due to the development of severe steal syndrome).
Twenty-two patients (57.8%) were prevalent patients in our Unit, all with a history of multiple unsuccessful fistulae (median: 2.7 fistulae), in which a TVC was fitted as a last resort: one patient suffered from Marfan syndrome; in four of the patients, AVF ligation had been necessary (two due to steal syndrome, one due to severe venous hypertension distal to the fistula and another due to a complicated haematoma) and in 18 patients a TVC had been fitted following repeated thrombosis of the AVF.
In 21 patients (55.2%) the decision was made not to create a new vascular access and to keep the catheter. In six patients, this decision was taken by the nephrologist due to the patients’ clinical characteristics due to associated pathology or for social reasons (causes which affected the patient’s physical capacity and personal autonomy: amputation, hemiplegia or bone fractures with deformity of the side available for the formation of AV; and medical history of significant cardiomyopathy with EF < 30% or brain damage). In three cases it was due to the refusal of the patient or of the family due to old age or a bad experience of previous complications with vascular access, associated with comorbidity. In 11 patients the decision was made by the vascular surgeon due to the lack of vascular options: history of multiple thrombosed AVFs in seven patients, one with Margan syndrome and three with the absence of a pulse.
Fourteen patients of the total (36.8%) demonstrated their preference to keep the TVC as opposed to a fistula being formed.
Following assessment by the nephrologists and the surgeon, the decision was made to carry out an AVF on 17 patients (44.7%). This decision affected 50% of the incident patients (8/16) and 45% (9/20) of the prevalent patients. In Table 3, the characteristics of these patients are shown. The primary failure rate was 0%. The percentage of success, the removal of the TVC being considered as such, was 64.7% (11/17). Eighteen months after the launch of “Operation Removal”, only four of the patients whose TVC had been removed remained without it: five patients had died (four with a working AVF and one with TVC following ligation of the AVF due to the development of severe steal syndrome) and in eight the TVC had to be reinserted (Table 2). The complications immediately following vascular surgery were: an expanding haematoma with secondary necrosis of the skin which required admission to hospital in a patient who was being dialysed the same day of the surgery via TVC; two steal syndromes, one of which was resolved with exercise and another which required surgical closure; and two infections, one of which was associated with venous hypertension due to pre-existent thrombosis of the superior vena cava which became apparent after the AVF was formed. In the latter case, due to poor venous drainage a surgical closure was required (Table 2).
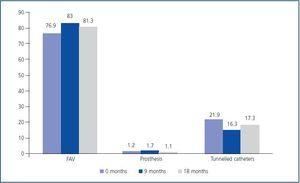
The median free TVC time of the patients in whom they were removed was 5.2 months (range: 0.7-14.3 months). The types of vascular access of the Unit in percentage of the actual dialysis population are shown in Figure 1.
During the study period, in the group on whom an AV was carried out, there were five serious cardiovascular events, four of which were in the first month following surgery, and 11 admissions to hospital, four immediately undergoing surgery and seven subsequently. Of the four admitted in the first month after surgery, one was related to vascular access and three were unrelated, with an average stay of 18 days. Of the admissions after one month following surgery, one was related to vascular access and the rest were unrelated, with an average stay of 23 days. One patient died due to congestive heart failure (CHF) 15 days after the fistula was carried out. Four patients died due to causes unrelated to the vascular access.
Mortality was 29.4% (5/17) in the group which were operated on and 9.5% (2/21) in the group on which AVF was not carried out (RR 3.19; CI 95%, 0.68-13.98; p = 0.11).
The group of patients on whom an AVF was carried out showed no significant differences from the group on whom on AVF was not carried out in terms of age, obesity (BMI), time on haemodialysis, comorbidity (Charlson comorbidity index), presence of DM, sex, being incident or prevalent, number of previous vascular access attempts, admissions to hospital or mortality (Table 3).
In addition, no significant differences were found between the group of patients who underwent surgery whose TVC was removed and those whose TVC was not removed.
DISCUSSION
This study demonstrates the difficulties which exist in attempting to reduce the numbers of patients fitted with permanent catheters in Haemodialysis Units. Based on the premise that patients fitted with a TVC are subject to a poorer outcomes and worse prognosis than those fitted with an arteriovenous fistula, the various guidelines for vascular access in existence set some ambitious targets for the achievement of vascular access in Haemodialysis Units. Studies have been carried out which demonstrate that initiating haemodialysis using a tunnelled catheter12 is associated with a relative risk of mortality of 1.3 compared with initiating dialysis with permanent vascular access. The use of catheters is an independent predictor of mortality and replacing a catheter with a fistula is associated with a reduction in the risk of mortality,13 of a magnitude similar to that attributed to an increase of Kt/V or haemoglobin level or the reduction of serum phosphorus.14
According to the latest guidelines for vascular access, published in 2005 in Spain, it is considered that the ideal percentage of dialysis patients with permanent catheters in a Unit should be less than 10% both in the incident and prevalent patients. However, the reality is quite different, and in recent years various studies have demonstrated a progressive increase in the use of central catheters for haemodialysis at the expense of the number of arteriovenous fistulae.6,8 This study aims to establish which factors are involved in this increase in the use of catheters, as well as to try and change the growing trend in the use of permanent catheters in haemodialysis, offering autologous vascular access as an alternative to all patients with a TVC to see if it was justified. Otherwise, there seems to be a certain “therapeutic nihilism”, considering the ease and immediacy of use and insertion of catheters.
The main drawback of this study is the inherent limitation to any analysis undertaken in one haemodialysis Unit alone, which prevents generalisation of the results (centre factor). However, in our opinion, its interest lies precisely in the description of habitual clinical practice in a typical Haemodialysis Unit.
Patients with a TVC displayed different demographic and clinical characteristics from the rest of the patients in the Unit: older in age, less time in haemodialysis, a greater proportion of women and diabetics, and a greater comorbidity index in relation with the median of the entire Unit, as well as a higher prevalence of serious cardiomyopathy and need for anticoagulation. These differentiating characteristics coincide with the description in the literature surrounding the greater usage of catheters in women,8,16 in people over 65 years of age and in patients with peripheral vascular disease or coronary artery disease,8,17 due to a higher percentage of failure of the AVF to mature in this class of patients.
Obesity was another characteristic of this patient subgroup, since over half were overweight with a BMI > 25 and over a quarter could be considered obese (BMI > 30). Although there are studies that demonstrate a reduced use of TVC in obese patients,8 needle access for dialysis in these patients entails greater technical difficulties, and requires venous superficialisation and lipectomy.
Contrary to reasonable belief, not all of the patients fitted with a TVC had a history of a long period in haemodialysis and multiple unsuccessful fistulae. Indeed, over 15% of cases were patients who had recently been admitted into the Unit, whose first and only vascular access had been a TVC.
Another interesting fact which has been unveiled by this study is that over half of the patients fitted with a TVC, despite their initial willingness to have the TVC removed and a fistula formed, chose to keep it and not to have new autologous vascular access. Although in the majority of cases the decision to keep the TVC was taken by the surgeon due to lack of vascular site options or due to vascular pathology which prevented the successful creation of a working fistula, in a significant percentage (45%) the decision was taken by the nephrologists, by the family or by the patient himself or herself, based on the associated pathology or social reasons which affected the patient’s physical capacity and personal autonomy. Indeed, many patients (36.8%) confirmed their wish and preference to continue with dialysis via TVC.
In those patients who opted for the creation of a new vascular access with the intention of removing the TVC, this aim was achieved in almost 65%, but after one year only four of the patients (23.5%) of this group retained working vascular access without the need for a TVC (five patients had died and in eight patients it was necessary to reinsert the TVC).
The successful vascular access was made via a humerocephalic fistula only in two cases: one patient on whom it had already been attempted previously but who refused needling (patient number 17), and a very obese patient (BMI 42.6) in whom a humerus-median fistula was fashioned which was inadequate for needle access of the deep vein, requiring superficialisation and additional lipectomy (patient number 5). For the rest of the patients, superficialisation of the basilic vein was required.
Indeed, the creation of a working AV is not sufficient; it is necessary for it to have needle access. Certain surgical techniques, such as transposition and superficialisation of the basilic vein, are an acceptable alternative for those patients in which it is not possible to carry out a humerocephalic fistula18,19 and, therefore, are an alternative option to vascular prosthesis or a catheter being fitted. Occasionally, the depth of the vein, although patent and adequately developed, proves impossible to needle or the access is limited to a small area, which eventually leads to the failure of vascular access. This situation is more frequent in the basilic vein, although it occasionally happens with the cephalic vein, especially in obese patients and patients with more subcutaneous tissue. This technique, from our experience, is an alternative to the fitting of prosthesis and has had good results.20 However, in this group of patients the results were worse than expected with regard to our previous series: three postsurgical haematomas, three early thrombotic complications (two of which were during hospital admissions and one following the dilatation of a subclavian artery stenosis) and two AVF closures due to steal syndrome and ischaemia of the hand. Upon admission, patients had other comorbid conditions and were in poorer health, the majority were anticoagulated both for maintenance of the catheter and for their basic cardiac pathology, as well as their poor vasculature, which entails greater technical difficulty. For this reason the thrombosis rate in this group is higher than the thrombosis rate in the Unit in general. Furthermore, all of these thromboses took place during admission to hospital. Given that the majority of possible access in this group required the superficialisation of the basilic vein, and this was performed close to their admission, it could lead to difficulties for hospital personnel unfamiliar with this type of vascular access. It would appear that, despite the attempts to convert TVC to fistulae, there is a high percentage of patients for whom, although this conversion is possible, the results do not last in the long term.
Over a quarter of the patients operated on died before the end of the year. There is no evidence that the cause of the deaths was related to the creation of the new vascular access. Indeed, one of the deaths was associated with the previous catheter (endocarditis), and there is the possibility in only one of the cases the death was related to the formation of the fistula, in a patient with cardiomyopathy. Although the number of deaths was greater in the group on which vascular access was implemented than in the group on which it was not, there were no significant differences between them, even though it is possible that the sample size may have prevented any statistical significance from being reached. Although there is a percentage of patients who can benefit from reassessment and the formation of new vascular access, the associated comorbidity, as well as inadequate vasculature, may have influenced the results. Therefore it is important to analyse in which population the higher technical, human and economic costs involved in implementing these measures would be justified. Although different studies indicate a reduction of mortality in patients in which a catheter was replaced by a fistula,13 it is likely that this depends on the reason for insertion of the catheter and the type of population in which this is indicated.
It appears likely, at least in part, that the increased risk of mortality attributed to catheters may be due to the relationship between its use and the increased age and comorbidity. However, there are various studies which attribute part of this mortality to the actual use of the catheter, either due to a state of chronic subclinical inflammation,21 or due to an inappropriate dose of dialysis.22 Whatever the case, we must concentrate our efforts on proposing the placement of autologous vascular access at an early stage, but it is important to weigh up the pros and cons at the time of proposing the creation of vascular access in a patient limited both by their age and their associated pathology and considering the added technical difficulties. Our study appears to confirm that although it is possible to improve the trend towards an increase in the use of permanent catheters, it is possible by a moderate degree, during an extended period and not without complications, some of which are serious. In addition there is a high percentage of patients from whom is not feasible to remove the TVC. In addition, in the CIMINO study, a programme to improve the quality of vascular access was possible by defining indicators and objectives; having periodic meetings; training and education syllabus, vascular access monitoring programme, which included a physical examination and monitoring of pressure and flow of the AV; designation of dedicated members of staff (the “vascular access nurse” as a key member of the implementation of the programme); and the formation of a multidisciplinary team involving a nephrologist, a surgeon and an interventional radiologist. Thanks to these measures, the percentage of autologous fistulae was increased in one year in incident patients by 3.5%, from 58.5% to 62.7%, as well as the use of vascular prostheses by 3.4%. However, the fitting of permanent catheters not only remained stable and did not fall, it even increased by a similar proportion to the placement of AVFs (4.3%).10
In light of these results, given that the increased creation of AVFs does not involve an effective AV in all patients nor a guarantee of safe removal of the catheter, and given that transitional period between the creation of the AVF until its effective use can last several months, it seems clear that efforts must be concentrated on making early provision for the placement of permanent vascular access, before initiating haemodialysis.23
One of the subjects currently under debate in various nephrology fora is whether the defined quality standards for vascular access should be changed to bring them more in line with reality, or to keep them as they are, with the idea of having a plan and an objective to achieve. Various studies have shown if an improvement in the attainment of arteriovenous fistulae is possible, the trend in use of catheters continues to increase. In the case in question, the attempts to remove TVCs only achieved the reduction of these by a small percentage, therefore there still exist a high number of patients whose special clinical characteristics, outside of the possible difficulties caused by the state of their vasculature, mean that the TVC is retained and the suggestion to fashion a fistula is not considered. To sum up, the quality standards give us a measure of what to aim for, but also they aid us in ascertaining if our results are “unacceptably” or “inevitably” high, and therefore the objectives must be both ambitious and reasonable, i.e. adapted to the population we are treating.
To conclude, it is possible to improve the trend in use of permanent catheters, but only by a moderate degree, over an extended process and not without complications, some of which are serious. In a high percentage of patients it proved unattainable to remove the TVC. Although comorbidity, age and the clinical situation of the patients make the placement of an autologous AV difficult, there is a percentage of them who can benefit from a reassessment, therefore a periodic systematic revision of all patients fitted with a TVC is advisable. The comorbidity of the patients may have influenced the results. Therefore it is important to analyse in which population the increased technical, human and economic cost which such measures involve would be justified. The quality standards must be appropriate to the reality of the population we are treating.
Table 1. Overall demographic characteristics of the patients with a TVC at the beginning of the study
Table 2. Types of vascular access performed and their evolution
Table 3. Comparison between those patients on whom a fistula was created and those on whom a fistula was not created.
Figure 1.