Previous reports have shown very high mortality among hemodialyisis patients. Our goal was to analyze the mortality of patients in the Renal Registry of Patients who remained exclusively on hemodialysis treatment.
MethodsThe cohort of patients who started treatment in the community of Castilla-La Mancha between 2010 and 2012 and remained on hemodialysis treatment was analysed until the end of 2017. Age, sex, primary kidney disease, vascular access, hemoglobin, Charlson index and serum albumin were included.
ResultsMortality rate was 63,4% after 5 years and 76% at the end of the study, with no difference between males and females, and was linked to an older age, urgent onset or in those with acute deterioration of chronic kidney disease, the use of catheters or albumin less than 3.5 g/dl.
ConclusionsMortality in patients who remain on hemodialysis is very high and is associated with non-modifiable factors such as age but also others that we can prevent or treat such as type of vascular access or nutrition status at the beginning of treatment.
Estudios previos han demostrado una elevada mortalidad de los pacientes en tratamiento con hemodiálisis aunque en pocos de ellos se analiza la supervivencia de los que reciben exclusivamente este tratamiento. Nuestro objetivo fue analizar la mortalidad de los pacientes que recibieron tratamiento con hemodiálisis.
MétodosSe analizó la cohorte de pacientes que iniciaron tratamiento sustitutivo entre los años 2010 y 2012 en la comunidad de Castilla-La Mancha y permanecieron en tratamiento con hemodiálisis. Se estudiaron las variables edad, sexo, enfermedad renal primaria, acceso vascular, hemoglobina, índice de Charlson y albúmina sérica al comienzo del tratamiento y se realizó un seguimiento hasta final de 2017.
ResultadosLa mortalidad fue del 63,4% a los 5 años y del 76% al final del periodo de seguimiento, sin diferencias entre varones y mujeres, y se relacionó con una mayor edad, el comienzo urgente o en aquellos con enfermedad renal reagudizada, la utilización de catéteres o una albúmina inferior a 3,5 g/dl.
ConclusionesLa mortalidad en los pacientes que permanecen en diálisis es muy elevada y se asocia a factores no modificables como la edad pero también a otros que podemos prevenir o tratar como el tipo de acceso vascular o el estado de nutrición al comienzo del tratamiento.
Patients with chronic kidney disease undergoing dialysis replacement therapy have a high mortality rate, which is higher than that of other pathologies such as cancer, diabetes, heart failure or stroke.1,2 According to the Spanish Dialysis and Transplantation Registry, global annual mortality was 8.2% in 2016, being higher in hemodialysis (15.2%) than in peritoneal dialysis (9.5%) or transplantation (2, 3%).3 An analysis on 60,615 patients between 2004 and 2015 showed that the 5-year overall survival was 57%, being similar in women and men and worse in diabetic patients, in those on hemodialysis versus peritoneal dialysis or transplant, and in patients with advanced age.3 The 2016 ERA-EDTA Registry showed that the adjusted 5 years probability of survival of patients that started dialysis between 2007 and 2011 was 45.5%.4 In short, the data from registries carried out in the past decade confirm that mortality is high, especially in prevalent hemodialysis patients compared to those on peritoneal dialysis or transplants. Several studies have analyzed the factors that can influence on this increased mortality; those studies must take into account the risk factors existing before starting the treatment and also the morbidity and mortality caused by hemodialysis. Among the former, there are non-modifiable factors such as age, sex and previous pathologies of the patients.5 From the point of view of prevention and treatment it is important is the study of modifiable factors, among which stand out the presence of arterial hypertension, diabetes mellitus, malnutrition, obesity, vascular calcifications, anemia, low adherence to treatment or type of vascular access.6–8 It is very important to take these into account these conditions since their treatment could reduce morbidity and mortality.5
The data from the registries, although very useful in evaluating survival, have some limitations, among which is the possibility that the patient, throughout his life, may change the modality of replacement treatment. Thus, it is common to observe that a kidney transplant patient returns to hemodialysis and the exchange between both dialysis techniques is also frequent. For these reasons, it is very interesting to analyze the survival of those who remain on the same treatment. It should also be taken into account that transplant patients or patients on peritoneal dialysis generally have different clinical characteristics from those who remain on hemodialysis, who tend to be older and have more comorbidities.
Our objective was to analyze through data obtained from the Registry of Renal Patients of Castilla-La Mancha (RERCLM) if certain factors present at the beginning of treatment are associated with higher mortality, limiting ourselves to those treated exclusively with hemodialysis.
Material and methods patientsOur study included the cohort of patients who started hemodialysis from January 1, 2010 to December 31, 2012 and remained on hemodialysis. Patients were followed until December 31, 2017. Patients transferred from other communities or who began in our community and moved to others were excluded. Those who were in treatment for less than a month or those who were lost to follow-up were also excluded.
MethodsThe following variables were studied:
- -
Age (categorized into the following groups: 15–44 years, 45–64, 65–74 and over 75 years).
- -
Sex.
- -
Primary kidney disease (classified according to EDTA codes).
- -
Previous risk factors.
- -
Initial indication for starting hemodialysis categorized as urgent in patient of wth unknown kidney pathology, urgent in patient with exacerbated chronic kidney disease or patient who starts hemodialysis on a scheduled basis.
- -
Type of vascular access at baseline: arteriovenous fistula, prothesis, indwelling tunnelled catheter or transient central catheter.
- -
Hemoglobin at the beginning of treatment (categorized as greater than or equal or less than 10 g/dl).
- -
Serum albumin at the start of treatment (categorized if it is greater than or equal or less than 3.5 g/dl).
We analyzed the probabilities of 96-month survival. The calculations are presented as life tables (actuarial method) and the graphs are presented using the Kaplan-Meier method. Hypothesis contrasts were performed with the log-rank test. A proportional hazards (Cox) regression model was performed to analyze the effect of albumin before starting treatment on the the variables included in the model: age, sex, vascular access, initial indication of treatment, primary kidney disease and index Charlson. An alpha error of 5% and a significance level of 95% were accepted in all tests.
We have used the statistical programs SPSS/PC + (version 22) and Stata (version 14).
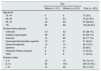
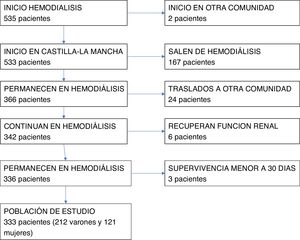
ResultsIn the years 2010–2012, 646 subjects began replacement treatment in the community (region) of Castilla-La Mancha. Of these, 535 began hemodialysis, 108 peritoneal dialysis, and 3 received an early kidney transplant. Fig. 1 shows the selection of study patients shown.
There were 333 patients included (212 men and 121 women). The clinical characteristics of the patients are shown in Table 1. The risk factors were arterial hypertension in 299 (89.8%), dyslipidemia in 184 (55.3%), diabetes mellitus in 172 (51.7%), heart disease in 151 (45.3%), vascular disease in 104 (31.2%) and neoplasia in 59 cases (17.7%). Regarding the type of vascular access at baseline, 131 had an arteriovenous fistula, 14 had a vascular prosthesis, 76 had an indwelling catheter, and 109 had a temporal catheter.
Clinical characteristics of the patients.
| Sex | |||
|---|---|---|---|
| Males (n = 121) | Women (n = 212) | Total (n = 333) | |
| Age group | |||
| 15−44 | 4 | 6 | 10 (3%) |
| 45−64 | 19 | 54 | 73 (21.9%) |
| 65−74 | 33 | 64 | 97 (29.2%) |
| 75+ | 65 | 88 | 153 (45.9%) |
| Primary kidney disease | |||
| Unknown | 3. 4 | 63 | 97 (29.1%) |
| Diabetic nephropathy | 36 | 61 | 97 (29.1%) |
| Vascular | 14 | 25 | 39 (11.7%) |
| Pyelonephritis/interstitial nephritis | 10 | 21 | 31 (9.3%) |
| Glomerulonephritis | 10 | 14 | 24 (7.2%) |
| Systemic | 6 | 14 | 20 (6%) |
| Polycystic Kidney Disease | 6 | 8 | 14 (4.3%) |
| Other | 5 | 6 | 11 (3.3%) |
| Charlson Index | |||
| 0−5 | 16 | 18 | 34 (10.1%) |
| 6−10 | 93 | 165 | 258 (77.5%) |
| > 10 | 12 | 26 | 38 (11.4%) |
Mortality was 63.4% at 5 years and 76% at the end of the follow-up period. Throughout the study, 162 men (76% of the total) and 91 women (75% of the total) died. The mortality by age group was: 40% (age group 15−44 years), 67.1% (group 45−64 years), 72.2% (age group 65−74 years) and 85% (age group over 75 years). No differences were observed between male and female mortality. The main causes of death were infectious in 51 cases (19.5%), cardiac in 46 (17.6%), exclusion of dialysis in 36 (13.8%), vascular in 29 (11.1%), cancer in 20 (7.7%) and not clearly determined in 45 patients (17.2%).
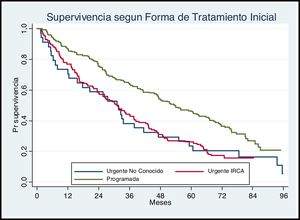
The Fig. 2 presents the observed survival in relation to the situation at the beginning of the hemodialysis treatment. Those who start hemodialysis urgently and their pathology was unknown or those who have exacerbated chronic kidney disease have higher mortality than those who start treatment on a scheduled basis (P < .05).
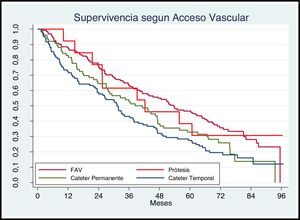
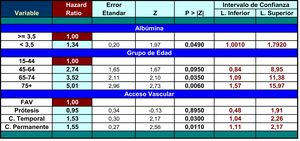
Regarding vascular access at the beginning of the technique Fig. 3 shows that patients with a fistula or prosthesis have a better survival than those who start treatment with a permanent or temporary catheter (P < .05).
In relation to baseline hemoglobin level, there were no differences in survival between patients who had hemoglobin lower (141 subjects) or higher (192 subjects) than 10 g/dl (data not shown).
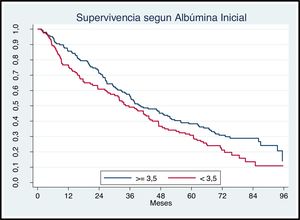
The survival of patients according to initial serum albumin concentration is shown in Fig. 4. Patients with serum albumin lower than 3.5 g/dl have a more mortality than those with the higher albumin (P < .05).
The results of the analysis of the multivariate regression model are shown in Table 2.
DiscussionOur results show that the mortality of patients who remained on hemodialysis treatment is very high. These data confirm the reports by other authors based mainly on registries and observational studies.9 However, in some countries it has been observed that in recent years there has been a decrease in mortality despite the fact that patients are older and have more comorbidities.2 Thus, according to the USRDS registry, the 5-year adjusted survival in patients who started hemodialysis in 2003 was 36.6%, while in the cohort that started in 2011 it was 42%.2 It has also been observed that mortality decreases in the second year and increase later, with the highest mortality 5 years after the start of treatment.10
Although the factors that condition higher mortality are not well known, there are some non-modifiable factors such as race, age, sex, or primary kidney disease. The age at which patients begin dialysis has progressively increased.11 In our series, 46% of the patients were over 75 years of age. When life expectancy has been compared between the general population and patients on dialysis, the differences are very significant: thus, as compared with subjects without kidney disease, dialysis patients under 80 years of age have a life expectancy one third lower and considering those over 80 the survival is reduced to half (that is, it falls from 7–8 to 2.7–3 years in the American population).2
Our interest has focused mainly on a series of modifiable factors that can be associated with higher mortality. Numerous studies have shown factors on which we can act that influence survival.12,13 Thus, renal function at the beginning of hemodialysis, the hemodialysis technique, avoiding hypotensive episodes, maintaining an optimal time and an adequacy of analytical parameters clearly influence the prognosis.6,14 In addition, other factors such as control of risk factors (hypertension, diabetes, dyslipidemia, etc.), adherence to prescribed drug treatments and control of different parameters (secondary hyperparathyroidism, anemia, lipids, etc.) also influence morbidity and mortality.7,15,16 Finally, the quality of life, socioeconomic situation or tendency to depression should also be considered.17
Our study analyzes the possible association between the clinical situation of patients when starting replacement therapy with hemodialysis and mortality. We found no differences regarding sex or hemoglobin. It is likely that the use of erythropoiesis stimulating factors prevent a severe anemia at the initiation of hemodialysis. However, we observed that patients who started hemodialysis urgently or with exacerbation of their chronic kidney disease had higher mortality. This fact has been confirmed in other studies and should make us work even more on the early detection and scheduled referral of patients with chronic kidney disease to Nephrology consultations.
Our data reflect that patients who start hemodialysis with catheter have higher mortality. It has been confirmed by several authors that the use of catheters carries an increased risk of complications, both infectious and non-infectious and this is associated with increased morbidity and mortality.18 However, Ravani et al.,18 using data from the DOPPS study between 1996 and 2011, postulated that complications related to the catheter do not justify the increase in mortality and advanced the plausible hypothesis that patients with catheters have other unrelated confounding factors that denote greater severity or associated comorbidities. This hypothesis has also been suggested in other studies.19 In any case, the “fistula first” initiative has been widely accepted to reduce the risk of complications related to vascular access, the number of hospitalizations and the cost.20
Finally, we show that plasma albumin less than 3.5 g/dl at the beginning of hemodialysis treatment is associated with higher mortality. Although it has its limitations, albumin has been considered a simple and reproducible nutritional marker and our data could suggest that patients with a worse prognosis have initial malnutrition. Several studies have also demonstrated this association in patients undergoing hemodialysis. Thus, Chen et al. evaluated 781 hemodialysis patients and observed that those with an albumin lower than 3.5 g/dl had a higher mortality and that the risk was higher as the albumin level decreased.19 It has also been suggested that a decrease in albumin may be associated with other pathologies that increase mortality, such as sarcopenia, chronic inflammation, or volume overload.19
Our study has the strength that the patients in the cohort remained on hemodialysis throughout the follow-up time, unlike others that analyzed mortality taking into account only the last form of treatment. However, we recognize that it also has some limitations since we have not analyzed other factors that may influence mortality, including the hemodialysis technique used, the psychosocial situation, adherence to treatment or the presence of other comorbidities such as inflammation. chronic or vascular calcifications.
ConclusionsIn short, patients who remain in hemodialysis treatment have a high mortality, and this is associated with factors that can be treated, such as the type of vascular access at the beginning or the serum albumin level.
Conflict of interestsNone.
We are grateful for the participation of all the professionals who have sent the data to the Castilla-La Mancha Registry of Renal Patients, as well as the collaboration of the Castilla-La Mancha Department of Health. We also appreciate the pioneering role in the registry of Dr. Tomás Sierra Yébenes and Dr. Isabel Ferreras García.
Please cite this article as: de Arriba G, Avila GG, Guinea MT, Alia IM, Herruzo JA, Ruiz BR, et al. La mortalidad de los pacientes en hemodiálisis está asociada con su situación clínica al comienzo del tratamiento. Nefrologia. 2021;41:461–466.