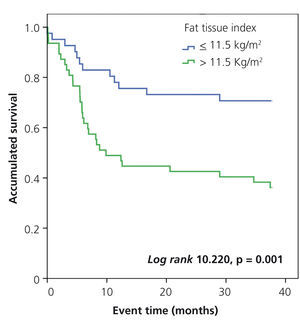
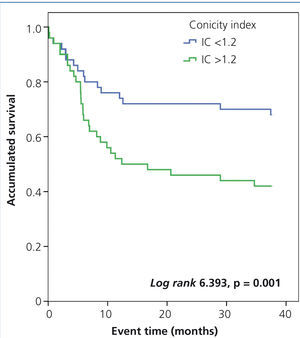
Antecedentes: El síndrome metabólico (SM) es un factor de riesgo cardiovascular y de mortalidad en la población general y en pacientes con enfermedad renal crónica. Sin embargo, apenas se ha estudiado en pacientes en hemodiálisis (HD). Objetivos: El objetivo del estudio es analizar el efecto del SM sobre la aparición de eventos cardiovasculares en HD. El objetivo secundario es determinar la influencia del índice de tejido graso y del índice de conicidad en los eventos cardiovasculares. Métodos: Estudio prospectivo en el que se incluyeron 100 pacientes en HD. El tiempo de seguimiento es de 3 años. Se recogieron eventos cardiovasculares y mortalidad. Se definió SM según los criterios de ATPIII e IDF. Resultados: La prevalencia del SM definido por ATPIII es 32 % y por IDF 29 %. La concordancia entre las dos definiciones es elevada (índice kappa 0,79, intervalo de confianza 95 % 0,65-0,92). El riesgo de desarrollar un evento cardiovascular es mayor en pacientes con SM (log rank 6,185, p = 0,013), con índice de tejido graso mayor 11,5 kg/m2 (log rank 10,220, p = 0,001) y con índice de conicidad mayor 1,2 (log rank 6,393, p = 0,011). En el análisis de Cox, ajustado a la edad y sexo, los pacientes con SM tienen el doble de riesgo de ingresar por un evento cardiovascular (odds ratio 1,93, 1,022-3,6, p = 0,043). La mortalidad fue 35 % en los 3 años de seguimiento sin diferencias entre los grupos con y sin SM. Conclusiones: El SM es una patología muy prevalente en pacientes en HD y su presencia duplica el riesgo de hospitalización por eventos cardiovasculares a corto plazo.
Background: Metabolic syndrome (MS) is a cardiovascular risk factor and is associated with mortality in the general population and in patients with chronic kidney disease. However, few studies have been carried out in patients on haemodialysis (HD). Objectives: The objective of the study is to analyse the effect of MS on the occurrence of cardiovascular events in HD. The secondary objective is to determine the influence of the fat tissue index and conicity index on cardiovascular events. Methods: A prospective study including 100 patients on HD. The follow-up period was 3 years. Cardiovascular events and mortality were recorded. MS was defined in accordance with ATPIII and IDF criteria. Results: MS prevalence as defined by the ATPIII was 32%, and by the IDF, 29%. The concordance between the two definitions was high (kappa index 0.79, 95% confidence interval 0.65 to 0.92). The risk of cardiovascular events was higher in patients with MS (Log Rank 6.185, p = 0.013), with a fat tissue index greater than 11.5 kg/m2 (log rank 10.220, p=.001) and a conicity index greater than 1.2 (log rank 6.393, p=.011). In the Cox analysis, adjusted for age and sex, patients with MS had twice the risk of being admitted due to a cardiovascular event (odds ratio 1.93, 1.022 to 3.6, p=.043). Mortality was 35% in the 3 year follow-up period with no differences between the groups with and without MS. Conclusions: MS is a very prevalent disease in HD patients and its presence doubles the risk of hospitalisation due to cardiovascular events in the short term.
INTRODUCTION
Metabolic syndrome (MS) is defined by a set of factors in the same individual that increase the risk of suffering from cardiovascular disease or diabetes mellitus. It is characterised by resistance to insulin and compensatory hyperinsulinaemia associated with carbohydrate metabolism disorders, high blood pressure (HBP), lipid disorders and obesity.
MS is a risk factor for cardiovascular disease and mortality in the general population1,2 and in patients with chronic kidney disease.3 However, there are few data in the literature regarding its prevalence in haemodialysis (HD) patients and very few studies analyse its prognostic implications.
The conicity index (CI)4 has been used to assess the degree of abdominal adiposity. The index values range from 1 (cylinder) to 1.73 (double cone). The cut-off point from which the risk of cardiovascular disease increases in the general population is not well-established and it is even less so in HD patients.
The main objective of the study was to analyse the effect of MS on the occurrence of cardiovascular events after 3 years of follow-up in HD patients. The secondary objectives were to determine the influence of the fat tissue index (FTI) and the CI on the development of cardiovascular events in these patients.
METHODS
A prospective cohort study including 100 prevalent HD patients, of whom 60% were male, with a mean age of 60.6±16.5 years of age at the start of the study, which had been on renal replacement therapy for 8.9±9.6 years. 39% of patients had received a kidney transplant. 34% of patients were diabetic (DM) and 83% had high blood pressure. The follow-up time was 3 years, from January 2009 to January 2012.
Cardiovascular events and mortality
We prospectively recorded admissions due to cardiovascular events (ischaemic heart disease, arrhythmia, congestive heart failure, stroke or peripheral vascular disease) and mortality in patients classified in accordance with the presence or absence of MS.
We also collected demographic data, medical history, laboratory data and comorbidity data measured using the Charlson index. We measured resistance to insulin with the HOMA index.5 We used the CI4 to assess the degree of abdominal adiposity. We carried out a bioimpedance spectroscopy analysis (BCM®, FMC) to determine body composition.
Definition of metabolic syndrome
MS was defined in accordance with the National Cholesterol Education Program Adult Treatment Panel III (NCEP ATPIII)6 and the International Diabetes Federation (IDF) criteria.7
In 2001, the third NCEP ATPIII report defined MS as the presence of 3 out of 5 clinical criteria: 1) waist circumference ≥102cm in males or 88cm in females, 2) triglycerides ≥150mg/dl, 3) HDL cholesterol <40mg/dl in males or 50mg/dl in females, 4) blood pressure ≥130/85mmHg and 5) glycaemia >110mg/dl. In 2005, the IDF proposed new criteria, similar to those of ATPIII, but with central obesity being considered as a necessary condition for the diagnosis of MS.
Statistical analysis
We divided patients in accordance with presence of MS as defined by the NCEP ATPIII. We analysed the concordance between the two definitions using the kappa index. We determined MS risk factors (as defined by the ATPIII) with the logistic regression analysis. We performed a Kaplan-Meier analysis to study the influence of MS, FTI and CI on the occurrence of a cardiovascular event. We divided the patients into 2 groups in accordance with the presence or absence of MS and in accordance with the FTI and CI medians. We subsequently carried out a Cox regression analysis to determine risk factors associated with the occurrence of the first cardiovascular event.
Continuous variables were expressed as the mean ± standard deviation and the categorical variables were expressed as a percentage of the number of cases. The continuous variables of the two patient groups (with and without MS) were compared out using the Student’s t-test and the χ2 test was used for categorical variables. The data were presented as odds ratios (OR) with 95% confidence intervals (95% CI). The analysis was carried out using the SPSS 18.0 statistical software for Windows.
RESULTS
Cohort characteristics
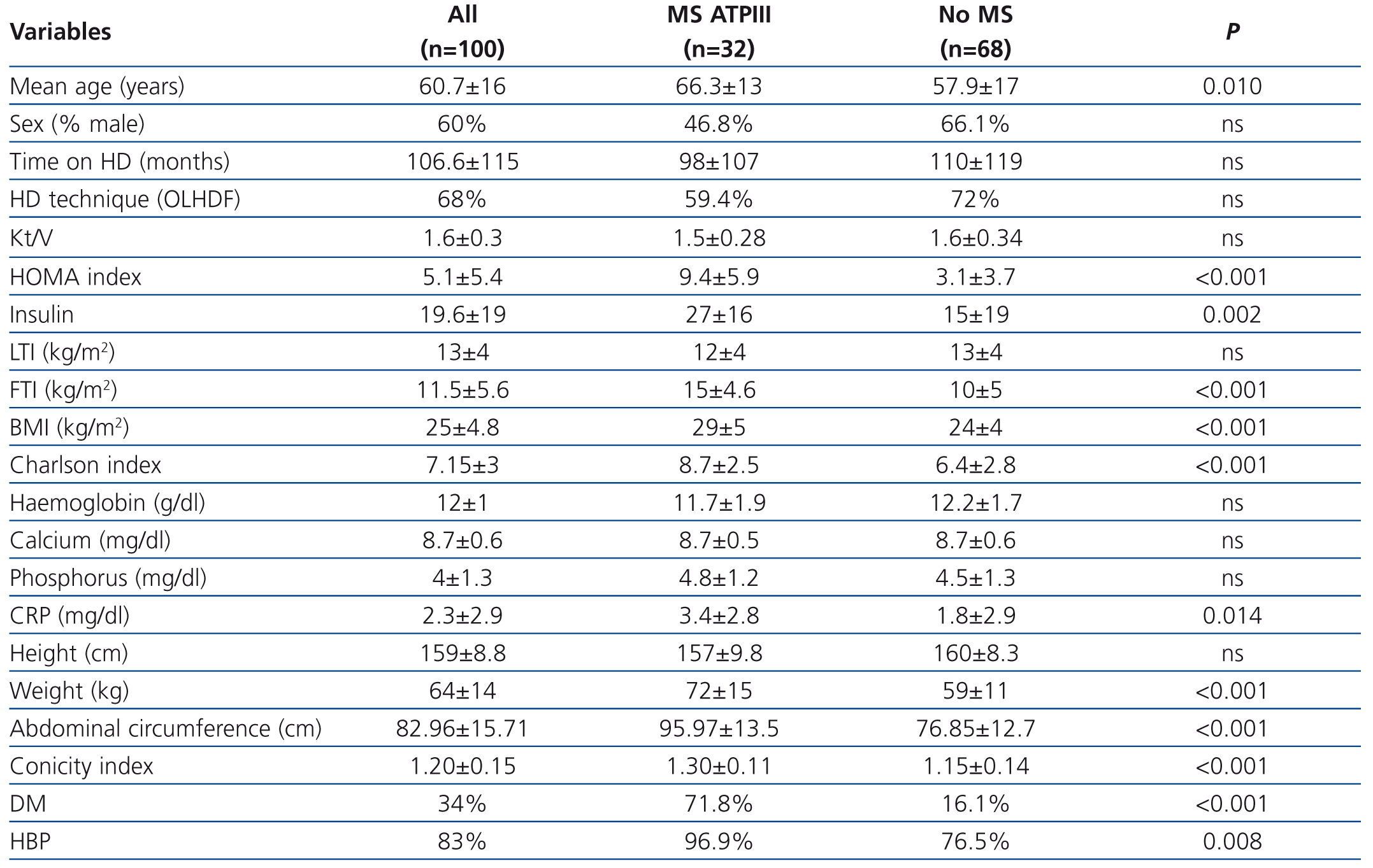
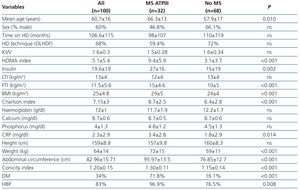
The baseline characteristics of the cohort studied, in accordance with the presence or absence of MS, are displayed in Table 1. The most common cause of renal failure in the cohort was glomerular disease (29%, n=29), followed by diabetic nephropathy (19%, n=19). The presence of a kidney transplant did not affect MS occurrence, the FTI or the CI. During the 3-year follow-up period, 2 patients were transferred to other hospitals, 8 patients received transplants and 35 died.
Presence and risk factors of metabolic syndrome
The prevalence of MS as defined by the ATPIII was 32% (n=32), and by the IDF, 29% (n=29), without significant differences between both. The concordance between the two definitions was high, with a kappa index of 0.79 (95% CI 0.65-0.92).
In the univariate analysis, we found that MS patients were older and had higher comorbidity, measured by the Charlson index. MS patients had a higher CI and their body mass index (BMI) was significantly higher due to a higher FTI, without significant differences being observed in the lean tissue index. Acute-phase reactants, measured by C-reactive protein (CRP), were higher in the MS group and the prevalence of HBP and DM was also higher.
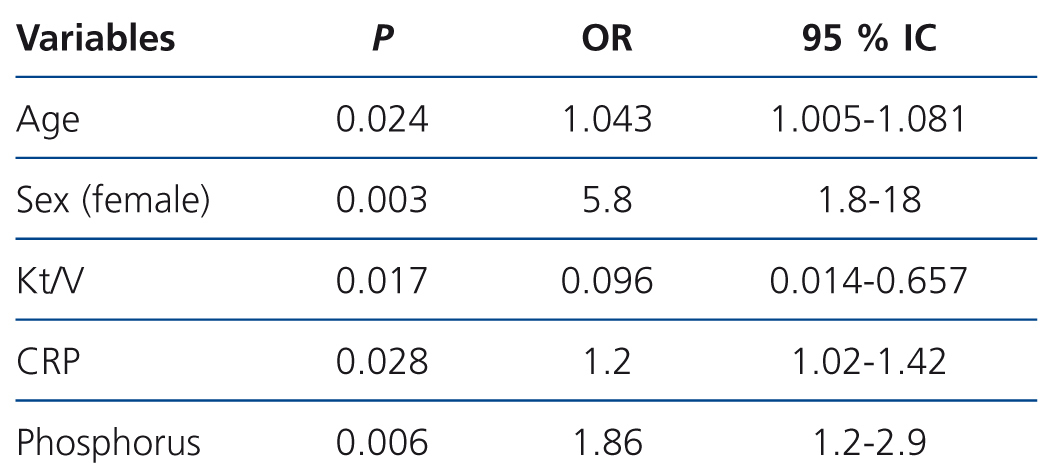
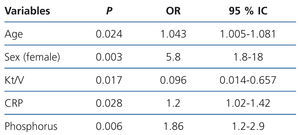
We performed a backward multivariate logistic regression analysis, in which we initially introduced the following variables: age, sex, time on HD, Kt/V measured by ionic dialysance, CRP and phosphorus. These variables were selected as they were significant in the univariate analysis or because they were clinically relevant. We found that the independent risk factors associated with MS as defined by ATPIII were old age, female sex, a lower Kt/V, hyperphosphataemia and increased CRP (Table 2). MS was not associated with time on renal replacement therapy.
Association between cardiovascular events and metabolic syndrome
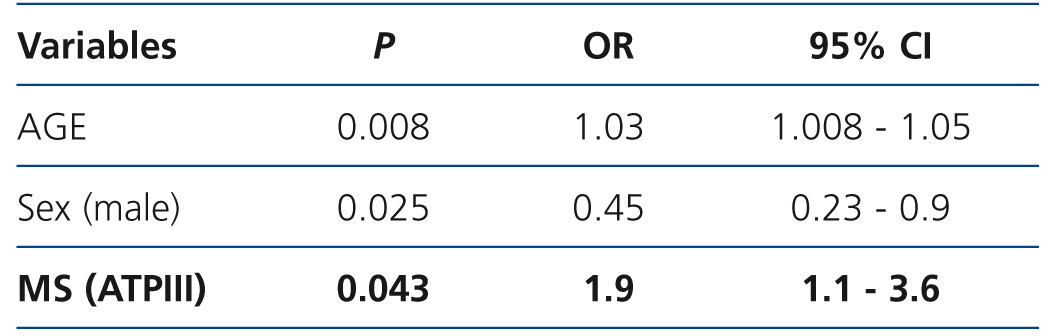
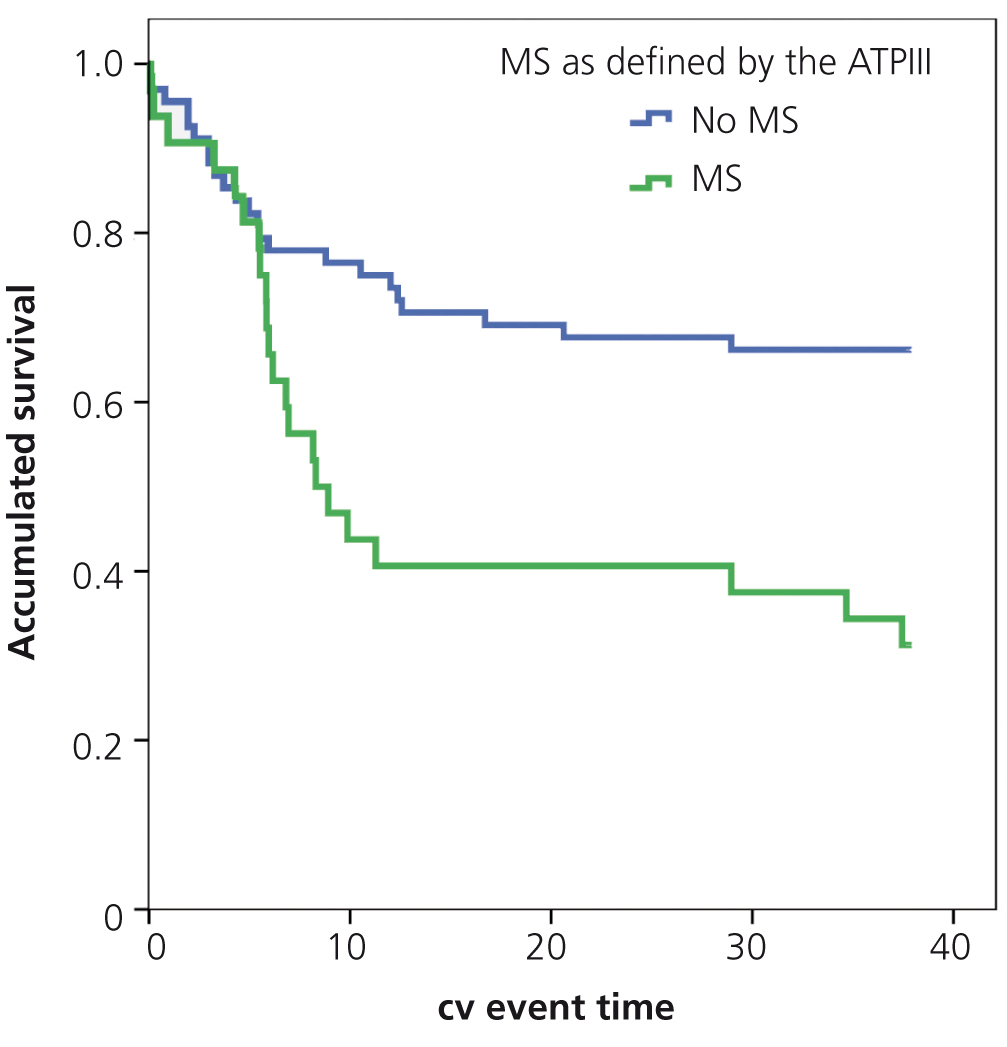
During the 3-year follow-up period, 22 patients with MS as defined by the ATPIII (22/32 patients with MS, 68.8%) and 23 patients without MS (23/68 patients without MS, 33.8%) were admitted due to a cardiovascular event.
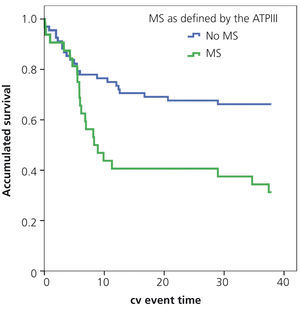
In the Kaplan-Meier analysis, the risk of a cardiovascular event was higher in MS patients (log rank 6.185, p=.013) (Figure 1).
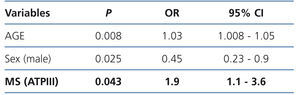
In the non-adjusted Cox regression analysis for cardiovascular events during follow-up, MS patients had a higher risk of being admitted due to a cardiovascular event (OR 2.15, 95% CI 1.2-3.9, p=.015). On adjusting the Cox analysis for age and sex (Table 3), MS patients were still twice as likely to be admitted due to a cardiovascular event (OR 1.93, 95% CI 1.022-3.6, p=.043), which reinforces the non-adjusted analysis results.
Association between cardiovascular events and the fat tissue and conicity indexes
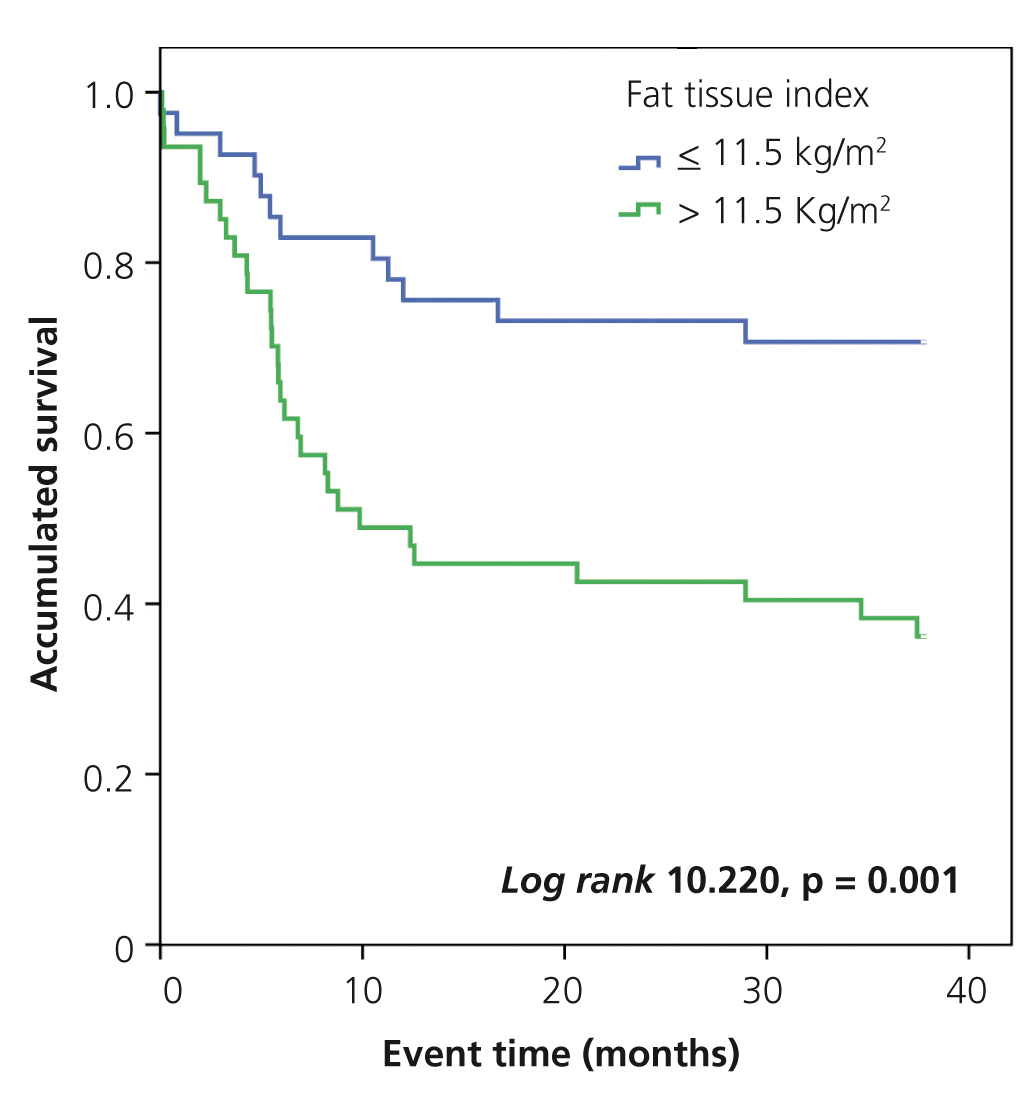
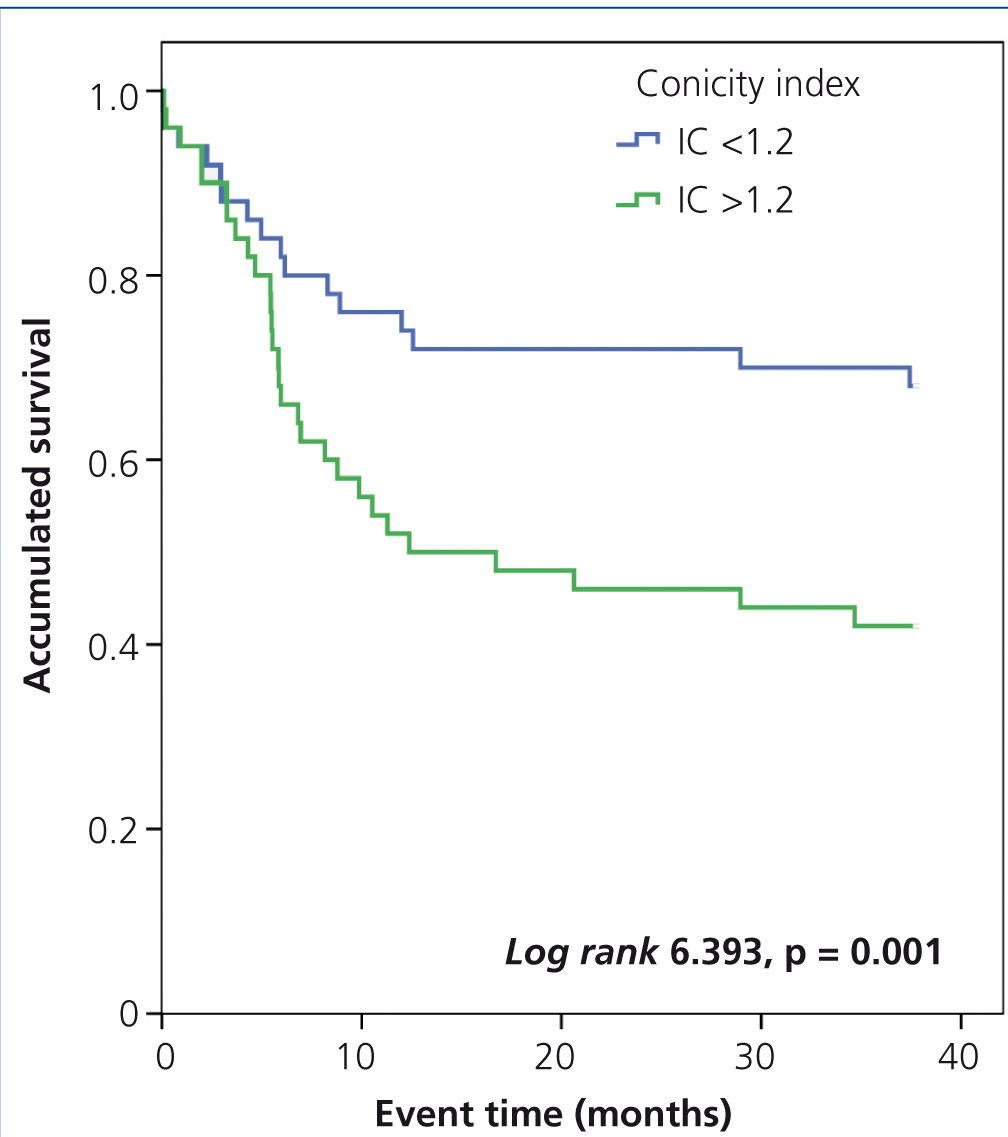
In the Kaplan-Meier analysis, we observed that the risk of a cardiovascular event was significantly higher in patients with a FTI greater than or equal to 11.5kg/m2 (log rank 10.22, p<.001) (Figure 2) and a CI greater than 1.2 (log rank 6.393, p<.011) (Figure 3).
During the 3-year follow-up period, 35 patients died (35%), 16 (50%) in the MS group and 19 (27.9%) in the group without MS (OR 2.58, 95% CI 1.1-6.2, p=.027). However, in the Kaplan-Meier analysis, we did not find significant differences in mortality between the two patient groups.
DISCUSSION
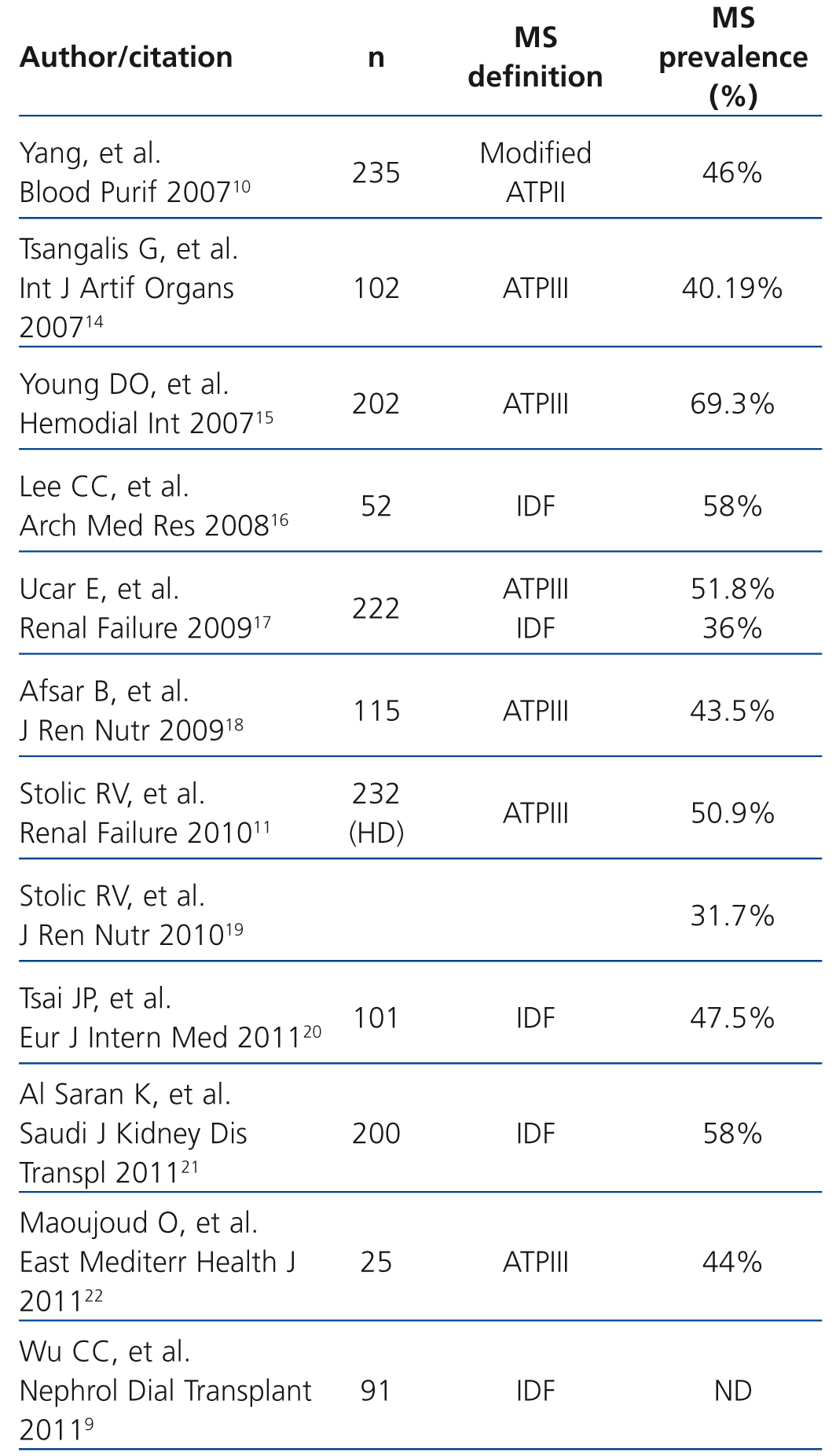
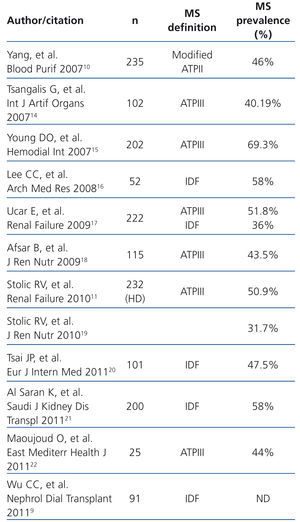
Our study shows that MS is very prevalent in the HD population; it affects one third of the population studied and is an independent risk factor for cardiovascular events in HD patients. This is a prospective study in which MS was defined by the ATPIII and the IDF and with a body composition analysis measured by bioimpedance spectroscopy. MS prevalence in patients on HD was 32%, similar to figures published in other series, which range between 30% and 70% (Table 4). It can be assumed that differences in MS prevalence may depend, amongst other factors, on the definition of MS that is used. However, the concordance found between the two definitions was high, and as such, it is necessary to find other explanations to justify the difference in prevalence in the different studies, which is probably linked to differences in age, sex, dialysis dose and prevalence of obesity in the different populations studied. These two definitions reflect the importance of abdominal fat in the genesis of MS, since they define obesity by a waist circumference greater than 102 in males and 88 in females, and not by BMI. The only difference between the two definitions is that that proposed by the IDF in 2005 considers central obesity as a necessary condition for MS to be diagnosed. However, in view of the high level of concordance, either of the two definitions is valid in HD patients.
Risk factors included in the definition of MS are very prevalent in HD patients, which explains its high prevalence. The purpose of measuring the parameters constituted by MS is to identify high-risk patients, in order to establish therapies to decrease the incidence of cardiovascular disease and mortality.
In this study, female sex, old age, a lower dialysis dose, hyperphosphataemia and inflammatory condition measured by an increase in CRP are risk factors for MS, and as such, cardiovascular events. However, MS is not associated with time on HD. CRP is significantly higher in the MS patient group, suggesting a worse inflammatory condition, which is one of the key components of MS. This association between inflammation and MS may explain the higher tendency for patients to develop atherosclerosis and cardiovascular disease.8
The presence of MS as defined by the ATPIII, is an independent predictor of cardiovascular events in HD patients. However, in the 3 years of follow-up, we did not find significant differences in mortality between patients with and those without MS on HD. These results are similar to those published by Yang et al. and Wu et al.9,10 in a prospective study on a cohort of Asian patients on HD. These authors defined MS by modified ATPIII criteria and they found no differences in mortality between patients with and those without MS, but they did observe a higher admission rate due to all causes in the patient group with MS (relative risk 1.67). Stolic et al.11 studied 407 patients, 232 on HD and 175 on peritoneal dialysis (PD) with a 4-year follow-up and they found that MS did predict mortality in HD patients, but not in PD patients in the 4 years of follow-up. In our study, we did not find differences in mortality in the 3 years of follow-up. This may be due to the short follow-up period, since malnutrition is associated with short-term mortality, while overnutrition is associated with long-term mortality. However, the role of obesity in the progression of HD patients continues to be unclear. Some studies, such as that of Abbott et al.12, which was a retrospective cohort study and measured obesity by BMI, found that after 5 years of follow-up, a BMI >30kg/m2 was associated with better survival in HD patients (HR 0.89, 95% CI 0.81-0.99, p=.042), although not in PD patients. However, BMI does not distinguish between lean tissue and fat tissue, and as such, the correct interpretation of these results is not clear.
Wu et al.9 analysed the implications of MS in HD in a study that included 91 patients who were followed up for 3 years. They found that patients with MS, as defined by the IDF, had a higher risk of suffering a cardiovascular event and furthermore, they observed that abdominal obesity was the individual MS component that best predicted the risk of suffering a cardiovascular event (hazard ratio [HR] 6.25). In our study, we also found that a CI higher than 1.2 increased the risk of cardiovascular events. Cordeiro et al.13, in a study on HD patients, found that a high CI increased mortality (HR 2.8). Waist circumference, necessary for calculating CI, is a cheap, easy to measure parameter that is associated with morbidity and mortality in HD and one which is hardly being used in HD hospital units.
Our study has some limitations, since it is a single centre study and the sample size was relatively small. It also has strong points, since it determined the prevalence of MS as defined by the ATPIII and by the IDF, which implies that, as well as BMI, the abdominal circumference of all patients was measured and the conicity index was calculated. Likewise, we measured body composition with bioimpedance spectroscopy. All admissions due to a cardiovascular event and mortality were recorded prospectively in the 3 years of follow-up. Furthermore, this is one of the few studies published to date that analyses the prognostic implications of MS in HD patients.
In conclusion, MS is a very prevalent disease in HD patients and is a risk factor for cardiovascular events. Its predisposing factors are: old age, female sex, hyperphosphataemia, a lower dialysis dose and inflammation. An increase in the conicity index and the fat tissue index are risk factors associated with the occurrence of a cardiovascular event. Abdominal circumference should be widely used as a parameter in HD units. MS doubles the risk of cardiovascular events in HD patients, but no association was observed with higher mortality in the 3-year follow-up period. Studies with a larger number of patients and with a longer follow-up period are necessary to analyse the effect of MS on mortality in HD patients.
Conflicts of interest
The authors declare that they have no conflicts of interest related to the contents of this article.
Table 1. Characteristics of patients on haemodialysis with and without metabolic syndrome
Table 2. Predictors of metabolic syndrome (ATPIII): multivariate logistic regression analysis
Table 3. Risk factors associated with the occurrence of the first cardiovascular event: Cox regression analysis
Table 4. Studies of metabolic syndrome prevalence in haemodialysis patients
Figure 1. Influence of the metabolic syndrome in the occurrence of cardiovascular events: Kaplan-Meier analysis
Figure 2. Influence of the fat tissue index in the occurrence of cardiovascular events: Kaplan-Meier analysis
Figure 3. Influence of the conicity index in the occurrence of cardiovascular events: Kaplan-Meier analysis