Introducción: En pacientes en hemodiálisis es frecuente observar pérdida de peso relacionada con el ingreso hospitalario. Nuestro objetivo fue cuantificar esta pérdida de peso y analizar con qué factores se relaciona. Pacientes y métodos: Seleccionamos a pacientes en hemodiálisis crónica, con ingresos hospitalarios por cualquier etiología con duración mínima de 4 días, recogiendo pérdidas de peso al alta, a las 2 y 4 semanas del alta, así como evolución de variables con interés nutricional (creatinina, albúmina, transferrina, nPNA) tras su alta. Resultados: Incluimos a 77 pacientes, con 67 ± 12 años y 30 ± 34 meses en hemodiálisis, 40 mujeres (51,9%) y 22 diabéticos (28,6%). La estancia hospitalaria fue 17,8 ± 12,6 días (mediana 12 días). El 70,4% mostraron pérdida de peso al alta y un 81,3% a las 4 semanas del alta, sin influir sexo ni diabetes. El peso disminuyó al alta -1,09 kg (IC 95%, -0,73 a -1,44), —1,64 kg (IC 95%, -1,21 a -2,07 kg) a las 2 semanas y -1,94 kg (IC 95%, -1,47 a -2,42 kg) a las 4 semanas. Tras el alta observamos un descenso de urea (antes del alta 134 ± 40 frente a después del alta 119 ± 36 mg/dl; p = 0,001), creatinina (antes del alta 8,1 ± 2,6 frente a después del alta 7,5 ± 2,6 mg/dl; p <0,001), fósforo (antes del alta 5,2 ± 1,7 frente a después del alta 4,3 ± 1,5 mg/dl; p <0,001), albúmina (antes del alta 3,70 ± 0,48 frente a después del alta 3,56 ± 0,58 g/dl; p = 0,05). La pérdida de peso a las 4 semanas se correlacionó con una mayor estancia hospitalaria (r = 0,41; p <0,001), mayor índice de masa corporal en el momento del ingreso (r = —0,23; p = 0,05) y menor albúmina en el ingreso (r = 0,39; p = 0,012) y con albúmina (r = 0,27; p = 0,05), creatinina (r = 0,30; p = 0,02) y nPNA (r = 0,47; p = 0,002) más bajos después del ingreso. Albúminas más bajas en el momento del ingreso se correlacionaron con mayores descensos de la creatinina después del ingreso (r = 0,42; p = 0,009) y con una estancia más prolongada (r = —0,61; p <0,001). Con análisis multivariante, la pérdida de peso se asoció con mayor duración de estancia y con potasio sérico antes del ingreso. Conclusiones: La hospitalización de pacientes en hemodiálisis provoca una pérdida significativa del peso corporal debido a una probable pérdida de la masa muscular. La mayor estancia hospitalaria y el estado inflamatorio durante el ingreso son los factores que se relacionan con el deterioro nutricional que sufren los pacientes en hemodiálisis durante su hospitalización.
Background: It is frequent to observe that hemodialysis patients suffer important loss of weight during hospital stay. This issue has not been investigated previously. Our aim in this study was to analyze factors associated with this loss of weight and what changes occur after admission in biochemichal parameters with nutritional interest. Patients and methods: We retrospectively selected patients undergoing chronic hemodialysis who were admitted at hospital for acute or chronic pathologies, with a minimum length of stay of 4 days, taking only one episode of admission per patient. We chose loss of weight observed at hospital discharge, at 2 and 4 weeks later and we also collected routine laboratory data and adecuacy parameters before and after the hospital admission and basic biochemical parameters in the first week of hospital stay. Results: We included 77 patients, with 67±12 years and 30±34 months in dialysis. Forty (51,9%) were female (51,9%) and 22 diabetics (28,6%). Length of stay was 17,8±12,6 days (median 12). There were 70,4% patients who suffered a loss of weight at discharge and 81,4% at 4 weeks, without differences in sex or diabetes. Weight decreased significantly with a mean of -1,09 kg (95%CI -0,73 to -1,44). After 2 weeks the loss of weight was -1,64 kg (95%CI -1,21 a -2,07 kg) and after 4 weeks was -1,94 kg (95%CI -1,47 a -2,42 kg). Comparing parameters before and after admission, we observed a significantly decrease in serum urea levels (before 134±40 vs after 119±36 mg/dl; p= 0,001), creatinine (before 8,1±2,6 vs after 7,5±2,6 mg/dl; p<0,001), phosphate (before 5,2±1,7 vs after 4,3±1,5 mg/dl; p< 0,001) and albumin (before 3,70±0,48 vs after 3,56±0,58 g/dl; p=0,05), without changes in adequacy parameters. Greater loss of weight at 4 weeks from discharge was correlated with larger length of stay (r= 0,41; p<0,001), greater body mass index at admission (r= -0,23; p=0,05) and lower serum albumin at admission (r= 0,39; p= 0,012). It was also correlated with a lower serum albumin (r= 0,27; p=0,05), lower creatinine (r= 0,30; p= 0,02) and lower protein intake (nPNA) (r= 0,47; p= 0,002) after discharge. Lower serum albumin levels at admission were correlated with greater decreases of creatinine after discharge (r= 0,42; p= 0,009) and larger length of stay (r= -0,61; p<0,001). Employing multivariate analysis we found that loss of weight was associated to length of stay and serum potasium levels before admission. Conclusions: Hospitalization of hemodialysis patients have a negative nutritional impact causing a significant loss of weight, probably reflecting a reduction of muscle mass. We found that length of stay in hospital is a basic factor associated with this nutritional impairment. The pathologies promoting hospitalization could influence this derangement through inflammation but this hypothesis should be investigated.
INTRODUCTION
The prevalence of malnutrition in patients at the moment of hospital admission is high, oscillating between 25 and 45%, and varies with age, the pathology presented and the criteria used to measure this variable.1-4 By using a global subjective evaluation system of patients about to undergo gastrointestinal surgery, Detsky5 observed moderate malnutrition in 21% of patients, and severe malnutrition in 10%. Using bioelectrical impedance analysis (BIA) Kyle6 observed a 25% reduction in fat-free mass in patients admitted with acute pathologies and normal body mass index (BMI), which reached 37% when dealing with chronic diseases. Weight loss before hospital admission also occurs in 16% of patients, and a reduced phase angle in the BIA in up to 74% of cases.3
Hospital malnutrition is important due to the risk factors linked to the higher rate of nosocomial infections (wounds, pneumonias, urinary infections), decubitus lesions, deficient wound cicatrisation, and suture dehiscence,3,4 which tend to cause increased mortality rates,3,5,7 longer hospital stays,1,7 and greater economic costs and use of resources.2,7,8 The hospital environment often leads to greater nutritional deterioration due to a combination of factors, leading to the development of a variety of strategies designed to provide early nutritional support in order to reduce morbidity/mortality and hospital costs.7,8
The hospitalisation rate in haemodialysis patients is greater than in other patients9 and is greater in patients with higher comorbidities,10 worse vascular access,11 older age,9,10 worse quality of life12 and reduced apetite.13 It is very common to observe a progressive and fast reduction in dry weight of patients on haemodialysis, in even just a few weeks, with relation to the number of hospital admissions. This well known phenomenon has not been specifically studied in the medical literature. The only study that we have come across, Ikizler,14 reviewed hospitalised haemodialysis patients and observed a mean reduction of 2.5 kg upon discharge, along with a reduction in protein-calorie intake and a negative nitrogen balance, leading to the conclusion that a clear nutritional deterioration existed in these patients.
In order to further explore the significance of this phenomenon, we proposed this retrospective study to analyse what factors are related to weight loss in haemodialysis patients following hospitalisation, and what other nutritional variables of interest could be affected.
PATIENTS AND METHODS
The Jaén Hospital Complex is a reference hospital for a population of 650,000 inhabitants. The nephrology department attended to 290 haemodialysis patients between January 2004 and December 2006, distributed in 3 centres: a hospital unit, a satellite centre in the capital of Jaén, and a dialysis centre in Úbeda (NefroUbeda). When these patients require more than 2 days of hospitalisation, they are always treated at the Jaén Hospital Complex, independently of the dialysis unit which the patients normally attends, since our centre is the only one in the province that provides a hospital dialysis programme.
From amongst the patients with over 3 months on chronic haemodialysis that were hospitalised during the study period, we selected those episodes with over 4 consecutive days of hospitalisation, considering shorter durations to be insufficient to produce significant changes. We registered 370 episodes of hospitalisation for over 4 days in 225 patients on haemodialysis, with a range of 1 to 11 admissions per patient. The mean age of this patient population was 67 ± 14 years, and the mean duration of hospital stay was 13.8 ± 9.3 days (range: 5-74).
We included planned and emergency episodes of hospitalisation attended by our unit or by others, due to any pathology. We chose one single admission for each patient in order to avoid excessively weighting re-admitted patients and the inherent self-correlation that this would entail. When a patient had more than one admission during the study period, we chose the first admission recorded. We excluded those patients that died during their hospital stay, since we could not analyse their progress after discharge from the centre, and also patients who were treated for more than 4 days in the intensive care unit, since weight changes in these patients could be excessive and skew the results from normal patients. From the total number of available patients, we obtained a randomised sample using an alphabetically ordered list of names and choosing the first of each three patients. The sample obtained included 34.2% of the patients hospitalised during the study period.
We collected demographic data, routine lab results, and dialysis parameters such as protein intake (nPNA) and dialysis dosage (Kt/V second generation Daugirdas corrected for rebound) of each patient before and after admission. Samples from lab analysis were taken within 1 – 6 weeks before the hospital admission, and 1– 2 months after discharge. We also collected haemoglobin/haematocrit, urea, creatinine, potassium, phosphorous, albumin, transferrin, and ferritin tests performed during the first week of hospital stay in patients that could provide this data, for later analysis of possible correlations between these variables and weight loss.
We followed the patient’s weight throughout the haemodialysis period, measuring weight one week before admission, upon admission, upon discharge, and at 2 and 4 weeks following discharge from the hospital. We calculated changes in weight (¢W) upon discharge (¢WDischarge), at 2 weeks (¢W+2w) and at 4 weeks (¢W+4w) after discharge, as the difference between the patient’s weight at each period and the weight measured when the patient was admitted. A negative value indicates weight loss, and a positive value indicates weight gain. We counted the total number of haemodialysis sessions and the accumulated weight loss produced therein during the hospital stay.
Results are expressed as a mean ± standard deviation. Changes in weight are expressed as the confidence interval for the mean in parenthesis. The variables with highly skewed distributions such as hospital stay and ferritin were log-transformed for the statistical analyses. We used Student’s t and Wilcoxon tests for comparison of paired quantitative variables according to the sample size and distribution. For the comparison of non-paired quantitative variables, we used the Student’s t test when the data presented a normal distribution, and the Mann-Whitney test when they were not normal, or the sample size was small (n< 30). We used a correlation analysis for the relationship between numerical variables, using the Pearson correlation coefficient for data with a normal distribution, and the Spearman coefficient for non-normal data. We used a multiple linear regression for the multivariate analysis, testing for multivariate normality using a residual analysis. We considered values to be significant when P< 0.05.
RESULTS
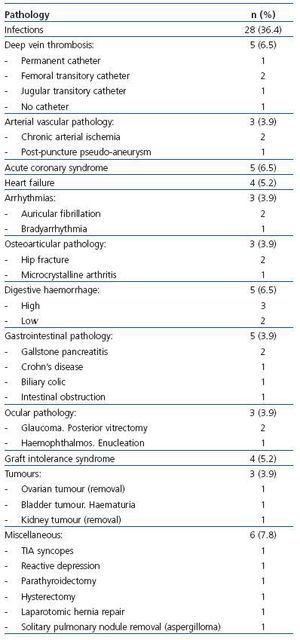
67 ± 31 years (range: 26-84), with 31 ± 34 months on dialysis (range: 3-184), and 22 (28.6%) were diabetic. The mean duration of hospital stay was 17.8 ± 12.6 days (range: 5-55 days), with a median of 12 days (first quartile = 9 and third quartile = 21 days). The diseases that caused hospitalisation are summarised in Table 1 and Table 2. The main medical and surgical pathologies requiring haemodialysis were represented, infections being the most common reason, especially those related to vascular access.
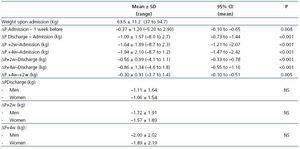
Weight changes after dialysis in the different periods measured are summarised in Table 3. Patient weight after dialysis was reduced upon discharge and continued to descend to an average of almost 2kg after 4 weeks. Weight loss was already noticeable one week before admission. 71.2% of patients experienced weight loss upon discharge, 67.2% at 2 weeks, and 81.3% at 4 weeks. The sex of the patient had no influence on weight lost.
By comparing the lab results from before and after hospital admission we observed a significant reduction in levels of urea, creatinine, phosphorous, and haemoglobin (Table 4), with non-significant increases in ferritin (logarithm) and no changes in nPNA and Kt/V. Serum creatinine values fell in male patients (8.7 ± 3.1mg/dl before hospital admission as compared to 8.0 ± 3.0mg/dl after hospital admission; P= 0.006) and this reduction was less severe for women (7.6 ± 2.0mg/dl before admission,
7.1 ±2.0mg/dl after admission; P= 0.07). In the rest of the lab results, only males had severely reduced potassium levels (5.1 ± 1.0mEq/l before admission, 4.6 ± 1.0mEq/l after admission; P= 0.007).
Lab results compared between pre-hospitalisation samples and those taken during the first week of hospitalisation showed significant decreases in creatinine (8.2 ± 2.8 versus 7.4 ± 3.0mg/dl; P= 0.008), albumin (3.70 ± 0.46 versus 3.08 ± 0.67g/dl; n = 36; P< 0.001), transferrin (195 ± 48 versus 166 ± 46mg/dl; n = 36; P< 0.001), potassium (5.0 ± 1.0 versus 4.6 ± 1.0mEq/l; P= 0.001) and haemoglobin (11.2 ± 1.7 versus 10.1 ± 1.7g/dl; P< 0.001) and a significant increase in ferritin (401 ± 331 versus 700 ± 608ng/ml; n = 36; P= 0.001).
Weight loss was greater with longer hospital stays (Table 5). Lab results from before hospitalisation were not different amongst the different hospitalisation terciles. Analysis of the results from after hospitalisation showed significantly lower albumin levels in longer hospital stays. Results from the first week of hospitalisation also showed significantly lower albumin levels in patients with longer hospital stays, as well as lower levels of transferrin and haemoglobin, and higher levels of ferritin, although these differences were not significant.
¢WDischarge was correlated with ¢W+2w (r= 0.85; P< 0.001) and with ¢W+4w (r= 0.77; 0 <0.001). ¢W+2w was also correlated with ¢W+4w (r= 0.90; P< 0.001). ¢WDischarge was not correlated with age or time on dialysis. We observed no correlations between weight changes and total ultrafiltrate volume processed in haemodialysis sessions during hospital stay, even after correcting for the number of dialysis treatments and number of days of hospitalisation. A longer hospital stay was correlated with greater weight losses in ¢WDischarge, ¢W+2w, and ¢W+4w (Table 6).
Weight changes were not correlated with pre-admission lab results. Lower serum urea, creatinine, and potassium levels before the hospitalisation were correlated with greater weight loss (Table 6). Lower albumin levels before hospitalisation were correlated with higher ¢W+4w (r= 0.39; P= 0.012).
Serum creatinine levels decreased more in patients with longer hospital stays, lower albumin levels during hospital stay, and lower potassium, albumin, and creatinine levels, and higher ferritin levels following hospitalisation (Table 6). Albumin levels fell more in patients with longer hospital stays, higher initial weight and BMI, and with lower serum albumin levels during hospital stay. Furthermore, we also observed a correlation with greater reductions in serum creatinine levels and lower potassium levels following hospitalisation (Table 6).
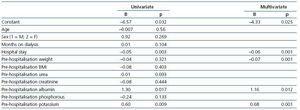
We performed a multivariate analysis in order to determine which variables were related to weight loss following hospitalisation. We introduced sex, age, time on dialysis, hospital stay, weight and BMI from when the patient was admitted, and lab results before hospitalisation (urea, creatinine, albumin, potassium, and phosphorous) as explanatory variables for ¢W. This multiple linear regression analysis produced duration of hospital stay and pre-admission potassium levels for determining ¢WDischarge (r= 0.43; P< 0.001; F= 16.7). ¢W+2w was related to duration of hospital stay and pre-admission potassium levels (r= 0.49; P< 0.001; F= 11.9). ¢W+4w was related to duration of hospital stay, weight upon admission, and albumin and potassium levels before hospitalisation (r= 0.63; corrected r2= 0.36; P< 0.001; F= 11.8) with coefficients expressed in Table 7.
DISCUSSION
Dry weight loss is commonly induced in haemodialysis patients when they suffer prolonged periods of anorexia with poor interdialysis weight gains, or after having been admitted to the hospital. However, this phenomenon of progressive, nonvoluntary weight loss is a consequence of nutritional deterioration, and has not been the subject of much medical research. We have attempted to quantify this weight loss and to analyse which factors could be influencing it. The primary result of our study has been the observation of weight loss after dialysis in the majority of patients upon discharge from the hospital, which is accentuated at 2 and 4 weeks after discharge, these weight losses after discharge all being strongly correlated to losses upon discharge. Furthermore, we have also observed a reduction in weight after dialysis upon hospital admission as compared with patient’s weight one week prior to admission, although this was seen in fewer patients. The only study that we have found that deals with this topic, Ikizler,14 analysed 18 patients on haemodialysis during their hospital stay and observed a reduction in average weight of 2.5kg by the time they were discharged, with a negative nitrogen balance and hypoalbuminaemia following hospitalisation. In a very recent study, Chan15 analysed the importance of post-hospitalisation changes in their capacity to induce re-hospitalisation, and also observed a very clear reduction in dry weight following hospitalisation.
It is difficult to discern the origins of this post-dialysis weight loss and dry weight loss observed in our study and daily clinical practice, since we have not used any methods to measure body composition. However, we have found some relationships that may serve to explain the observed changes. Weight loss was correlated with a reduction in serum albumin values during the first days of hospital stay. We also observed a reduction in serum transferrin values and an increase in serum ferritin values during hospitalisation and after discharge from the hospital, which together may reflect an inflammatory response triggered by the various diseases presented by the patients. The reduction in serum creatinine levels after hospital admission and the correlation found between greater decreases in creatinine values and the presence of hypoalbuminaemia during hospitalisation suggest that the inflammatory response could also be the cause for this reduction. Given that creatinine is localised in muscle tissue, the loss in body weight would logically be due to a loss in muscle mass and, therefore, body protein content would be significantly affected, implicating a nutritional deterioration in the haemodialysis patient.
Both the causal condition for hospitalisation and those that arise as complications during hospital stay trigger a systemic inflammatory response, which can lead to nutritional deterioration. Clear examples are found in prolonged stays in intensive care units, burn units, or following surgeries with prolonged postoperative periods, in which severe persistent hypoproteinemia, reduced muscle mass and body weight, and reduced functional capacity of the patient arise.16,17 High proinflammatory cytokine levels (IL-1 and IL-6) are the initial mediators in this response, which provokes changes in the liver in the synthesised protein profile, with high levels of CRP, ceruloplasmin, and alpha-1-acid glycoprotein, among others, and a decrease in prealbumin and albumin. These also stimulate a generalised protein catabolic response, especially strong in the skeletal muscle tissue, in which the activation of the ubiquitin-proteasome system contributes to the degradation of myofibrils and the release of amino-acids.18 This is accompanied by a marked systemic hormonal change with elevated catecholamines, ACTH, cortisol, glucagon, etc., which translates into an insulin resistance, with increased lipolysis and decreased glucose consumption in the muscle tissue, diverting the glucose to the liver, viscera and brain, and a reduction in protein synthesis. Protein synthesis is also halted due to the key effect of the glucocorticoids that also facilitate the transport of amino acids to the liver and promote gluconeogenesis.
Fasting initially activates muscle catabolism with a freeing of amino acids in order to support gluconeogenesis. After 3-4 days, basal metabolic rate is reduced along with protein synthesis and catabolism, while simultaneously, the low insulin levels favour lipolysis by adipocytes in order to free fatty acids as a combustible alternative to glucose. This coordinated response facilitates a neutral nitrogen balance and minimises the negative effects on protein levels. If inflammation exists, proinflammatory cytokines provoke an increased metabolism in the organism along with activation of protein (muscle) catabolism, which produces a negative nitrogen balance with the consequent loss in muscle mass.19-21 Fatty tissue is also involved in this stress response, releasing fatty acids thanks to the catecholamines in order to provide an extra source of energy in this highly metabolically demanding situation, which would also explain the decrease in body fat.17 Administration of glucose solutions without nitrogen in this situation leads to an increase in insulin levels, which will reduce adipocyte lipolysis, halting this release of alternative energy sources, remaining gluconeogenesis from muscle amino-acids as the only available mode of fuel (glucose) synthesis for general use. All of these adaptive metabolic pathways explain the reason for which muscle tissue is the most severely affected during hospital stays.22-24
In addition to this increased metabolic demand, nutritional uptake is clearly reduced in the hospital environment. General caloric intake is two-thirds lower than recommended in 64-70% of patients, and protein intake is two-thirds lower than recommended in 43-54% of admitted patients.25 Close to a third of hospitalised patients consume less than their estimated daily minimum energy and protein requirements, and in acute patients, this deficit rises to 44.7 and 47.5%, respectively.26 Prolonged fasting, whether motivated by the patient or diagnostic tests, clearly reduces daily food intake, but there are also other factors to be considered that are just as important. 59% of hospitalised patients refuse to eat hospital food26 due to several causes: excessively restrictive or specialised diets; they do not like the dishes offered at the hospital, lack of choice; foods arriving cold at the patient’s room; eating hours that are excessively early for the schedules that the patients are used to, etc. On the other hand, the patient may refuse hospital food, but does consume snacks and other foods brought by family members, which provide up to a third of the patient’s protein calorie requirements, especially in older patients.26 These factors are often as important as anorexia or poor digestive tolerance that is associated with the diseases that provoke hospitalisation and require a local analysis in order to find solutions that minimise this problem.
Haemodialysis patients also consume less food during hospitalisation, with protein intake reduced to 66% of the recommended quantity, and caloric intake to 50%.14 Only 33.3% of patients consume the recommended quantity of dietary protein and none consume an adequate number of calories.27 The reason for this reduced uptake in haemodialysis patients has been linked to inflammatory stimulus and the presence of gastrointestinal symptoms related to infradialysis,14,28 although food preference factors due also exist.27 In our study, we did not evaluate food intake, but we did produce some data that point towards some level of anorexia or reduced food consumption that could have influenced the severity of weight loss. Serum urea and phosphorous values were lower following hospital admission, which could be attributed to an increase in dialysis dosage, although this does not appear to be the cause since we observed no accompanying increase in Kt/V. Meanwhile, less severe weight loss was correlated with lower nPNA values after hospitalisation, which could indicate that patients with a higher level of anorexia following hospital stay suffer more extreme weight loss. It was also correlated with lower serum potassium levels before hospitalisation, which points toward the existence of anorexia at the time of admission in some patients. It is in accordance with the observation that a reduced appetite before hospitalisation is a predictor for duration of hospital stay.29 Together, it is possible that poor appetite and reduced food consumption present themselves upon hospital admission, during the hospital stay, and are even maintained after discharge, and are related to the inflammatory stimulus and anorexigenous effect of some cytokines, which all contribute to the global weight loss.
In order to reduce the negative impact of hospital stays on the level of food consumption in haemodialysis patients, some measures should be taken into account, such as minimising changes in dialysis schedules, assign appointments that do not interfere with normal eating hours, expand the dialysis diet to be less strict during hospitalisation, and adapt dialysis sessions to the situation of the patient, in order to avoid infradialysis and poor haemodynamic tolerance that might reduce consumption directly or produce vomiting that interferes with eating.
Our data show that with a longer hospital stay in haemodialysis patients, more weight is lost, more severe decreases are produced in creatinine and albumin levels, and in albumin values following admission, with no influence of age and time spent on dialysis, findings that concur with those found in a recent study.15 Transferrin, potassium, and nPNA values were also lower after hospitalisation, and ferritin values were higher in patients with longer stays, although some of these changes were not significant due to the widely dispersed data. These relationships between hospital stay and nutritional variables must be linked by the severity and/or number of pathologies presented upon hospitalisation, which would be mediated by the inflammatory stimulus that triggers: the more severe, the longer hospitalisation and greater inflammation (lower albuminemia) with strong changes in nutritional variables. The acute nutritional deterioration that is produced during hospital stay is responsible for the reduced functional capacity observed in over 70% of patients of advanced age on haemodialysis following hospitalisation.30 In this sense, hypoalbuminemia, as a reflection of the patient’s diseases, is logically related to a longer hospital stay in our study, but it is also logical that it be a predictive factor for hospital mortality, greater incidence of re-admissions, and a greater incidence of nosocomial infections.31-34 In some studies in which direct inflammation markers are used, such as alpha-1-acid glycoprotein, these appear to be better prognostic markers than even albumin,35 which indicates that the inflammation and not albumin, which is responsible for the poor prognosis in some hospitalised patients.
Maintaining an adequate dry weight in hospitalised patients is a difficult task due to the fact that haemodynamic stability and the situation of the patient often do not allow for large ultrafiltrations, the duration of dialysis is shortened, shift changes are frequent, and the treatment can be inadequate due to vascular access difficulties. Moreover, the patients cannot be weighed sitting, and bed scales are not always available. The increase in muscular catabolism comes with a reduction in intracellular volume and an increase in extracellular water,22 which cannot be eliminated in patients with acute renal failure or on dialysis, contributing to distort the dry weight measurement by developing peripheral oedema in some cases and heart failure in others due to overloading during hospitalisation. All of these factors explain why patients do not leave the hospital with an adequate weight when they are discharged, a change that is not manifested until they return to their dialysis unit5 and have improved sufficiently to withstand stronger rates of ultrafiltration. This also explains why in our study we observed greater reductions in body mass after the patient was discharged from the hospital, and we must also mention that the adjustment for dry weight was made using different methods than those employed while the patients were hospitalised, and so the weight loss was not intentional, but was rather a “natural” phenomenon, neither provoked nor predicted. We must also point out that perhaps not all of the weight lost was produced during hospital stay, as it could also have been developed from the patients’ diseases before hospitalisation without having manifested itself until the patients were in the dialysis unit, once the disease was under control and the patient’s dry weight was adjusted. This is supported by the results from the multivariate analysis: albumin before hospitalisation was a predictor for the amount of weight loss observed at the end of the 4 weeks after discharge from the hospital.
This study could have one important limitation, which is the bias produced by limiting the analysis to those patients that did not die during their hospital stay or were admitted to the intensive care unit. It is possible that in this group of patients the weight loss could have been even more severe. However, our objective was to establish an estimation of what occurs in hospitalised patients that return to their dialysis unit after hospitalisation. The number of patients used for this study has permitted us to estimate these changes with a sufficient level of precision. If we had used some technique to evaluate body composition, we could confirm some of the hypotheses established so far, although the application of these methodologies in patients that are constantly changing, such as hospitalised patients, can become problematic for interpretation.
In summary, we have observed that hospitalised patients on haemodialysis suffer a progressive reduction in body weight that is evidenced several weeks after discharge from the hospital, and that is very probably related to nutritional deterioration. This implies that patient dry weight should be monitored during and after hospitalisation in order to avoid overloading and congestive heart failure. It is also important to approach these patients from a nutritional perspective, monitoring their intake during and after hospital stay, performing a nutritional evaluation upon admission, and providing nutritional support for several weeks if an adequate appetite and intake are not observed. We believe that the cause of this nutritional deterioration in haemodialysis patients is related to the inflammatory stimulus that is triggered by the disease or sum of diseases suffered by the patient during hospital stay, as well as the poor dietary intake that this produces, which justifies an early resolution of these conditions in order to avoid severe nutritional deterioration that could lead to greater morbidity and possible consequent hospitalisations.
Table 1. Causes of hospitalisation in the population on haemodialysis included in the study
Table 2. Infectious causes for hospitalisation
Table 3. Body weight one week before hospitalisation (-1 week), upon hospital admission, and the variations in weight observed upon discharge and at 2 and 4 weeks after discharge with respect to weight measured upon admission to the hospital and discharge from the
Table 4. Evolution of lab results and haemodialysis parameters before and after hospitalisation
Table 5. in weight at discharge from hospital, 2 weeks and 4 weeks post-discharge; lab results from hospital admission and first week of hospitalisation according to hospital stay terciles
Table 6. Correlations between change in weight at discharge, at 2 weeks, at 4 weeks, change in creatinine (DCr) after admission vs before admission, change in serum albumin (&
Table 7. Factors associated with weight loss after 4 weeks following discharge from the hospital in haemodialysis patients (univariate multiple linear regression analysis after a stepwise selection of variables)