Introducción y objetivos: La frecuencia e importante repercusión clínica de la enfermedad renal crónica (ERC) en los pacientes con diabetes mellitus tipo 2 (DM2), junto con la posibilidad de mejorar su evolución mediante una intervención precoz, refuerza la necesidad de una estrecha colaboración en su detección y tratamiento entre nefrología y atención primaria. Objetivos: Los objetivos del estudio son estimar la prevalencia de ERC en los pacientes con DM2 controlados en atención primaria en nuestro sector sanitario y determinar el volumen de pacientes que serían remitidos a las consultas de nefrología. Material y métodos: Se incluyeron pacientes mayores de 18 años de edad, en los que se había realizado analítica por cualquier motivo en los 16 centros de salud del sector sanitario de Alcañiz (84.340 habitantes) a lo largo de 2008. Se recogieron datos demográficos (edad y sexo), creatinina plasmática, cociente albúmina/creatinina en orina simple, hemoglobina glicosilada, potasio y hemoglobina. Se calculó el filtrado glomerular estimado (eFG) por la fórmula MDRD. Se revisaron los criterios de remisión a nefrología de acuerdo con el Documento de Consenso sobre ERC de la Sociedad Española de Nefrología-Sociedad Española de Medicina Familiar y Comunitaria (S.E.N.-SEMFyC) de 2008. Resultados: Del total de 16.814 pacientes incluidos, 3.466 (20,6%) presentaron DM2. En los pacientes con DM2 la prevalencia de ERC según criterios K/DOQI fue del 34,6% (IC 95%, 33-36,2). El eFG <60 ml/min/m2 se registró en el 25,2% de los pacientes con DM2, siendo en este subgrupo la prevalencia de micro-macroalbuminuria del 31,7%. Cumplieron criterios de remisión a consultas de nefrología 104 pacientes con DM2 (3%) y 132 sin DM2 (1%) (p <0,0001). Conclusiones: La prevalencia de DM2 en los centros de salud es elevada, con frecuente presencia de ERC y micro-macroalbuminuria asociada. Un porcentaje significativo de pacientes cumple los criterios de remisión consensuados S.E.N.-SEMFyC. La colaboración con atención primaria es fundamental en la detección precoz y seguimiento de esta enfermedad, de tal forma que en cada área de salud debe protocolizarse el seguimiento conjunto, con unos objetivos que deben cumplirse en función del estadio de ERC.
Introduction: The frequency and clinical impact of chronic kidney disease (CKD) in type 2 diabetes patients (DM2) and the benefits of early intervention highlights the need for close collaboration in detection and management between Nephrology and Primary Health Care. Objective: Our objectives were to estimate the prevalence of CKD in DM2 patients controlled by primary care and evaluate the need to early referral of CKD DM2 patients to renal specialists Material and methods: Study population: patients older than 18 years of age, with analysis made for any reason in the 16 Health Centers of Health Sector Alcañiz (84,340 inhabitants) during 2008. Variables: age, sex, serum creatinine, urine albumin/creatinine ratio, glycated hemoglobin, potassium and hemoglobin. We calculated the estimated glomerular filtration rate (eGF) by the MDRD formula. We reviewed the Consensus Document S.E.N.-SEMFyC ERC 2008 criteria for referral to renal specialists. Results: Of the 16,814 patients enrolled, 3,466 (20.6%) had DM2. In DM 2 patients, the prevalence of CKD was 34.6% (IC 95%, 33-36.2). eGF <60 ml/min/m2 was recorded in 25.2% of DM2 patients. In this subgroup the prevalence of albuminuria was 31.7%. Met criteria for referral to renal specialists 104 (3%) DM2 patients and 132 (1%) non diabetic patients (p <0.0001). Conclusions: The prevalence of DM2 in the Health Centers is high, with frequent presence of CKD and albuminuria. An important percentage of patients meets the referral S.E.N.-SEMFyC criteria. The collaboration with primary care is essential in early detection and monitoring of these patients, and common primary care and nephrology protocols are need.
INTRODUCTION AND OBJECTIVES
Chronic kidney disease (CKD) is one of the most common and damaging complications of type 2 diabetes mellitus (T2DM). Often patients with T2DM have CKD and this process, in addition to notably increasing cardiovascular morbidity and mortality, is the leading cause of kidney replacement treatment in most countries.1,2 We currently have therapeutic options to improve its evolution, especially if detected in the early stages.3-5 These data reinforce the need for early detection and proper treatment of this disease, which makes the close collaboration between nephrology and primary care essential.6
Current epidemiological data give us a better idea of the scale of the CKD problem. The EPIRCE study detects a prevalence of CKD in the general population of 9.06% in Spain,7 and two studies addressing the impact of this disease in primary care indicate a prevalence of 21.3% in the EROCAP8 study and 16.4% in the Alcañiz health sector9 in patients attended to in health centres. However, no epidemiology studies have been conducted to estimate the prevalence of CKD in patients with T2DM monitored in primary care.
Our aim was to estimate the impact and importance of CKD in patients with T2DM checked at health centres. We have developed this study for that purpose with the following two objectives:
1. Estimate the prevalence of CKD in patients with T2DM monitored in primary care in health centres of the Alcañiz health sector.
2. Analyse the impact of this process on the activity and workload of our outpatient nephrology, determining the number of patients who met criteria for referral proposed in the Consensus Document by the Spanish Society of Nephrology and the Spanish Society of Family and Community Medicine (S.E.N.-SEMFyC).10
MATERIALS AND METHODS
Study design
Transversal descriptive epidemiology study.
Studied population
Patients of both genders, older than 18 years, diagnosed with T2DM, and in whom a biochemical determination had been performed for any reason in any of the 16 health centres of the Alcañiz health sector (serving a total of 84,340 inhabitants) between Janurary 1st and December 31st 2008 were included.
Selection of patients diagnosed with type 2 diabetes mellitus treated in primary care
In the process of improving the quality of CKD treatment previously performed in our health sector with collaboration between nephrology, endrocrinology, biochemistry department and primary care, analytical request profiles were established. One of these is the “DM profile” which specifically determines glycated haemoglobin, glomerular filtration rate and the albumin-to-creatinine ratio in single urine samples. We have considered as diabetic those patients for whom the attending physician first made the request with this profile, independently of the values of glucemia or glycosylated haemoglobin that could be determined in a given analysis. Meanwhile, we believe the absence of analytical results from endocrinology between January 1, 2006 and December 31, 2008 (dates of the computerisation of laboratory services) means that follow-up of patients was done by primary care. We intended to limit the study to DM2 and to relate it in percentages to this group of the adult population. For this reason we limited the study to those older than 18, after consulting with endocrinology that all patients with type 1 DM (DM1) are reviewed in their offices and, therefore, are excluded from the study.
Variables collected
Using a computerised process in the Department of Biochemistry at Alcañiz Hospital, demographic data were collected (gender and age) and analytical assessments (serum creatinine [sCr], glycosylated hemoglobin, potassium, haemoglobin and the albumin/creatinine ratio in urine) were carried out. If there were several analytical determinations in the same patient, the one that had lower creatinine was collected.
Biochemical methods
CRP was determined using a modified kinetic Jaffé method with an autoanalyser Architec C-8000 (Abbot Scientific).
Definitions
The estimated Glomerular Filtration Rate (eGFR) was calculated using the MDRD study equation (Modification of Diet in Kidney Disease): Estimated GFR = 186 x (creatinine) -1.154 x (age) -0.203 x (0.742 if female) x (1.210 if black).11,12 Criteria used were K/DOQI in the definition and staging of CKD. Microalbuminuria was defined as the presence of a simple urinary albumin/creatinine ratio between 30 and 300 mg/g, and macroalbuminuria as a ratio greater than 300 mg/g.
As criteria for referral to nephrology, consultations were adopted as proposed in the SEN-semFYC Document. According to this consensus, patients should be referred to nephrology with DM2 and CKD, considering eGF values (under 70 years: eGFR <45 mL/min/1, 73 m2, over 70 years: EFG <30 mL/min/1, 73 m2) and values of urinary albumin excretion (albumin/creatinine ratio in urine> 300 mg/g).
Statistical analysis
The description of quantitative traits was performed using mean and standard deviation, and the qualitative characteristics by frequency distribution. We calculated the 95% confidence interval (CI) of the estimated rate of patients with DM2 and CKD. The statistical significance of differences between rates was assessed using the chi-squared test. The statistical significance of differences between averages of independent groups was assessed using the Student’s t test. P-values < 0.05 were considered significant.
RESULTS
During the 12 months reviewed, 18,898 CRP determinations were conducted in 17,963 patients in the health centres. 1096 determinations were excluded (5.8%) because they were repeated in the same individual (in this case we consider only those with the lowest CRP value) and 888 (4.7%) for not including age in the analysis request, making us unable to estimate the GFR. Lastly, data on the 16,814 patients were included.
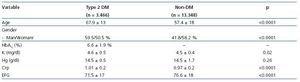
Out of the total number of patients, 3.466 (20.6%) presented with DM2. Age, percentage of men and potassium values were higher in subjects with T2DM, while haemoglobin was similar in patients with and without DM2 (Table 1).
The incidence of CKD and micro-macroalbuminuria was 34.6% (95%, 33-36.2) and 16.1% (IC 95%, 14-18.2%), respectively, in subjects with T2DM, which was significantly higher than the reported incidence in unaffected DM subjects (Table 2). They had an eGFR <60 mL/min/m2 25.2% of DM2 patients, registering the presence of micro-macroalbuminuria in 31.7% of cases.
Glycated hemoglobin did not correlate with eGFR (r = 0.008, p = 0.65) but it did with age (r = -0.495, p<0.001). In cases with micro-macroalbuminuria, mean age was significantly higher (72.5 ± 12 vs 67.5 ± 12 years, p<0.0001) and so was glycated haemoglobin (7.36 ± 1 5 versus 6.8 ± 1.2%, p = 0.001).
One hundred four patients with DM2 (3%) and 132 of those without DM2 (1%) met the criteria for referral to nephrology specialists (p<0.0001). Of the patients with T2DM who met criteria for referral, 78.9% had micro-macroalbuminuria.
DISCUSSION
Patients diagnosed with T2DM managed in primary care represent a significant percentage of routine work of health centres. The frequency of CKD in this group is very high at 34.6%, which means that one out of three patients will have even greater cardiovascular and renal risks. Furthermore, the high prevalence of micro-macroalbuminuria at 16.1%. adds another factor that we know effects the morbidity and the development of terminal CKD.
In terms of the aetiology of CKD in DM2, as well as diabetic nephropathy, hypertensive nephroangiosclerosis and renal vascular disease are common causes. Therefore, up to 50% of patients with DM2 and a significant decrease in eGFR did not have micro-macroalbuminuria, in contrast to CKD from classical diabetic neuropathy.13 Although the risk of terminal CKD does not appear to differ significantly if renal involvement is related to diabetic nephropathy or other diagnostic groups,14 it seems appropriate to perform a screening for albuminuria as well as an assessment of renal function in the identification of CKD in DM2. Indirectly, the fact that the eGFR is not correlated with glycated haemoglobin and it is with age, while the presence of micro-macroalbuminuria is related to older age and higher levels of glycated hemoglobin, suggests that the decline of eGFR may depend on other diseases, while the micro-macroalbuminuria would relate more with diabetic nephropathy.
It is important to consider that people with DM2 and CKD have a high cardiovascular and renal risk, and that actions to reduce this risk are priorities.15,16 Its evolution significantly improves if the disease is detected at an early stage and an appropriate treatment program is implemented. For this reason, in the document agreed upon by the S.E.N.-SEMFyC, special attention is paid to these patients, setting some reasonable objectives for detection, treatment and control. Cardiovascular risk as well as the evolution to terminal CKD in patients with T2DM can be reduced by adequate glycemic control (target glycosylated hemoglobin less than 7%), a reduction of blood pressure values (to 130/80 mmHg), good control of dyslipidemia (target LDL cholesterol below 100 mg/dL) and the introduction of drugs capable of blocking the renin-angiotensin system, and also avoiding nephrotoxic drugs and monitoring even relatively trivial processes that may lead to renal function impairment.
These actions constitute a remarkable effort in a large population, which in our health sector would cover at least 1199 patients. If we apply the referral criteria in the SEN-semFYC document, 3% of them should be referred to nephrology specialists, three times higher than non-diabetics subjects. Previous estimates and the growth experienced in our consultations after the release of a protocol for treatment of common CKD in primary care (about 37%)9,17 highlight the limited resources available for attention to this process, enhancing the need for collaboration between nephrology and primary care to share in the care of patients with CKD.
There are, in our study and in general in epidemiological studies on the CKD,7,8,18 some limitations. These studies are carried out with a single time point, so transient alteration of renal function cannot be distinguished from established CKD. Also, we do not have a gold standard for estimating GFR, although the MDRD formula does seem appropriate in population studies.1,2 As an advantage the large sample size should be noted, which allowed higher accuracy in estimating the prevalence of CKD in patients with DM2.
We conclude that the frequent presence of CKD (34.6%) and micro-macroalbuminuria (16.1%) in patients with T2DM followed in primary care is an important factor in cardiovascular and renal risk that must be detected early and treated properly. A significant percentage of patients met the criteria agreed by SEN-semFYC for referral of diabetic patients (3%). Collaboration with primary care is essential in the early detection, control and monitoring of these high-risk patients.
Table 1. Demographic and analytic data of patients with type 2 diabetes mellitus and non-diabetics
Table 2. Stages of chronic kidney disease and presence of micro/macro albuminuria in patients with type 2 diabetes mellitus and non-diabetic patients