Antecedentes: El aumento del tamaño renal desempeña un papel importante en el desarrollo de la hipertensión arterial (HTA) en pacientes con poliquistosis renal autosómica dominante (PQRAD) con función renal normal. Material y métodos: Se han practicado a 37 pacientes con PQRAD, filtrado glomerular estimado (FGe) por MDRD >60 ml/min/1,73 m² y supuestamente normotensos, una monitorización de la presión arterial (MAPA) y una ecografía renovesical para investigar la posible relación entre el aumento del tamaño renal y un perfil patológico de presión arterial (PA) en estadios de prehipertensión. Resultados: 13 pacientes resultaron ser normotensos, 11 presentaron HTA enmascarada, 4 tuvieron HTA de bata blanca y 9, HTA verdadera. Se ha observado en los pacientes normotensos con patrón reductor de la PA una correlación positiva y estadísticamente significativa entre el tamaño renal y la variabilidad de la presión arterial diastólica (PAD). Conclusiones: La MAPA permite realizar un diagnóstico precoz de la HTA e identificar a pacientes con hipertensión enmascarada. Este trabajo sugiere que en pacientes normotensos con PQRAD existe una posible relación entre el tamaño renal y un perfil de PA con mayor riesgo cardiovascular.
Background: Enlargement of renal size plays an important role in the development of hypertension in patients with autosomic dominant polycystic kidney disease (ADPKD) and normal renal function. Methods: A 24h blood pressure monitoring (ABPM) and a renal ecography have been performed in 37 patients with ADPKD and estimated glomerular filtration rate >60 ml/min/1,73m2 to study the relationship between renal size and an altered blood pressure profile in prehypertension stages. Results: 13 patients had normal blood pressure, 11 were diagnosed of masked hypertension, 4 had white coat hypertension and 9 had hypertension. We have found in the normotensive group with a dipper blood pressure profile a positive and statistically significant relationship between renal size and diastolic blood pressure variability. Conclusions: ABPM helps to make an early diagnosis of hypertension and to identify those patients with masked hypertension. This study suggests a relationship between renal size and a blood pressure profile linked to a major cardiovasular risk in normotensive patients with ADPKD.
INTRODUCTION
Autosomal dominant polycystic kidney disease (ADPKD) is a genetic disease characterised by the presence of bilateral renal cysts that progressively increase in number and size.1 It is the most common genetic disease affecting the kidneys and leads to terminal kidney failure as patients get into their 40s and 50s.2,3
The leading cause of death in patients with polycystic kidney disease is cardiovascular disease, being arterial hypertension (AHT) its main determinant.4 Both hypertension and the increase in renal size secondary to the growth of cysts1 is correlated with a progressive deterioration of renal funcion in ADPKD. The onset of hypertension in these patients is common and in approximately 60% of cases the diagnosis is performed before any renal function impairment appears. It seems that the increase in kidney size5-7 and the activity in the renin-angiotensin-aldosterone system8-10 are primarily responsible for the development of hypertension in these patients. Studies in patients with ADPKD and normal renal function have shown the presence of target organ damage (increased left ventricular mass)11,12 before developing AHT. This damage appears to be related more to the increase in systolic blood pressure (SBP) determined by ambulatory blood pressure monitoring (ABPM) than to the blood pressure (BP) measured at the clinic.12
Twenty-four hour ABPM adds additional information to the BP measurements in the clinic (BPc) as it reports on the circadian rhythm and the variability of the BP. Furthermore, it identifies patients with masked hypertension (normal clinic BP and high ambulatory BP) and isolated clinic hypertension (high BP readings in the clinic and normal ambulatory BP). A non-physiological BP profile (nondipper nocturnal pattern), a greater BP variability (average of standard deviations over 24 hours greater than 18 mmHg for SBP or greater than 15mmHg for DBP) and the presence of masked or isolated clinic hypertension have been related to greater cardiovascular risk.13-17
Therefore, although hypertension is a key factor in cardiovascular morbidity and mortality in patients with polycystic disease, little is known about the pre-hypertensive stage. In addition, it is not known whether the increase in kidney size could be associated with a change in the BP profile and its variability. We therefore decided to evaluate the following points in patients with normotensive ADPKD a priori and with eGF by MDRD >60 mL/min/1.73 m2:
1. Whether there are differences between the BPc and the ABPM readings.
2. The relationship between maximum kidney diameter and SBP, DBP and mean BP (MBP) over 24 hours, day and night, and pulse pressure (PP) obtained by 24-hour ABPM.
3. If there is a relationship between maximum kidney diameter and the variability of BP or the circadian BP pattern.
MATERIAL AND METHODS
We performed a transversal, observational study that included 37 patients with ADPKD from those who visited outpatient clinics, who were between the ages of 18 and 50 years, with eGF by MDRD >60 mL/min/1.73 m2 and who were normotensive (patients with home BP <135/85 mmHg and not receiving treatment for hypertension).
The following information was collected from these 37 patients:
1. Three readings of SBP and DBP with the OMRON 705 IT blood pressure monitor (Tokyo, Japan), following the standard for BPc readings of the European Society of Hypertension (ESH),18 using the average of three readings as the clinical BP value.
2. ABPM data (via the Dyasis Integra device) (Rueil-Malmaison, France).
- SBP, DBP and MBP (DBP + 1/3 pulse pressure (PP) (PP = SBP – DBP) during the day, night and over 24 hours. Heart rate and 24-hour PP.
- Percentage of nocturnal BP decrease with respect to the daytime SBP, DBP and MBP and quality of sleep on the ABPM date.
- Load index (percentage of BP measurements above the established target BP) for SBP and DBP during the day, night and over 24 hours.
- Typical or standard deviation of the average SBP and DBP during the day, night and over 24 hours. Maximum daytime, nightime and 24-hour SBP and DBP.
3. Anthropometric data: weight, height, body surface area and body mass index.
4. Mean maximum diameter of both kidneys (in millimetres) by renal ultrasound performed by ultrasound specialists who are expert in renovesical ultrasound, using a single measure.
According to the ABPM readings and following the recommendation in the 2007 ESH Guidelines,18 patients are consider normotensive if they present a SBP <130 mmHg and a DBP <80 mmHG by ABPM over 24 hours.
The percentage of decrease in nocturnal MBP versus daytime MBP allows us to classify patients according to their BP profile:
1. Non-dipper pattern: nocturnal MBP decrease versus daytime MBP less than 10%.
2. Dipper pattern: nocturnal MBP decrease versus daytime MBP between 10 and 20%.
3. Riser pattern: nocturnal MBP higher than daytime MBP.
4. Extreme dipper pattern: nocturnal MBP decrease versus daytime MBP greater than 20%. The circadian profile was not assessed if the patient reported suffering from a bad night’s sleep.
Considering the BP readings obtained from the ABPM and the BPc, we can classify the patients into four groups:
1. White coat AHT: patients with high BPc ((>140/90 mmHg) and BP by ABPM over 24 hours <130/80 mmHg.
2. Masked AHT: patients with normal BPc (<140/90 mmHg) and high BP by ABPM over 24 hours ((>130/80 mmHg).
3. True AHT: patients with high BPc and BP by ABPM over 24 hours.
4. True normotensives: patients with normal BPc and BP by ABPM over 24 hours.
The statistical analysis was carried out with the SPSS software. The results are expressed as the mean ± standard deviation (SD) for the continuously distributed variables and as frequencies for the categorical variables.
Given the small sample size, the normal distribution of variables was studied using the Kolmogorov-Smirnov and Shapiro-Wilks tests. After verifying the normality of the variables, the Student’s t-test was used to compare samples with two categories and ANOVA was used for those with three or more categories. For the non-parametric variables, the Mann-Whitney and Kruskall-Wallis tests were used depending on whether they had two or more categories.
To study the association between the mean maximum kidney diameter and the various data provided by the ABPM, the linear Pearson correlation coefficient was used. The distribution of categorical variables was analysed by means of the chi-squared test. A p less than 0.05 was considered statistically significant.
RESULTS
Blood pressure classification according to BP values obtained in the clinic and by ambulatory blood pressure monitoring
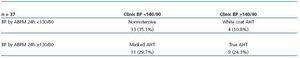
The 37 patients included were classified into four groups according to the BP obtained in the clinic and through 24-hour ABPM. Of these, 13 were true normotensives (35.1%), 9 were true hypertensives (24.3%), 4 patients had white coat hypertension (10.8%) and the remaining 11 (29.7%) had masked hypertension (Table 1).
Taking into account the average BP by ABPM over 24 hours and hypertension being diagnosed for a SBP >130 mmHg or a DBP >80 mmHg, 20 of the 37 patients (54%) initially selected as normotensives according to the home BP readings were diagnosed with AHT.
Relationship between kidney size and blood pressure characteristics
There is currently no standard of normality in relation to maximum kidney diameter in the general population but it is known that the maximum kidney diameter is correlated with height,19 which was coherent with our population (r = 0.572, p = 0.016). The mean maximum diameter was measured for both kidneys of each individual and was adjusted for height.
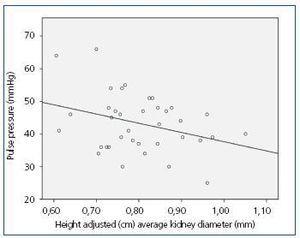
We had set out to only assess normotensive patients with ADPKD but because we had a significant percentage of hypertensive patients, we decided to study whether there was any relationship among the total available population (37 patients) between the various parameters obtained by the ABPM and the mean kidney diameter adjusted for height. This analysis revealed a statistically significant negative correlation between a greater kidney size and a lower PP (r = -0.325, p = 0.05) (Figure 1).
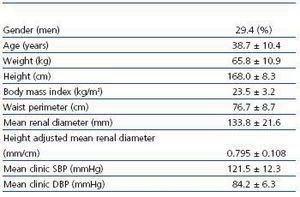
Subsequently and because this was the main objective of the paper, the results in the subset of 17 normotensive patients by ABPM over 24 hours were analysed. Table 2 and Table 3 contain the demographic characteristics, kidney size and BP obtained in the clinic and by ABPM. When analysing the data from the group of the 17 normotensive patients, positive correlations were identified between average maximum kidney size adjusted for height and all parameters of ABPM with the exception of PP, without reaching statistical significance.
Kidney size, circadian profile and blood pressure variability
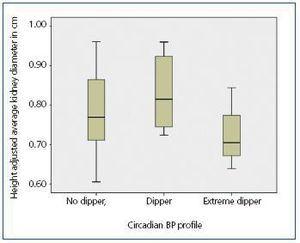
Clinically, the parameter used for assessing the BP pattern was the decrease in daytime to nightime MBP. In the group of 17 normotensive patients, there were no statistically significant differences in the maximum renal diameter adjusted for height between patients with a non-dipper pattern (n = 6), dipper pattern (n = 8) and extremely dipper pattern (n = 3) (p = 0.662) (Figure 2). None of the 17 patients reported a riser pattern.
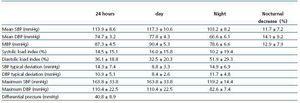
Of the 17 normotensive patients, we decided to study those who had a physiological BP profile, maintaining 11 assessable patients with a dipper BP pattern.
In the group of 11 patients with dipper BP patterns according to the decrease in MBP, positive correlations were found, although not significant, between kidney size and all parameters (SBP, DBP, systolic and diastolic load index, SD of SBP and DBP) for daytime, nightime and 24-hour BP readings by ABPM, where diastolic load index over 24 hours showed the greatest positive correlation (p = 0.07). The nocturnal decrease in BP for this group had a negative correlation, although not statistically significant, with the increase in kidney size.
Since, strictly speaking, a dipper pattern should present a nocturnal decrease in both SBP and DBP greater than 10%, we investigated in the 17 normotensive patients whether the absence of a noctural decrease in SBP and/or DBP was associated with a greater maximum renal diameter adjusted for height. No significant differences were found in kidney size among patients with or without a dipper BP pattern.
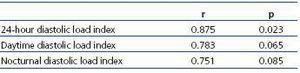
Applying this criterion of a nocturnal SBP and DBP decrease of >10% versus daytime to define the dipper pattern, only 6 of the 17 patients had a dipper pattern, all with a proper night’s rest on the date of the ABPM. In these six patients, a trend was once again observed towards a positive correlation that approached statistical significance for the 24-hour mean DBP, the diastolic load index for day and night, with the 24-hour diastolic load index achieving statistical significance (r = 0.875, p = 0.023) (Table 4).
In the group of 11 patients without a dipper pattern of SBP and DBP, a positive and statistically significant correlation was observed (r = 0.623, p = 0.04) between the maximum kidney diameter adjusted for height and the standard deviation of DBP at night, which once again is a parameter that reflects the BP variability.
DISCUSSION
The ABPM study of this group of patients who reported correct home BP readings allowed us to diagnose some 54.1% of them as hypertensive. The patients were not trained to carry out a proper home blood pressure monitoring (HBPM), which would have helped diagnose hypertension in some of the patients who reported being normotensive at home.
An important aspect of this study is that 11 of the 37 patients selected (29.7%) would not have been diagnosed with hypertension using only the clinical measurements, since they had masked AHT. Some studies have shown that patients with masked hypertension have more important subclinical organ damage than subjects with white coat hypertension or with grade I AHT, which causes this condition to carry a greater cardiovascular risk.15-17 Population studies have also shown a significant increase in mortality in this subset of the population, which might become comparable to the established AHT.18 The prevalence of masked AHT, according to the literature, varies between 6 and 26%. In the population studied, the prevalence of masked hypertension is very important and, if not detected and corrected, it can increase cardiovascular risk and the likelihood of developing target organs damages.
The existence of a statistically significant negative correlation between a greater maximum kidney diameter and a lower PP in the initial group of patients indirectly suggests an alteration of the DBP. The population studied was young, with an average age of approximately 38 years. As with our group, the general hypertensive young population is much more likely to have high DBP than SBP, which leads to a decrease in PP.
In the group of normotensive patients, no relationship was detected between kidney size and the alteration of the circadian BP cycle, although only a few patients were analysed. However, there remains a discernible trend towards a poorer BP profile associated with a poorer DBP to greater kidney diameter. This trend persists even in the group of normotensive patients with proper nocturnal decrease in MBP. The relationship between a greater diastolic load index over 24 hours to greater renal diameter in patients with dipper pattern of SBP and DBP is statistically significant. The load index (percentage of the BP readings by the ABPM that exceed the preset target BP) is one of the measures used for evaluating BP variability and it has been shown that an increased load index is related to greater target organ damage (left ventricular hypertrophy).20 The trend towards increased diastolic load index as kidney size increases could ultimately be related to greater target organ involvement, which has been shown in some studies with this type of population.12
Given the importance of the results obtained in this study, it is necessary to expand the sample size to confirm the findings and to evaluate the possible relationship that these findings may have to subclinical involvement of target organs.
In conclusion, the single reading of BPc in patients with ADPKD and normal renal function leaves many hypertensive patients undiagnosed given the high prevalence of masked AHT. ABPM-assisted examination helps to identify these patients early on.
The analysis of the overall group of 37 patients, as well as the separate analysis of the group of normotensive patients, show a statistically significant relationship between greater renal size and a worse performance of DBP, as revealed by a lower PP in the former group and a greater variability in DBP in the latter group. This data shows a worse DBP profile as compared to SBP. These findings indicate that a relationship might exist along the entire evolution of the disease between renal growth and DBP alteration.
Table 1. Classification of BP according to measurements taken in the clinic and by ABPM
Table 2. Demographic and clinical characteristics of the normotensive population confirmed by 24-hour ABPM (n = 17)
Table 3. BP readings by ABPM of the normotensive population (n = 17)
Table 4. Study of the relationship between average renal diameter adjusted for height and the variability of BP in the group of normotensives with a dipper pattern of SBP and DBP (n = 6)
Figure 1. Linear regression line between height adjusted average renal diameter and pressure differential in the overall population (n = 37).
Figure 2. Height adjusted average renal diameter as a function of the circadian BP profile in the normotensive group (n = 17).