Introducción: La edad y las comorbilidades asociadas de muchos pacientes en hemodiálisis dificultan su autonomía funcional. Nuestros objetivos fueron conocer el grado de dependencia de las personas en hemodiálisis (HD) según criterios de la Ley sobre Promoción de la Autonomía Personal y Atención a las personas en situación de dependencia o Ley de Dependencia (LD) y su asociación con la mortalidad a tres años. Método: Estudio descriptivo transversal, realizado entre octubre de 2007 y enero de 2008. De 3702 pacientes de 40 unidades de Cataluña se seleccionó como posibles dependientes a 806, según el criterio del personal sanitario que los atendía. Se valoraron: grado de dependencia según los criterios de la LD, edad, tiempo en HD, patología asociada, características del tratamiento, situación familiar y supervivencia de 2009 a 2011. Resultados: Según la LD, no presentaban dependencia 137 pacientes, 350 presentaban dependencia de grado 1; 237 de grado 2, y 82 de grado 3. Residían en una institución 121. La media de edad fue de 74,9 ± 18,2 años y la mediana del tiempo en diálisis, de 36 meses. Destaca la prevalencia de diabetes (35,7%) y enfermedad cardiovascular (29,1%); las alteraciones musculoesqueléticas (87%) y neurológicas (38%) fueron las principales causas de dependencia. Eran portadores de catéter como acceso vascular el 64,2%. El 34,9% de los pacientes sobrevivieron a los 3 años, presentando menor grado de dependencia del que tenían los fallecidos antes del óbito, sin que existieran diferencias en el grado de dependencia entre los fallecidos en el primer, segundo o tercer año de supervivencia. Conclusiones: Según la LD, la prevalencia de pacientes con dependencia es elevada en Cataluña (18,07%). Estos pacientes presentan una elevada mortalidad a los 3 años.
Introduction: Age and the comorbidities associated with ESRD impair the functional autonomy of patients on haemodialysis (HD). Our objectives were to assess the level of dependence in patients on HD and their mortality rates after three years of treatment. To do so, we followed the criteria established by the "Ley de Promoción de la Autonomía Personal y Atención a las Personas en situación de dependencia", the Spanish Law of Dependence (LD). Methods: We carried out a cross-sectional descriptive study between October 2007 and January 2008. From 3702 patients in 40 dialysis units in Catalonia, 806 were selected as potential dependent individuals according to the criteria of their healthcare providers. Variables studied included: level of dependence according to the LD criteria, age, time on HD, associated pathology, treatment characteristics, family circumstances, and survival from 2009 to 2011. Results: According to the LD, 137 were not dependent, 350 had a grade 1 dependence level, 237 grade 2, and 82 grade 3. In addition, 121 were living in an institution. The mean age was 74.9±18.2 years and the median time on HD was 36 months. The prevalence of common pathologies was: diabetes (35.7%) and cardiovascular disease (29.1%). Musculoskeletal alterations (87%) and neurological disorders (38%) were the main causes of dependence. 64.2% of patients had a catheter as a vascular access. 34.9% of patients survived after three years, and these had a lower level of dependence when compared to those patients who had died, with no statistically significant differences within those three years. Conclusions: According to the LD, the prevalence of dependent patients in Catalonia is substantial (18.07%). These patients have a high mortality rate after three years.
INTRODUCTION
Evaluating the level of dependence in patients on haemodialysis (HD) has been the subject of interest for several authors, since current profiles of this population, namely elderly patients with substantial associated pathologies, not only have direct implications on mortality and morbidity rates, but can also fundamentally affect other functional aspects, such as the quantity and quality of the health care required and the structure of dialysis units needed in order to provide proper care.1-3
Dependence can be understood as the result of a process that commences with the appearance of a deficit in body functioning as a consequence of disease or trauma.4 This deficit implies a limitation for the individual that, when adaptation to the environment is insufficient for compensating for the limitation, necessitates the assistance of other people in order to carry out daily activities, namely the patient’s family and social services, with consequent personal and economic costs that have consistently been deficiently provided.5-6 One of the primary initiatives to combat this deficiency was the establishment of law 39/2006, the Law of Dependence (LD) (Ley de Promoción de la Autonomía Personal y Atención a las personas en situación de dependencia),7 which was the source of a great deal of debate. Currently, this law continues to be the source of major controversy due to the difficulties in applying it, to the point where serious doubts have been raised regarding its viability.8 Even so, today it remains as the framework that legally determines the level of dependence that allows for patients to access social services and any form of assistance outlined in its text. According to the census of dependence, almost 250 000 people were in a situation of dependence in 2011, and the provision of social and health care required an enormous amount of organisation and resources in terms of prevention, diagnosis, and treatment.9 Dependence implies a serious challenge for dialysis units, since it is an incontrovertible fact that the number of dependent patients that will be treated in these units is on the rise.10-12
On the other hand, the dependence of renal patients is also defined by certain social characteristics and limitations that have traditionally been evaluated in nephrology departments using scales such as the Barthel or Delta test.13-15 Dependence in these patients will not only influence quality of life, but can also be associated with morbidity/mortality rates and thus be an important predictor of survival.16 The LD facilitates the use of a single, unified vocabulary for the evaluation of dependence through the use of a self-established dependence scale,17 which, while based on these same tests, presents unique characteristics that are specifically designed to provide a different evaluation than those produced by other instruments.18 As such, it would appear logical that clinical registries should include the criteria of the LD to assign levels of dependence to each patient. Currently, we do not have information regarding the prevalence and grade of dependence according to the LD criteria in patients on haemodialysis in Spain.
The objectives of our study were: a) to evaluate the level of dependence in patients on HD in Catalonia according to the LD criteria, and b) to analyse the evolution of mortality in these patients in relation to the level of dependence.
MATERIAL AND METHOD
We carried out our study in 40 of the 42 adult dialysis units in Catalonia. Our study was descriptive and cross-sectional, and was carried out in two phases: the first (October 2007-January 2008) involved the collection of data regarding the grade of dependence in patients on HD as a renal replacement therapy in Catalonia, as well as other clinical and sociodemographic variables. The second phase (2009-2011) involved a yearly compilation of survival results for those patients initially interviewed in the first phase.
Our sampling design was non-probabilistic and by convenience, since out of the total population of 3702 patients on dialysis in the 42 participating centres, we used the following inclusion criteria to choose patients for our study: patients receiving HD as a renal replacement therapy in any of the 44 dialysis centres in Catalonia, age >18 years, and considered as “dependent” by the healthcare providers (doctors and nurses). Conversely, we excluded those patients categorised as “non-dependent.” Healthcare providers classified patients as “dependent” or “non-dependent” based on whether these, during their stay at the dialysis centre, required assistance in order to carry out basic activities of daily living (BADL), such as dressing and mobility. In order to ensure that the selection of these patients was correct, we used the LD scale to evaluate a sample of “non-dependent” patients, which produced satisfactory results and the conclusion that the classification system was appropriate and did not exclude patients that were in fact dependent.
The study variables included: level of dependence and its relationship to sociodemographic variables (age, sex, level of study, and marital status), information regarding the patient’s caretaker (age, relation to the patient, perception of the caretaker’s health according to the patient), and clinical information regarding the HD treatment (associated pathologies, hospitalisations in the last year, time on dialysis, duration of treatments, and type of vascular access). Mortality and its relationship to level of dependence were evaluated after the first, second, and third years of follow-up.
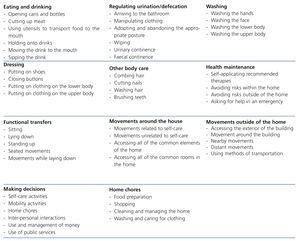
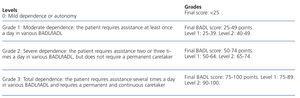
The first phase of field work took place between October 2007 and January 2008. Information was obtained from clinical histories, and a single researcher observed each patient prior to, during, and after the HD session in order to evaluate the dependence of each patient in carrying out BADL such as walking, eating, drinking, and dressing, in addition to compliance with an ad-hoc questionnaire, the reliability and validity of which was tested prior to the study with a test-retest and pilot test analysis. In order to evaluate the level of dependence, we used the dependence scale proposed by the LD without modification.17 This scale was inspired by the instruments normally used in clinical practice, such as the Barthel scale13 and the Lawton test,15 and is composed of items that classify levels of personal autonomy and the need for supervision and/or support for basic activities (Table 1). The BADL include: feeding, continence, mobility, going to the bathroom, dressing, and bathing17; and instrumental activities of daily living (IADL) include: capacity for using the telephone, shopping, preparing food, taking care of the house, washing the clothes, using transportation, responsibility for medication, and economic maintenance,19 which determines the grade of dependence of the patient in question on a scale of 100, defining the patient as dependent or not using a scale of grades and levels (Table 2). The technique used for ensuring compliance with the questionnaire was a personal interview carried out by the researcher with each patient included in the study. In patients that were unable to answer the questionnaire, the interview was held with someone close to the patient, primarily nurses or caretakers. The second phase of the study was carried out from January 2009 to January 2011, and involved yearly consultations with those responsible for the treatment of each patient in order to register the survival of the patients evaluated in the first phase.
We used SPSS statistical software, version 19, for all data analyses. In the descriptive statistical analysis, we used frequency tables, mean, median, mode, standard error, and standard deviation to describe the study variables. We calculated Spearman’s Rho to evaluate the possible association between numerical variables, and used the Mann-Whitney test to compare percentages. Other aspects that related mortality to dependence and other clinical variables were compared using the Kruskal-Wallis test, Kendall’s Tau, Gamma coefficient, and chi-square test. We considered a P-value of <.05 to be statistically significant.
The study was approved by the Human Research Ethics Committee of the Universitat Internacional de Catalunya. We also acquired informed consent from the patients or their family members when patients were unable to respond to the interview.
The study was also approved by the Renal Patient Registry of Catalonia (Registre de Malalts Renals de Catalunya [RMRC]), a division of the Health Institute of Catalonia, who then presented a letter to all dialysis centres in Catalonia, informing them of the study and the participating institutions, as well as the objectives of our research and what it would mean to participate in it.
RESULTS
Patient characteristics
Of the 810 patients selected, 4 did not wish to be interviewed, leaving us with a final sample size of 806 patients. Of these, 67 were unable to respond to the questionnaire for themselves, due to severe cognitive deterioration, and so their attending nurses (n=36) or family members (n=21) were interviewed.
A total of 425 patients (52.7%) were men and 381 (47.3%) were women, and 604 (74.5%) were 70 years of age or older. In addition, 15.1% of patients (n=121) lived in health institutions, 53% (n=427) lived with their spouse, 35.4% (n=285) were widowed or separated, 10.9% (n=88) were single, and 80.1% (n=635) had one or more children. Finally, 77.4% (n=624) were employed in unskilled or manual labour; 65.4% reported that they had no education or only primary education.
As regards patient care, 64.5% (n=520) were cared for by close family (spouse/children), 24.9% (n=201) were looked after by formal caretakers, and 1.55% (n=11) were not cared for by anyone (all of which were considered non-dependent according to the LD). The mean age of patient caretakers was 66±13.1 years. When the patients were asked to evaluate the state of health of their caretakers, 40.3% said good (n=325), 20.2% said average (n=163), and 9.3% said bad (n=75).
Level of dependence and clinical characteristics
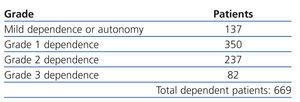
Table 3 shows the results regarding patient dependence. The aspects evaluated by the LD scale showed that the primary causes of dependence were correlated with mobility; in this context, 82% of patients with grade 2 dependence and 74.5% with grade 1 dependence required a wheelchair or cane to move about. All patients with grade 2 dependence required assistance in daily activities such as eating, dressing, personal hygiene, leaving the house, and performing domestic chores, and 67.8% required assistance in making decisions. Patients with grade 3 dependence were totally dependent in all activities of daily life, and only 16% were capable of making decisions, since 66 patients in this group had a cognitive deficit.
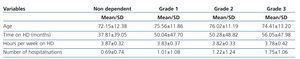
We used the Kruskal-Wallis test to examine whether differences existed between groups of grade 1, 2, and 3 dependence and independent variables (age, time on HD, hours per week on HD, and number of hospitalisations), which revealed significant differences in terms of age (P=.017): patients in dependence groups 1 and 2 were older on average than non-dependent patients; however, there were not enough group 3 patients in order to observe significant differences as compared to the other 3 groups; b) time on haemodialysis (P=.002): non-dependent patients had less time on treatment than others; and c) number of hospitalisations (P<.0001), as higher grades of dependence were correlated with increased hospitalisations. In contrast, we did not observe significant differences in terms of hours per week on HD between the different groups of dependence (P=.209). Table 4 displays the means and standard deviations of the study variables.
Patients received dialysis through a conventional internal fistula or prosthesis in 518 cases, and 286 used a catheter, with catheters being more common in more dependent patients; 136 patients in non-dependent groups or grade 1 dependence vs. 150 in groups of dependence grades 2 and 3 (χ2, P=.001).
Upon comparing patients that have one single vascular access with those that have had more, we did not observe any significant differences (Mann-Whitney Z=1.264; P=.206).
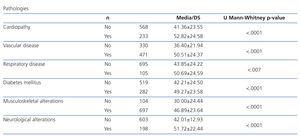
The pathologies found in our patients are summarised in Table 5. For each pathology, we performed a Mann-Whitney U-test to compare the means of dependence scores between patients that suffer each pathology and all others, and the results were significant in all: suffering a pathology increases the level of dependence as compared to those that do not suffer it (P=.0001).
Mortality after 1, 2, and 3 years and the relationship with grade of dependence
During the three year study-period following the initial study, 489 patients died. Of the 315 that were still alive, 12 received transplants and had a functioning renal graft (of these, 8 had mild dependence or autonomy at the moment of the study, and 4 had grade 1 dependence). The relationship between mortality and dependence was significant (Mann-Whitney Z=-5.011 and P=0), and those with a higher grade of dependence had higher mortality during follow-up (Figure 1).
Upon comparing the level of dependence between patients that died during the first, second, and third years, the differences were not significant (P=.946).
DISCUSSION
The results of our study demonstrate a high prevalence of dependence among patients on haemodialysis in Catalonia, based on the criteria of the new LD. We also observed a high rate of mortality after 3 years in this population, with a positive correlation between mortality and level of dependence. The extensive collaboration in our research, including both the dialysis centres (40 of 42 in Catalonia) and patients (only 4 patients declined participation), yielded a very representative sample that is comparable to the results from the RMRC.20 In addition, the use of a single researcher dedicated to this task guaranteed the homogeneity of the sample.21,22
Upon comparison of the demographic characteristics of our sample with those from the registry, our sample has a higher percentage of women than in the general population on HD (47.3% vs. 37.5%); this finding coincides with the results from studies in the general population showing greater dependence in women. As in the general population, dependent patients on HD are often older than 70 years.23
Fewer patients (53%) lived with their spouse than in the overall group of patients on HD, according to the RMRC value (61.7%).20 In a similar manner, more patients were institutionalised (15% vs. 3% in the RMRC). The need for assistance in these patients often explains the inability of spouses/family members to provide care, leaving this responsibility for a professional caretaker (24.9% vs. 14% in the RMRC). The fact that the vast majority of dependent patients were elderly and that very few patients were cared for in a family setting with employment outside of the home in the productive age explains why family member caretakers are older and often have deteriorated health. This result is also in accordance with the results from studies in the general population.23 The only patients that did not have any assistance (11) had a score lower than 25 (mild dependence or autonomy) in the LD scale.
A total of 77.4% (n=624) of the patients in our study worked in unskilled/manual labour; in addition, 65.4% reported that they had no education or only primary education. The level of education coincided with the data from the RMRC, since 70% of people older than 65 years had only primary studies.20
There is a certain level of over-estimation of patient dependence on the part of the healthcare personnel: we observed a discrepancy between the subjective evaluation of dependence by healthcare professionals and the objective score produced by the LD criteria, since 18% of patients considered dependent by healthcare professionals were not dependent or had a very mild dependence according to the LD criteria. This fact is probably due to the healthcare professionals’ evaluation of clinical aspects that are unrelated to dependence and their evaluation of patients in concrete situations (hospitalisations at the end of treatment), and the fact that patients feel more vulnerable in the HD centre, which tends to magnify their deficits. We must also consider the restrictive philosophy of the LD, since the notable associated socioeconomic costs imply that the benefits should only go to very clear cases of dependence. Both circumstances can explain why studies involving patients on dialysis that use other classification scales result in much higher rates of dependence.1-3
As has been observed in other studies, dependence in these patients is produced primarily by alterations to the musculoskeletal system, which hampers proper mobility and necessitates assistance in activities in the dialysis centre such as eating, dressing, or laying/sitting down in the dialysis bed/chair. In addition, our study detected, as other authors have as well, that many of these patients have a notable mental deficiency. In this context, elderly patients on haemodialysis have a high prevalence of cognitive alterations, which can be 7.4 times higher than in elderly individuals in the general population. This appears to be closely related to the advanced atherosclerosis observed in these patients.24-26
As in previous studies, we observed a significant correlation between time on HD and level of dependence,1-3 and although we might assume that patients that have been on dialysis for a longer time are in worse physical condition. In fact, many patients with several years on HD were young and in good physical condition when they started treatment, whereas currently, elderly patients with a more deteriorated physical state are being included in HD programmes.1,2,10
Dependence does not appear to influence the appropriateness of intensifying dialytic treatment, and although the available evidence would advise an increase in the hours and/or frequency of haemodialysis sessions in labile or pathological patients,27,28 in our study, the vast majority of patients in our sample received 12 hours or less of treatment per week.
The use of a catheter as a vascular access was much higher in these patients than in those of the RMRC, with a greater rate of use in patients with greater dependence; this may be due to the worse state of the vascular system, older age, greater comorbidity, or lower life expectancy, which impedes or hinders the creation of a conventional arteriovenous fistula.29,30 Patients with catheters have greater difficulty in carrying out basic activities, especially those related to personal hygiene, which is especially relevant in these dependent patients which, if also suffering from cognitive deterioration, may compromise catheter survival due to inadequate care, requiring caretakers to adopt greater precautions for proper maintenance.30
The pathologies observed in dependent patients comprise a good deal of the comorbidity found in patients in dialysis units, and are the most representative of diseases that cause dependence in the general population, particularly in the form of musculoskeletal alterations. On the other hand, cognitive deterioration, which is one of the primary causes of dependence in our study, was lower than in the dependent general population.26
One indicator of morbidity is the number of hospitalisations, and although the study group had a high number of hospitalisations in the 12 months prior to the study, only 10% of patients were hospitalised three or more times, whereas 274 were not hospitalised on any occasion, with a similar rate of hospitalisations to that of all patients; as such, dependence appears to produce increased need for hospitalisation only in severely dependent patients.10
Although patients with a higher grade of dependence have a lower survival rate than non-dependent patients, deaths in the first, second, and third years of the study were similar in dependent/non-dependent patients. As such, we would expect that the rate of dependence of any grade in patients on HD programmes will remain constant in the near future as long as the inclusion criteria for this type of treatment do not change, since the current trend is to incorporate new patients into HD that are elderly or have associated pathologies that create a situation of dependence.2,10
The high prevalence of dependence among haemodialysis patients in Catalonia requires considering the complex profile of HD patients when planning how dialysis treatment is provided and the conditions in HD units, as well as the fact that dependence creates substantial workloads for healthcare providers, since these patients require greater care during HD sessions and outside of treatment. In general, this is not taken into account or given value when allocating resources for these units.3 In addition, the provision of limited resources to patients with more deteriorated health implies a notable physical and emotional strain.
In the current financial crisis of health care, it is difficult to see how the social and health-related needs of dependent patients on HD programmes can be resolved, since healthcare professionals and caretakers must not only provide high-quality dialytic care, but also special attention for the personal needs of each patient, which implies an important cost that occurs in any group of dependent patients and that the LD does not appear to be capable of defraying.31
In conclusion, the haemodialysis centres in Catalonia are attending to a significant proportion of patients with substantial dependence, which implies a greater workload for healthcare professionals and requires more intensive care and assistance in basic daily activities during HD treatment. The mortality rate in these patients, while higher than in the general population on HD, implies that the continuation of surviving dependent patients, along with the inclusion of new dependent patients on treatment programmes, will produce the situation in which the provision of care to these patients will continue to be an important issue in the near future. An evaluation metric established by law and used unanimously throughout the country would be a useful tool for assessing the level of dependence in these patients.
Study limitations
We did not administer direct interviews to 67 patients; the data for these cases were obtained from patient caretakers. However, the bias produced by this situation is minimal, since these patients were all severely dependent.
Although we performed a pilot study in order to rule out the possibility that dependent patients would be excluded from the study, which produced positive results, we cannot completely rule out that some dependent patients were not included, although it would seem improbable since healthcare personnel tended to overestimate dependence.
We also did not monitor the evolution of dependence over the three year follow-up period; we only followed the survival of those patients interviewed. It would be interesting to analyse these data, since it would be logical that a notable deterioration could be observed during this period.
Acknowledgements
We would like to thank the Monitoring Committee of the Renal Patient Registry of Catalonia, who supported this project. In addition, we would like to thank the participating dialysis centres*, the patients, and the healthcare professionals, in particular María Paz Sorribes, for their collaboration.
* Centre de Diàlisi Bonanova; Centre de Diàlisi Nephros; Centre de Diàlisi Verdum; Centre de Diàlisi Verge de Montserrat; Consorci Hospitalari del Parc Taulí; Centre Hospitalari-Unitat Coronària de Manresa; Centre Nefrològic Baix Llobregat; Centre Nefrològic de Mataró; CETIRSA Barcelona; CETIRSA Terrassa; Clínica Girona; Clínica Secretari Coloma; Clínica Renal Tefnut, SA; Fundació Sanitària d’Igualada Fundació Privada; Fundació Hospital Comarcal de Sant Antoni Abat; Fundació Puigvert; Hospital de Terrassa; Hospital Universitari de Bellvitge; Hospital de Vic; Hospital Clínic i Provincial de Barcelona; Hospital de Figueres; Hospital Universitari de Girona Dr. Josep Trueta; Hospital Dos de Maig; Hospital de Mollet; Hospital de Palamós; Hospital de Puigcerdà; Hospital Sant Bernabé de Berga; Hospital de la Santa Creu de Tortosa; Hospital Universitari de Lleida Arnau de Vilanova; Hospital de Sant Pau i Santa Tecla; Hospital Universitari de Tarragona Joan XXIII; Hospital del Mar; Hospital Universitari General Vall d’Hebron; Hospitalet Medical; Institut Mèdic Barcelona; Institut Nefrològic de Barcelona-Diagonal; Institut Nefrològic de Barcelona-Jules Verne; Institut Nefrològic de Granollers; Pius Hospital de Valls; Reus Medical; Sistemes Renals.
This study was financed by the FIS, project No. PI08/90011.
Conflicts of interest
The authors have no conflicts of interest to declare.
Table 1. Activities evaluated in the Spanish Law of Dependence scale
Table 2. Level of personal autonomy according to the dependence scale
Table 3. Level of dependence according to the dependence scale
Table 4. Level of dependence according to age and dialytic treatment variables
Table 5. Relationship between different pathologies and mean dependence scores
Figure 1. Level of dependence between groups of patients (alive and dead)